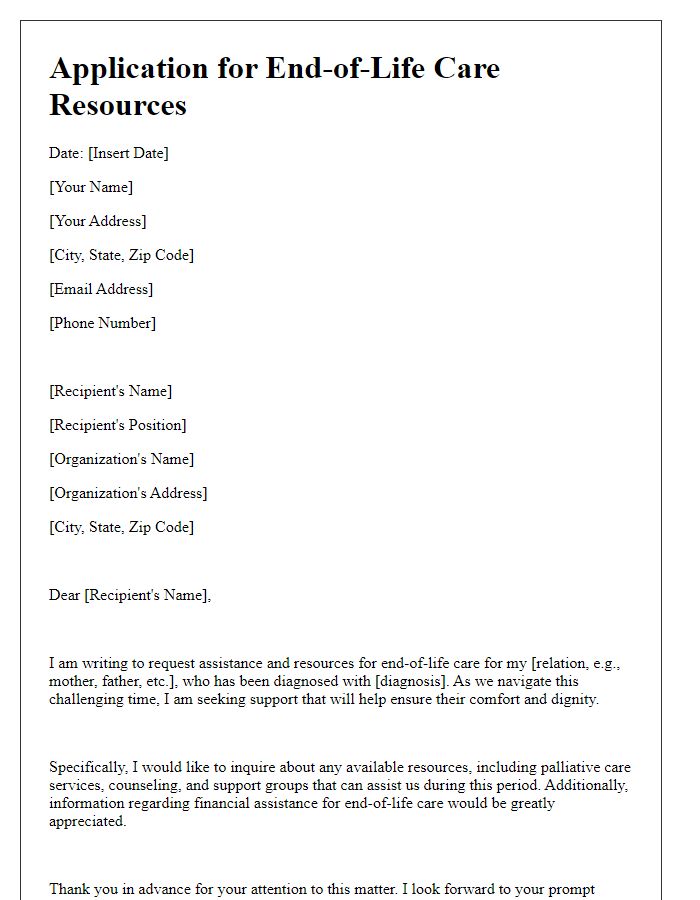
Writing a letter to request end-of-life care plans can feel daunting, but it's an important step in ensuring that your wishes are respected and understood by your healthcare team. It's a chance to communicate your desires for care in a compassionate manner, addressing both your medical needs and personal values. By outlining your preferences now, you can foster peace of mind for both yourself and your loved ones. Ready to learn how to draft the perfect letter? Let's dive in!
Personal Information and Identification
End-of-life care plans are essential documents that ensure individuals receive the necessary support during their final stage of life. These plans often include personal information such as the individual's full name, date of birth, and medical history. Identification documents like a government-issued photo ID or health insurance card are crucial for verifying the person's identity and eligibility for care services. Additionally, important details concerning current medications, specific medical conditions, and preferred medical interventions should be documented. Establishing a discussion with healthcare providers in facilities such as hospice or palliative care units can further enhance the effectiveness of these care plans, ensuring they reflect the individual's wishes and cultural beliefs.
