When it comes to hospice care, understanding eligibility can feel overwhelming, but it doesn't have to be! Hospice care is designed to provide comfort and support for patients facing terminal illnesses, typically within a six-month prognosis. If you're navigating these sensitive waters for yourself or a loved one, knowing the criteria can make a world of difference in accessing the compassionate care you deserve. Read on to discover the essential details that can guide you through the process and ensure you have the best options available.
Medical diagnosis and prognosis
Hospice care eligibility hinges on specific medical diagnoses and prognoses. Terminal illnesses must be confirmed by a healthcare provider, often including conditions like advanced stage cancer, chronic obstructive pulmonary disease (COPD), heart failure, or neurological disorders such as Alzheimer's disease. A prognosis of six months or less to live is typically required for hospice admission; this timeframe is critical for individuals to receive palliative care focused on comfort rather than curative measures. Documentation must reflect the patient's condition, treatments, and response to therapies, outlining the limitations of current medical interventions. Healthcare providers must ensure that these criteria are meticulously assessed to determine the appropriateness of hospice services.
Patient's functional status and daily activities
Hospice care eligibility is determined by various factors, primarily focusing on the patient's functional status and daily activities. A patient requiring hospice care often experiences significant decline in their ability to perform essential daily activities, such as bathing, dressing, or eating, which indicates a functional status typically assessed using the Palliative Performance Scale (PPS); patients scoring below 70% generally qualify. Furthermore, patients might demonstrate a deterioration in cognitive abilities, leading to increased reliance on caregivers for daily tasks. Patients frequently report experiencing persistent symptoms, including pain, fatigue, or difficulty breathing, despite aggressive medical interventions. These key aspects, combined with a prognosis of six months or less to live, establish the criteria for transitioning to hospice care, emphasizing comfort and quality of life over curative treatments.
Documented decline in health
Patients receiving hospice care often require specific eligibility criteria, such as a documented decline in health. This decline usually manifests through measurable changes in medical conditions, such as a decrease in the patient's ability to perform daily activities (Activity of Daily Living, ADL). Conditions like advanced cancer, end-stage heart disease (e.g., congestive heart failure), or progressive neurological disorders (e.g., Alzheimer's disease) often indicate a prognosis of six months or less, as determined by a healthcare professional. Medical records must reflect such findings, including symptoms like weight loss exceeding 10% of body weight within six months or recurrent hospitalizations. These details are critical in establishing eligibility for hospice services, which focus on providing palliative care aimed at enhancing quality of life during the final stages of illness.
Psychosocial and emotional considerations
Hospice care eligibility often involves evaluating psychosocial and emotional considerations pivotal for both patients and their families facing terminal illnesses. In the context of hospice services, such as those provided by Medicare-certified facilities, the presence of significant emotional distress, anxiety, or depression can indicate the need for specialized support. Patients dealing with life-limiting conditions, such as advanced cancer or late-stage heart disease, frequently experience altered mental states or heightened emotional burdens. These factors not only impact the individual's quality of life but also the coping mechanisms of family members, requiring comprehensive assessments by interdisciplinary teams that include social workers and counselors. Furthermore, end-of-life discussions facilitate emotional preparedness, ensuring that both patients and their families have access to effective resources for grief and bereavement support, which is critical in navigating the complexities of their situations.
Physician's certification of terminal illness
Hospice care services offer compassionate support for patients diagnosed with terminal illnesses, such as advanced cancer, end-stage heart failure, or Alzheimer's disease, when life expectancy is six months or less. Physicians, often specialized in palliative care, must provide a certification confirming the patient's terminal condition based on clinical assessments. This certification, encompassing the patient's medical history, prognosis, and treatment options, is crucial for Medicare and Medicaid eligibility. The hospice team includes interdisciplinary professionals, such as nurses, social workers, and chaplains, working collaboratively to enhance quality of life for both patients and families, focusing on pain management, emotional support, and holistic care approaches.
