Are you feeling overwhelmed by a hospital bill that seems excessively high? You're not aloneâmany people face similar challenges when it comes to medical billing disputes. Tackling these issues doesn't have to be daunting, and understanding your rights can empower you to fight back. Join us as we explore how to effectively dispute hospital bill overcharges and reclaim your peace of mind.
Patient information
In the city of San Francisco, hospital billing discrepancies have become a pressing concern for many patients seeking medical care. Patients, such as those treated at UCSF Medical Center, often experience unexpected overcharges on their hospital bills, which can include inflated fees for procedures, tests, or emergency services. For instance, a common issue may arise when patients are billed multiple times for the same service, such as a CT scan, which typically costs an average of $1,200 in California. Additionally, charges for necessary medications, such as pain relievers or antibiotics, can significantly vary, leading to frustrations among patients. Proper patient information, including insurance details and visit dates, is crucial for addressing these disputes effectively, ensuring patients can challenge unjust fees and seek resolution.
Hospital details and bill reference
Disputes over hospital bills can arise due to various reasons, including overcharges associated with procedures or medications. A detailed analysis of the billing statement reveals discrepancies in charges for services rendered at XYZ Hospital, renowned for its cardiovascular care, located in Springfield. The bill reference number 123456789 corresponds to services provided on January 15, 2023, which include a cardiac catheterization that was billed at $15,000, significantly higher than the average cost of $10,000 for similar procedures in the region. Additionally, the itemized list includes a charge for a standard blood test at $500, which, based on local market rates, averages around $100. It is crucial to address these inconsistencies promptly to ensure appropriate billing practices and maintain transparency in healthcare costs, particularly for patients navigating financial burdens during recovery.
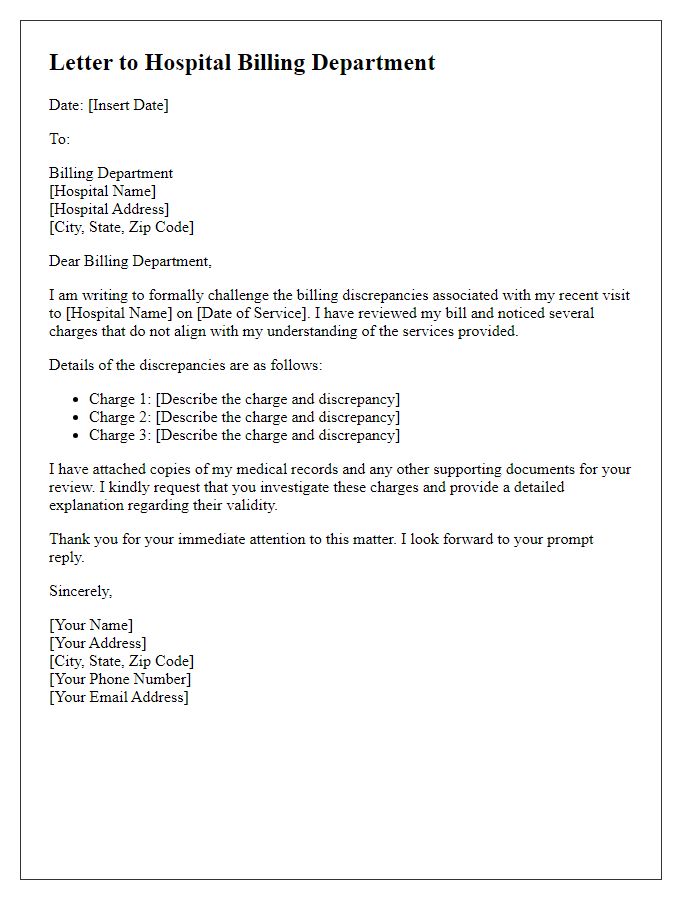
Specific discrepancies in charges
Discrepancies in hospital bills can arise due to various reasons, prominently seen in the charges for services like imaging, consultations, and laboratory tests. A common example includes the billing for an MRI scan at XYZ Hospital, where the standard charge (averaging $1,200) may inflate to over $2,000 due to additional fees for the radiologist's interpretation. Another area of concern is the the emergency room visit, typically priced around $500, which can escalate to $1,000 if bundled with charges for various diagnostic procedures that may not have been performed. In ICU settings, daily rates can vary significantly, with some facilities charging as much as $4,000 per day compared to a national average of $3,000, leading to confusion for patients reviewing their bills. Additionally, coding errors can result in inflated expenses if services are billed under a more expensive category, such as classifying a routine check-up as a complex consultation. Addressing these discrepancies is essential for ensuring fair billing practices within healthcare settings.