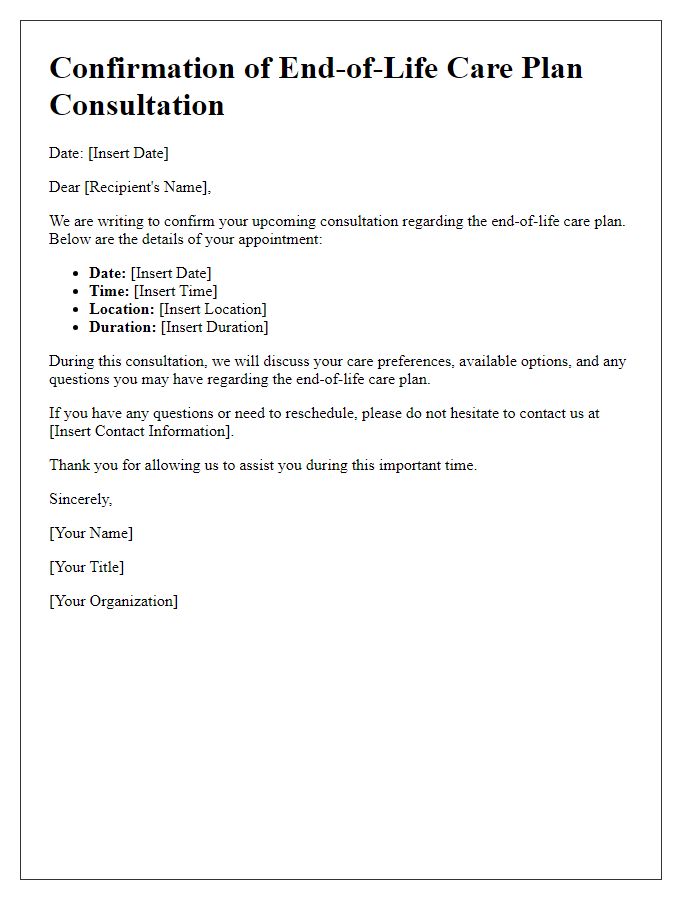
Detailed Medical History and Current Health Status
End-of-life care plans are essential for ensuring comfort and dignity during a person's final days. A comprehensive medical history includes significant diagnoses, treatments, and medications. For example, chronic conditions like heart failure or late-stage cancer must be clearly documented. Current health status involves recent assessments, including vital signs, mobility levels, and mental health evaluation. Specific details, such as nutritional needs and pain management strategies, play crucial roles in effective care planning. Accessibility to healthcare professionals, such as palliative care teams, ensures a holistic approach to support the patient and their family during this critical time.
Specific End-of-Life Care Preferences
End-of-life care preferences are essential for ensuring dignity and comfort during a vulnerable time. Individuals should outline their specific desires regarding medical interventions, palliative care options, and preferred settings, which may include home environments or hospice facilities. Decisions may encompass preferences for pain management methods, such as opioid medications, and the extent of life-sustaining treatments, like mechanical ventilation or resuscitation efforts. It's crucial to document these preferences with clarity, providing contact information for designated healthcare proxies or family members, ensuring that personal wishes are respected by healthcare providers in facilities like hospitals or hospice care centers. tnZym hdhh lrGbt ymkn 'n ys`d fy tkhfyf lDGT `n l`y'lt 'thn tkhdhhm qrrt S`b@ fy l'wqt lHrj@.
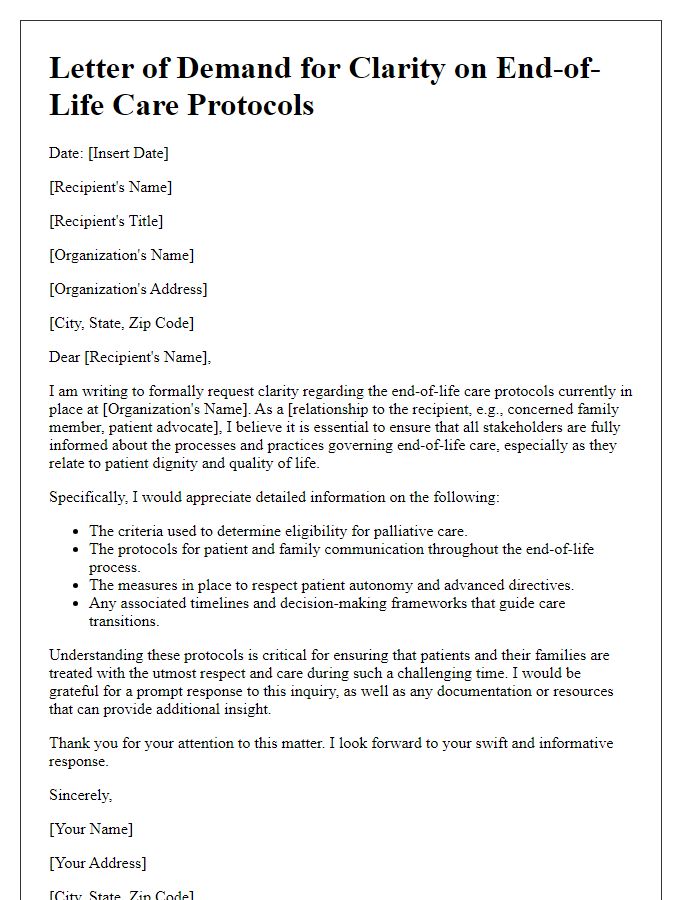
Legal Documentation and Authorization
End-of-life care plans are crucial documents outlining the preferences and medical wishes of individuals facing terminal illness or advanced aging. These plans encompass various aspects such as resuscitation preferences, pain management strategies, and hospice care arrangements. Legal documentation, including advance directives and power of attorney forms, ensures that healthcare providers honor these preferences. Revered institutions like the National Hospice and Palliative Care Organization (NHPCO) provide guidelines for creating these plans. Authorization for end-of-life care often requires signatures from healthcare proxies and witnesses, ensuring clarity and adherence to the individual's choices. Understanding local laws, such as those in California's End of Life Option Act, is essential for a legally binding plan.
