Are you struggling with eczema and looking for effective treatment options? You're not aloneâmany people face the challenges that come with this skin condition, and finding the right approach can make all the difference. In this article, we'll explore some helpful tips and remedies that can alleviate symptoms and improve your skin health. So, let's dive in and uncover the best strategies to manage eczema effectively!
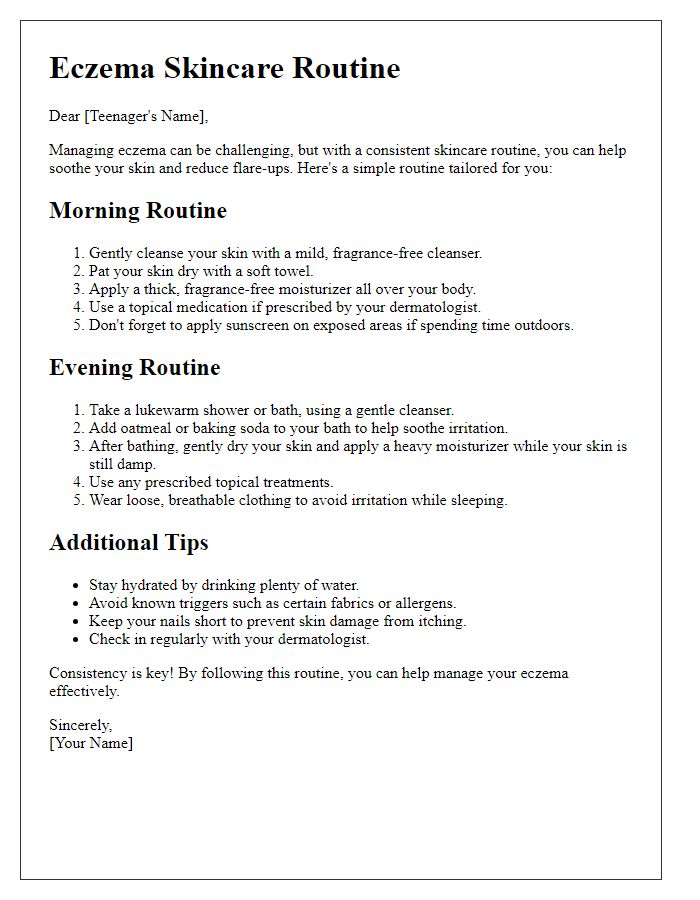
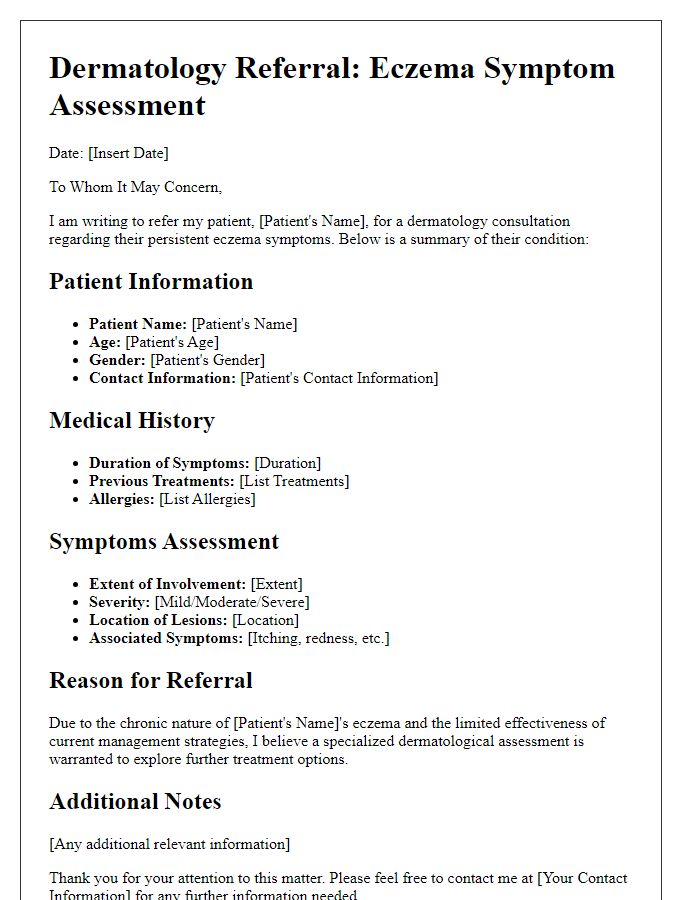
Personalized greeting and clear patient identification.
Eczema, a chronic inflammatory skin condition often characterized by patches of red, itchy, and inflamed skin, requires a tailored treatment approach for optimal management. Common treatments include topical corticosteroids for inflammation control and moisturizers with emollients to maintain skin barrier integrity. Emerging therapies such as biologics aim to target specific immune pathways, offering relief for moderate to severe cases. Environmental factors, such as dust mites and pollen, can exacerbate symptoms, making allergy management essential. Patients should also consider incorporating lifestyle changes, such as stress reduction techniques and dietary adjustments, to mitigate flare-ups. Regular check-ups with dermatology specialists can help refine treatment plans based on individual responses.
