Preparing for surgery can feel overwhelming, but having clear instructions can make the process much smoother. It's essential to familiarize yourself with the pre-operative steps to ensure everything goes as planned, from dietary guidelines to medication adjustments. Understanding what to expect will not only ease your mind but also help you recover faster post-surgery. So, grab a cup of tea and let's dive into the essential preparation tips that will set you up for success!
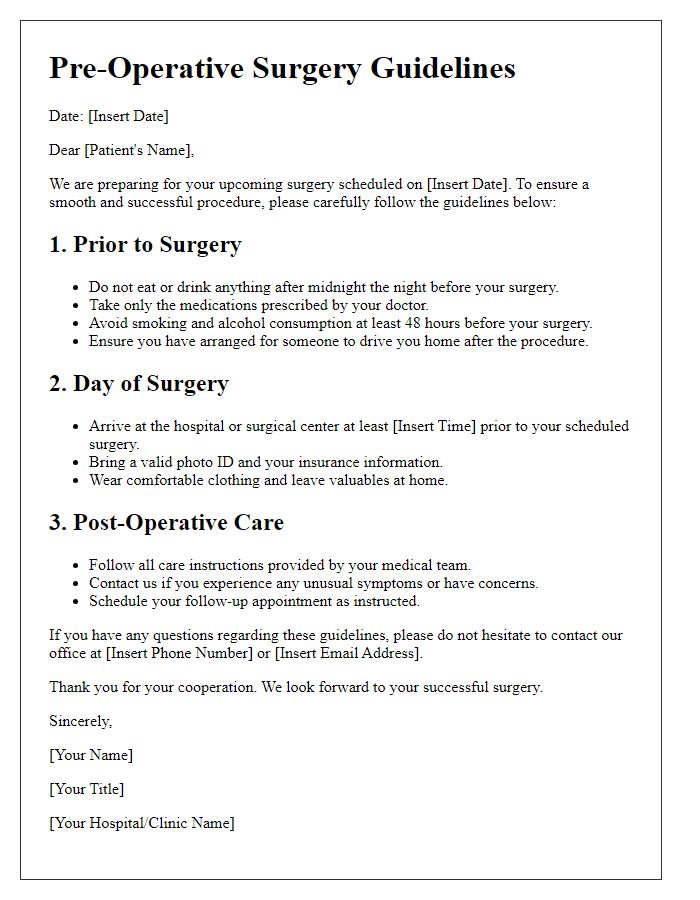
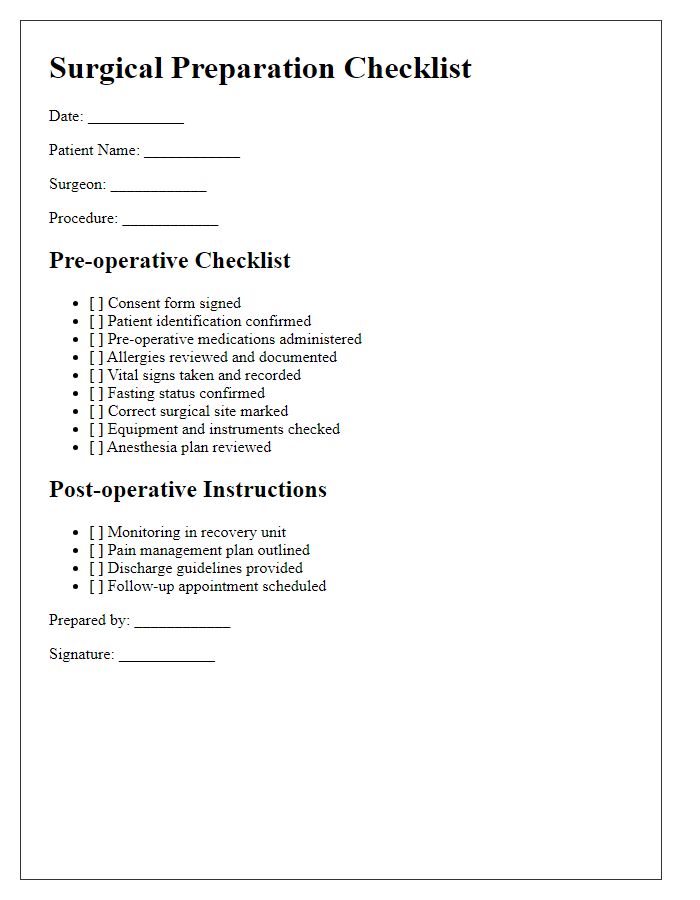
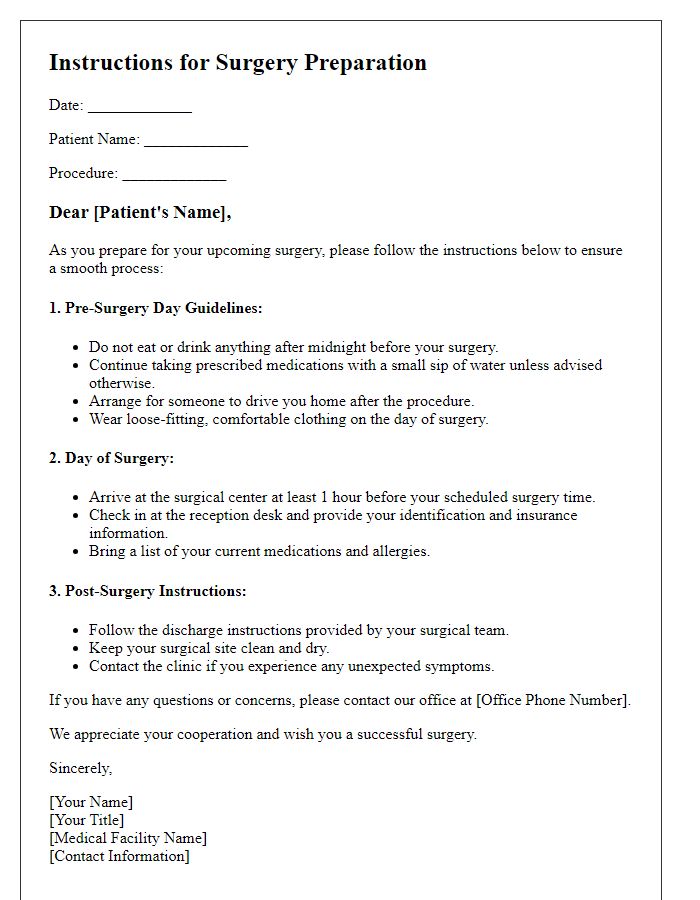