Letter Template For Hospice Care Eligibility Samples
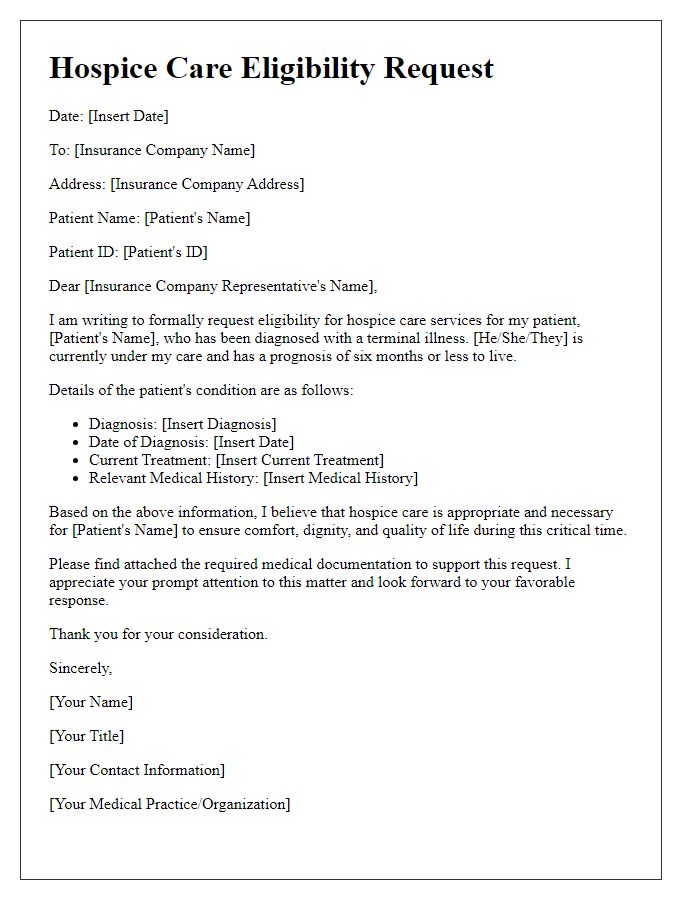
Letter template of hospice care eligibility request for patients with terminal illness.
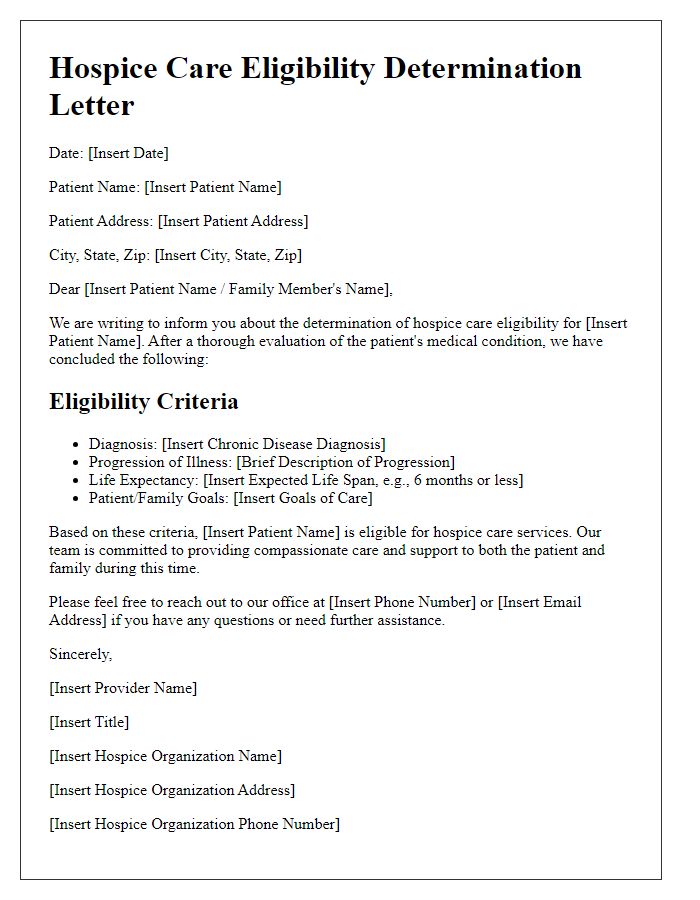
Letter template of hospice care eligibility determination for chronic disease patients.