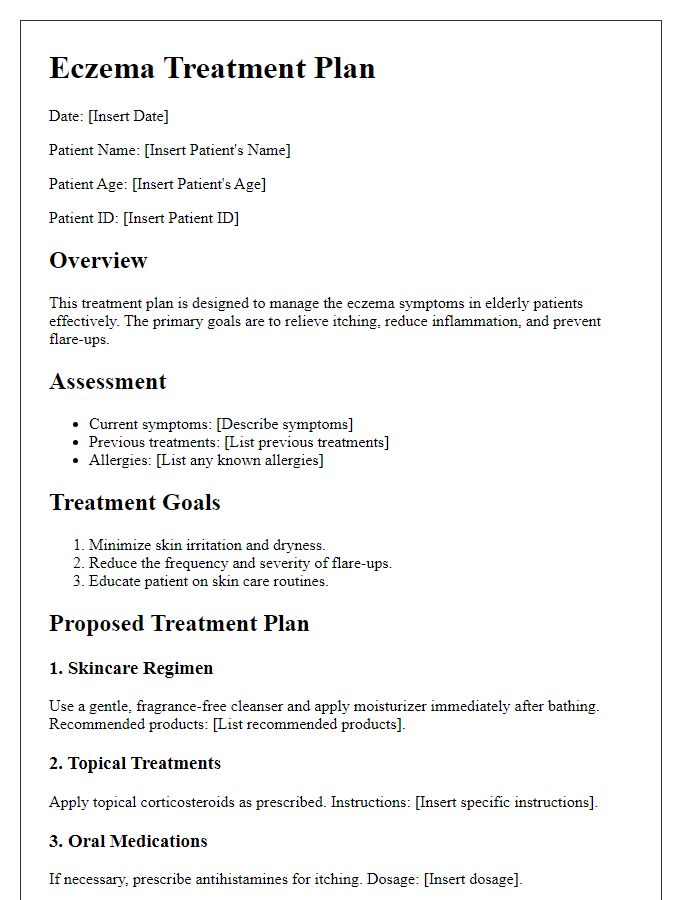
Detailed explanation of diagnosis and severity level.
Eczema, also known as atopic dermatitis, represents a chronic inflammatory skin condition characterized by fluctuating bouts of dryness, itching, and skin irritation. The diagnosis is often confirmed through a physical examination, where criteria from the Hanifin and Rajka classification system are utilized to evaluate symptoms such as pruritus, distinctive morphology, and distribution of lesions. Severity levels--mild, moderate, or severe--are commonly assessed using tools like the SCORAD index, with scores ranging from 0 to 103, where higher values indicate increased severity and worsening impact on overall quality of life. In mild cases, symptoms might involve localized, occasional dryness, whereas moderate to severe eczema can lead to widespread involvement, significant discomfort, sleep disturbances, and possible secondary infections due to skin barrier impairment. Treatment strategies may vary greatly depending on severity and often include topical corticosteroids, moisturizers, and advanced therapies like systemic medications or phototherapy in severe instances.
Specific treatment plan with medication and lifestyle recommendations.
Eczema, a chronic inflammatory skin condition, can significantly affect patients' quality of life. A comprehensive treatment plan includes topical corticosteroids such as Hydrocortisone (mild), Triamcinolone (medium), or Clobetasol (potent) applied directly to affected areas twice daily for optimal results. Emollients like Cetaphil or Aquaphor should be used liberally throughout the day to maintain skin hydration, especially after bathing. Antihistamines, such as Diphenhydramine or Loratadine, can alleviate nighttime itching. Regular lukewarm baths mixed with oatmeal or baking soda may soothe plaques, while avoiding known irritants (e.g., harsh soaps, fragrances, wool fabrics) is vital for prevention. Wearing breathable fabrics like cotton, maintaining a humidity level of 30-50% in living spaces, and managing stress levels may further reduce flare-ups. Regular follow-ups with a dermatologist, especially in severe cases, ensure treatment effectiveness and make necessary adjustments.
Guidelines for managing symptoms and flare-ups.
Eczema, also known as atopic dermatitis, requires careful management to alleviate symptoms and reduce flare-ups. Moisturizers designed specifically for sensitive skin can provide essential hydration, with products containing ingredients like ceramides and hyaluronic acid achieving optimal results. Avoid irritants including harsh soaps and detergents, as well as allergens such as pollen and pet dander, which can exacerbate condition severity. It is crucial to implement a skincare routine that includes gentle cleansing once or twice daily using lukewarm water, as hot water can strip natural oils. Topical steroids, prescribed by healthcare professionals, can effectively manage flare-ups, particularly those classified as moderate to severe. Identifying and avoiding known triggers, such as specific foods (e.g., dairy, nuts) or environmental factors, can significantly reduce the frequency of flare-ups. Regular use of antihistamines during peak allergy seasons can also mitigate itching and discomfort. Consulting with a dermatologist for personalized treatment plans can further enhance management strategies tailored to individual needs.
Contact information for follow-up and questions.
Eczema treatment requires a multifaceted approach, including the use of topical corticosteroids, moisturizers, and antihistamines. Regular application of emollients, such as those containing ceramides, helps to maintain skin hydration (recommended at least twice daily). In addition, identifying and avoiding triggers like specific allergens (e.g., pollen, pet dander) is crucial in managing flare-ups. For persistent symptoms, dermatologists often prescribe systemic therapies (e.g., corticosteroids or biologics such as Dupilumab) to alleviate inflammation. Regular follow-up appointments are essential to adjust treatment plans based on individual response and monitor for potential side effects. Patients are encouraged to maintain open communication with their healthcare provider to address concerns and enhance overall skin health.


Comments