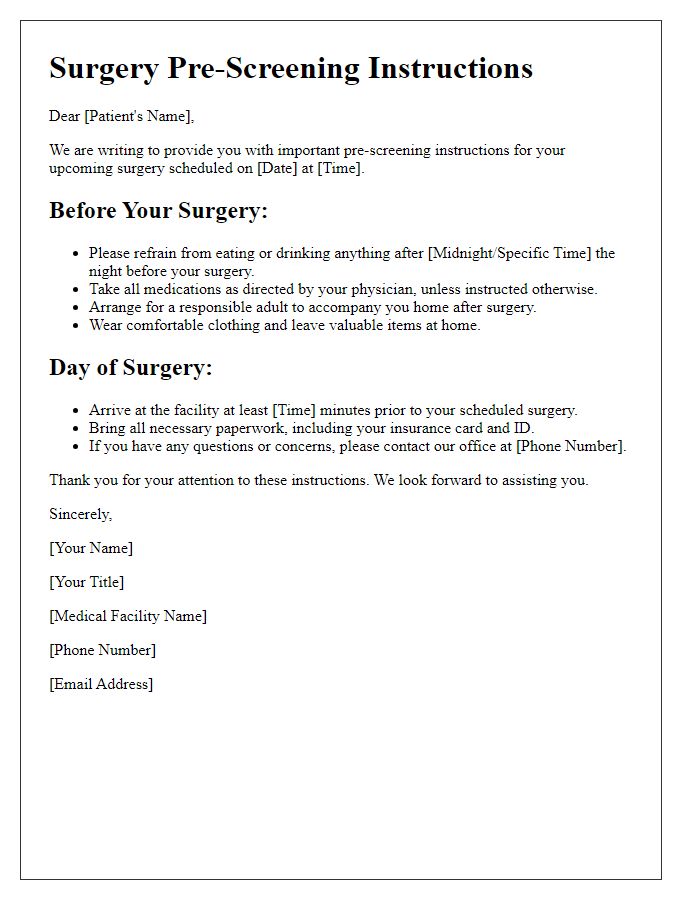
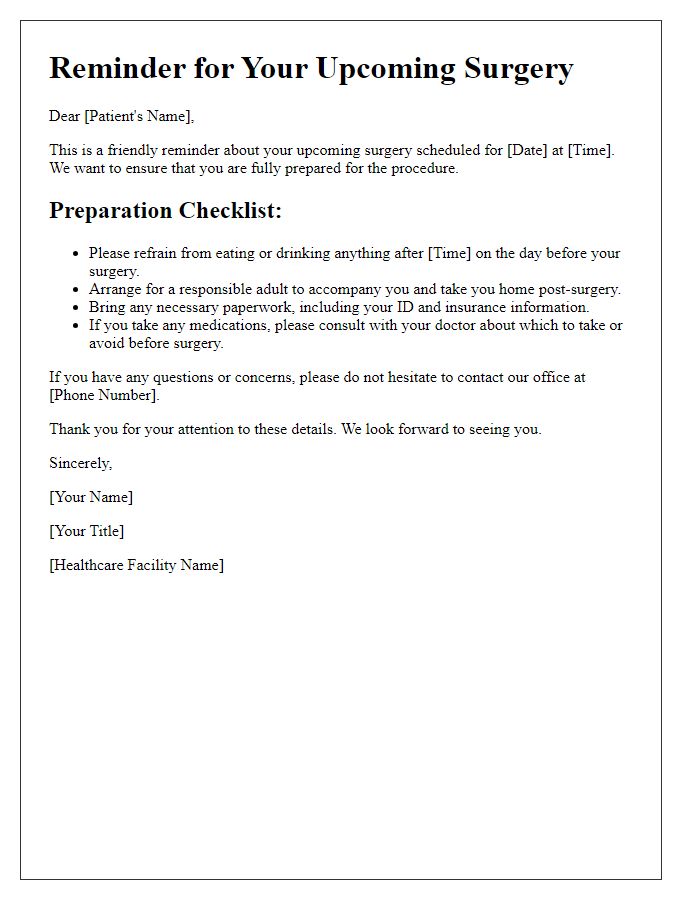
Pre-Operative Instructions
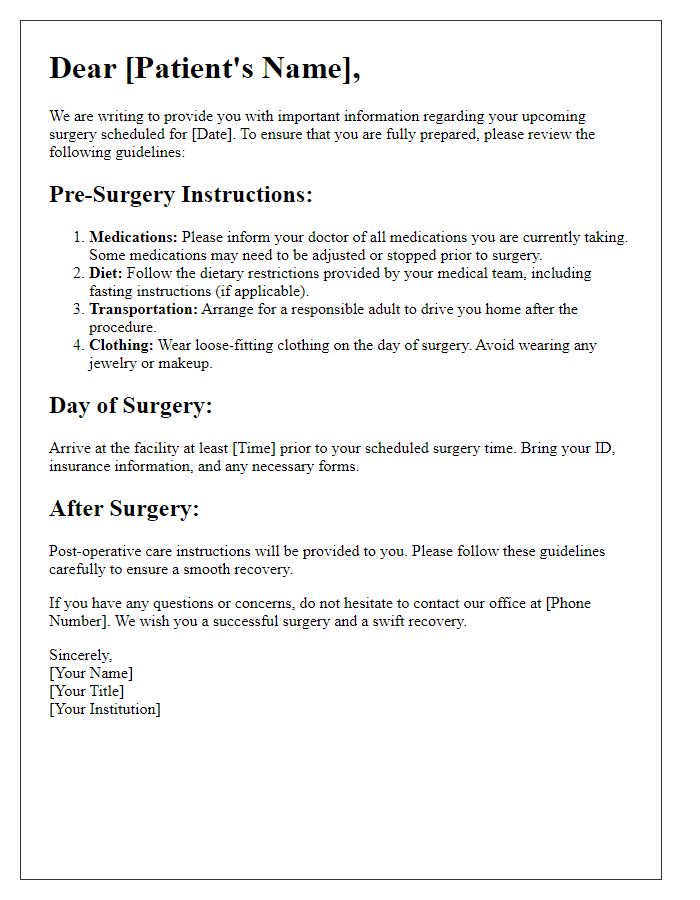
Pre-operative instructions are crucial for ensuring a smooth surgical process. Patients should review essential guidelines leading up to their procedure. Fasting is typically required for at least eight hours before surgery to minimize the risk of aspiration under anesthesia. Medications should be discussed with a healthcare provider (such as a surgeon or anesthesiologist), particularly blood thinners which could complicate the surgery. Medical history, including allergies and previous surgeries, must be communicated clearly during pre-operative consultations. Arranging for a responsible adult (like a family member or friend) to provide transportation home post-surgery is necessary due to anesthesia-related impairments. On the day of the procedure, wearing loose-fitting clothing and avoiding makeup can facilitate easier monitoring and reduce infection risks at the surgical site. Compliance with these instructions (August 2023 Standards) can significantly impact recovery and surgical outcomes.