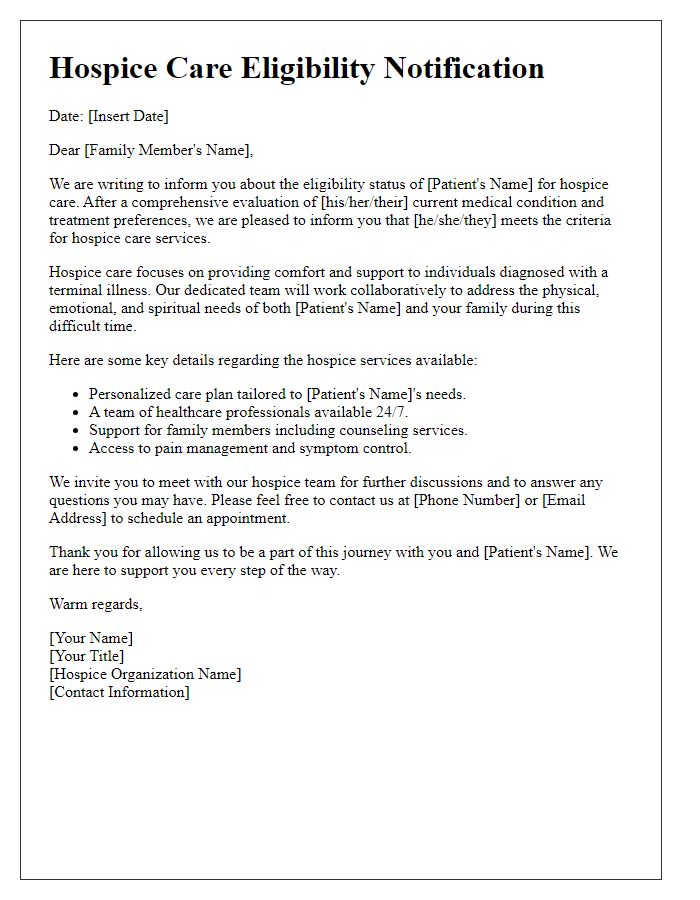
Letter template of hospice care eligibility notification for family members.
Letter template of hospice care eligibility inquiry for healthcare providers.
Letter template of hospice care eligibility assessment for palliative care transition.
Letter template of hospice care eligibility confirmation for insurance purposes.
Letter template of hospice care eligibility summary for patient records.
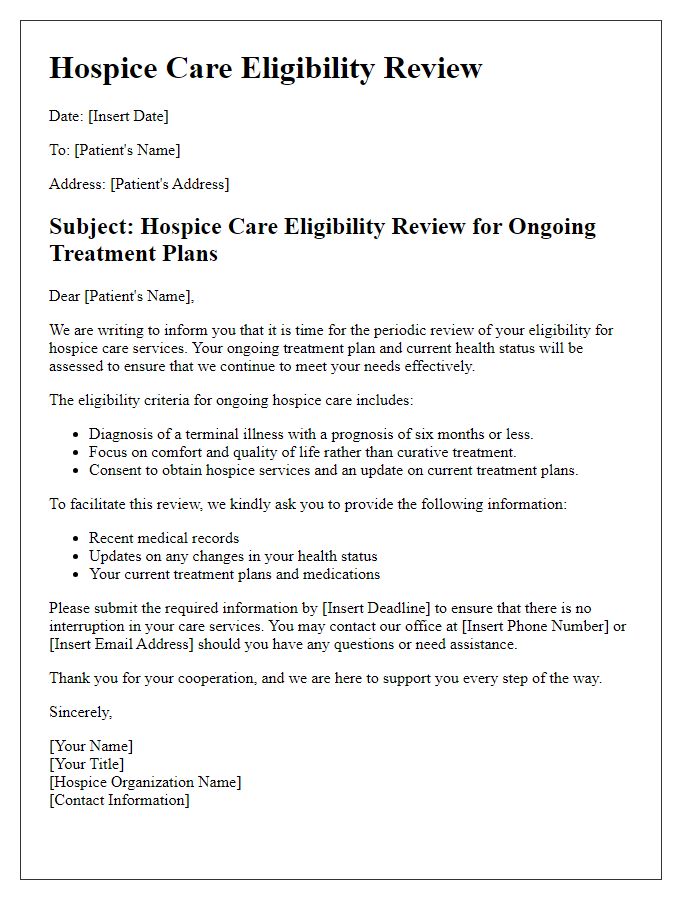
Letter template of hospice care eligibility review for ongoing treatment plans.


Comments