Contact Information for Healthcare Proxy or Representative
End-of-life care plans are essential for ensuring that patients' wishes are honored during critical times. Providing contact information for healthcare proxies or representatives allows for clear communication regarding medical decisions. A healthcare proxy, who may also serve as a family member or trusted friend, can play a pivotal role in executing the patient's desires when they cannot express their preferences. For example, the designated individual may be required to make choices about life-sustaining treatments and palliative care options during end-of-life scenarios, particularly in hospitals like Mayo Clinic in Rochester, Minnesota, where advanced medical technologies are frequently employed. Documenting this information promotes patient autonomy and ensures that personal values are respected throughout the healthcare journey.
Letter Template For Requesting End-Of-Life Care Plans Samples
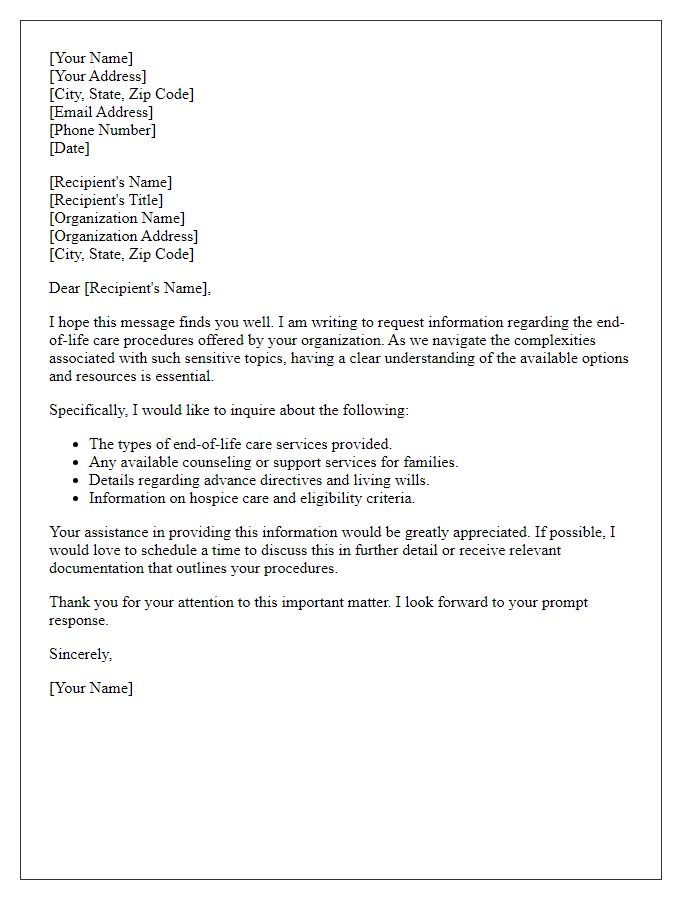
Letter template of request for information on end-of-life care procedures
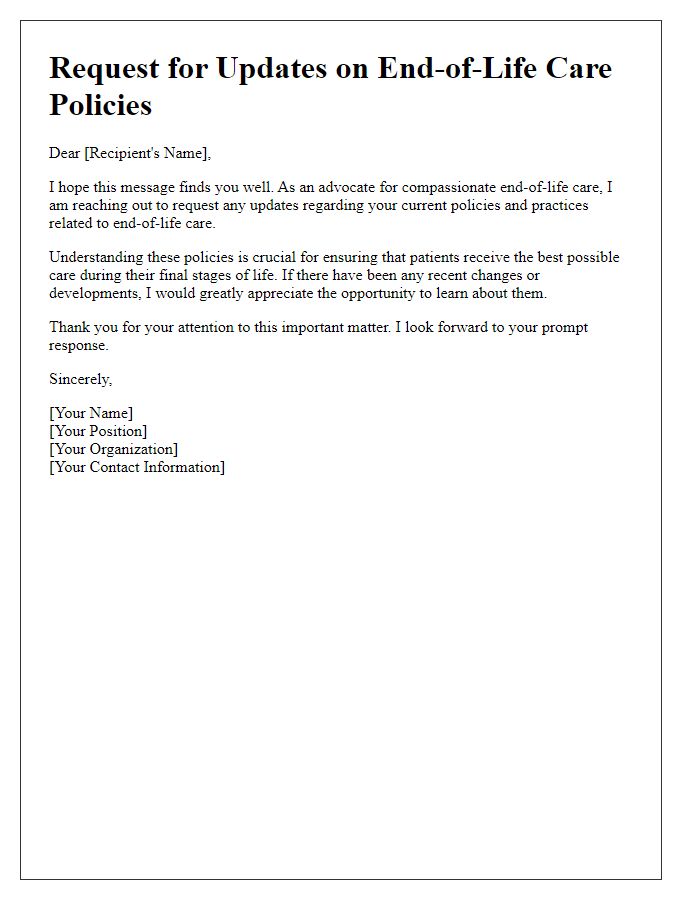
Letter template of solicitation for updates on end-of-life care policies
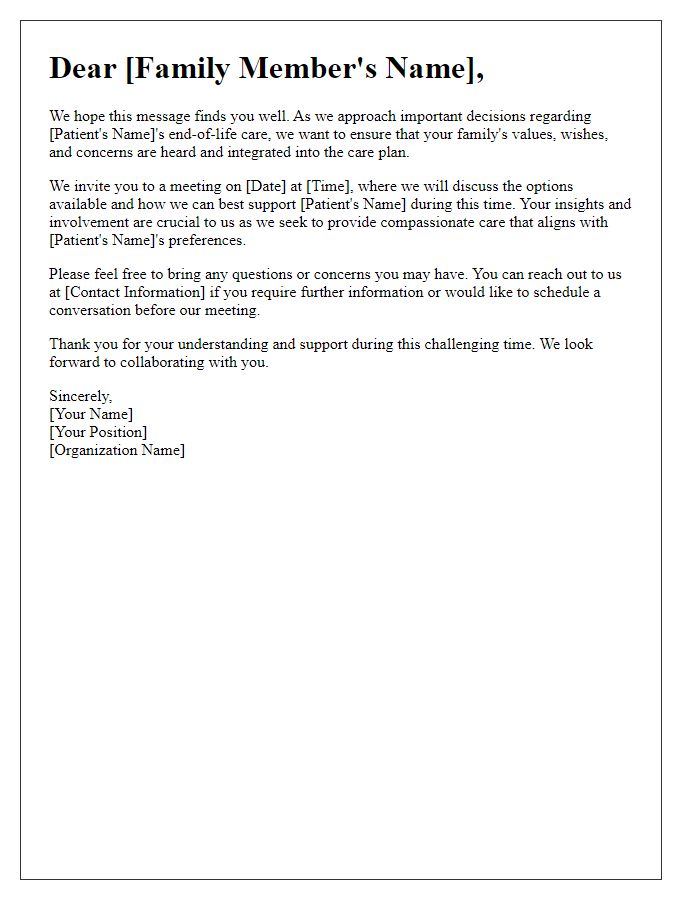
Letter template of communication for family involvement in end-of-life care
Letter template of suggestion for improvement in end-of-life care services


Comments