Medication Guidelines
Pre-operative medication guidelines are essential for surgical success and patient safety. Patients scheduled for surgery should review their current medications, including prescriptions, over-the-counter drugs, and supplements. Specific medications such as blood thinners (e.g., Warfarin, Aspirin) must be discontinued (typically 5-7 days before surgery) to minimize bleeding risks. Nonsteroidal anti-inflammatory drugs, including Ibuprofen (Advil) and Naproxen (Aleve), should also be avoided for at least a week to reduce potential complications. Adequate hydration prior to surgery is crucial, but patients may be instructed to abstain from food and drink for specified hours (usually 8 hours) before surgery to prevent aspiration. Following surgeon's directions regarding diabetes medications (e.g., Metformin, Insulin) is critical as dosage adjustments may be necessary. Maintaining clear communication about all medications with the surgical team can facilitate a safe and effective surgical experience.
Dietary Restrictions
Surgery preparation includes important dietary restrictions to ensure patient safety and optimal outcomes. Two days prior to surgery, patients must avoid solid foods, opting instead for clear liquids such as broth or gelatin. Specific beverages like water, apple juice, and tea without milk are permitted. On the eve of surgery, a total fasting period begins at midnight, prohibiting all food and drink intake. In some cases, doctors may allow sips of water to take essential medications. Adhering to these guidelines, established by medical teams at leading hospitals like the Mayo Clinic and Johns Hopkins, significantly reduces risks of complications during and after the procedure.
Arrival and Check-In Procedures
Proper arrival and check-in procedures are essential for successful surgery preparation. Patients should arrive at the designated surgical center, such as St. Mary's Hospital, at least two hours prior to their scheduled procedure, ensuring ample time for registration and pre-operative assessments. Check-in should occur at the main reception area, where staff will verify personal information, including name, date of birth, and procedure details, to confirm patient identity. Required documents, such as insurance cards, identification, and previous medical records, must be presented. Patients will receive an informational packet detailing pre-surgical guidelines, including fasting requirements, medication instructions, and attire recommendations. After check-in, patients typically undergo preliminary evaluations, including vital sign measurements and reviews of medical histories, to ensure suitability for anesthesia and surgery.
Post-Operative Care Expectations
Post-operative care expectations play a crucial role in recovery following surgical procedures, such as knee arthroscopy performed at specialized outpatient clinics. After surgery, patients can anticipate experiencing varying levels of discomfort, typically rated on a scale from 1 to 10, with effective pain management strategies involving analgesics like acetaminophen or ibuprofen. Surgical sites must be kept clean and dry; instructions will often highlight the importance of changing dressings every 48 hours or as advised by healthcare professionals. Mobility may be restricted, and physical therapy sessions involving targeted exercises are usually scheduled within a week to promote healing and regain strength. Patients should also monitor for any signs of complications, such as increased swelling, redness, or unexpected discharge, with immediate communication to their surgical team necessary if these occur. Furthermore, hydration and balanced nutrition are emphasized for optimal recovery, often featuring vitamins essential for wound healing, such as Vitamin C and Zinc.


Comments