Supporting documentation
Disputing hospital bill overcharges can be crucial for managing healthcare expenses. For example, when receiving a bill from a facility like St. Mary's Hospital in July 2023, discrepancies may arise in charges for specific procedures, such as a CT scan costing $2,000 instead of the average $800 based on industry standards. Supporting documentation, including an itemized bill illustrating all procedures and their associated costs, medical records detailing treatments received, and insurance statements indicating coverage limits, are vital for substantiating claims of overcharging. Additionally, references to state regulations or insurance policies that outline allowable charges can strengthen the case. Obtaining a written explanation of benefits (EOB) from the insurance provider and contacting the hospital's billing department for clarification can further assist in resolving billing issues efficiently.
Request for prompt review and correction
Hospital billing discrepancies often arise from overcharges on various services rendered. A common issue is inflated charges for treatments or medications, which may not align with standardized rates outlined by insurance providers. For example, a routine blood test priced at $200 could be unjustly billed at $600 in specific hospitals, leading to confusion and frustration for patients. Timely review of billing statements is essential, as insurance adjustments and patient deductions should be applied correctly. It's crucial to document all services received against the itemized bill, ensuring transparency and accuracy in charges. The contact points for the billing department can vary across healthcare facilities; therefore, fostering communication with proper documentation can facilitate a resolution. Specific instances of overreach can significantly affect personal finances, necessitating swift and thorough investigation into the matter.
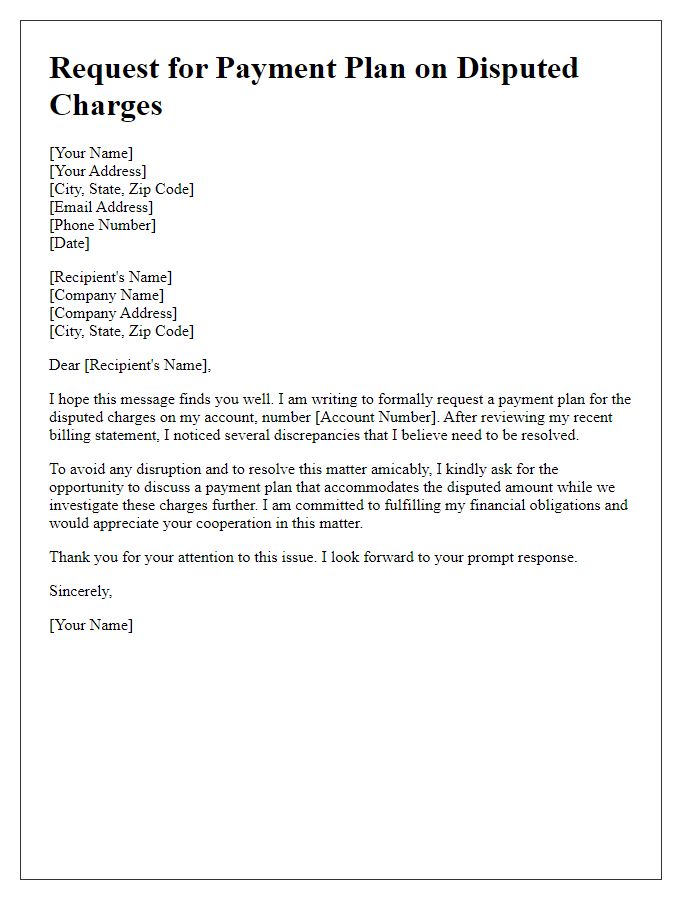
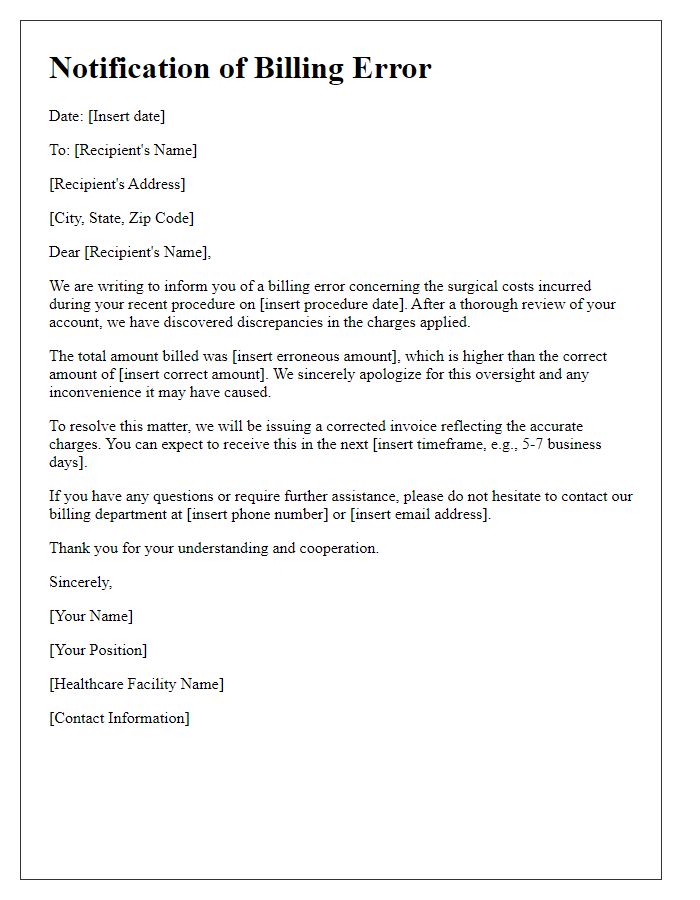
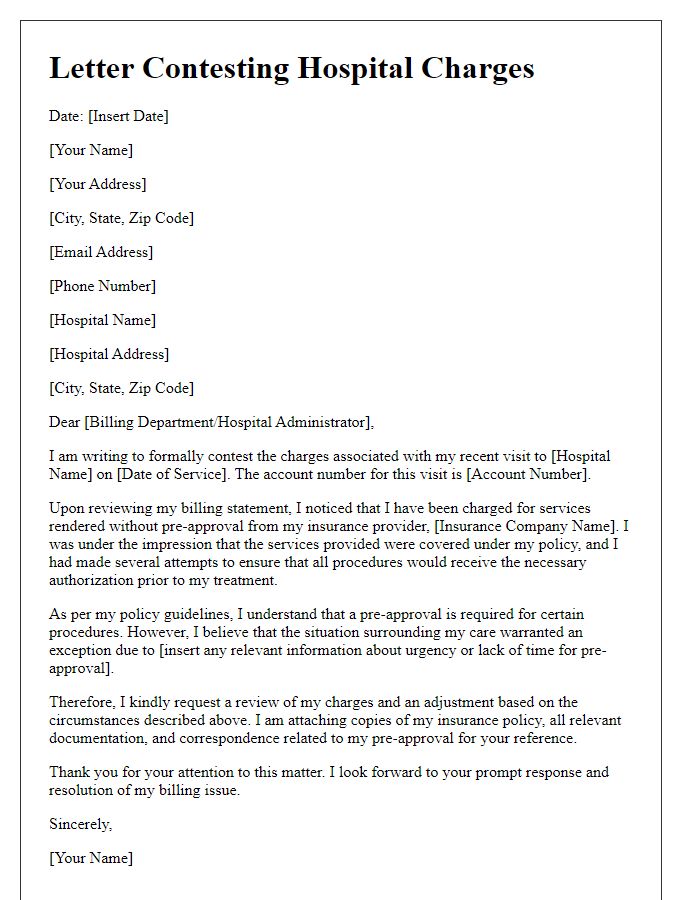
Letter Template For Disputing Hospital Bill Overcharges Samples
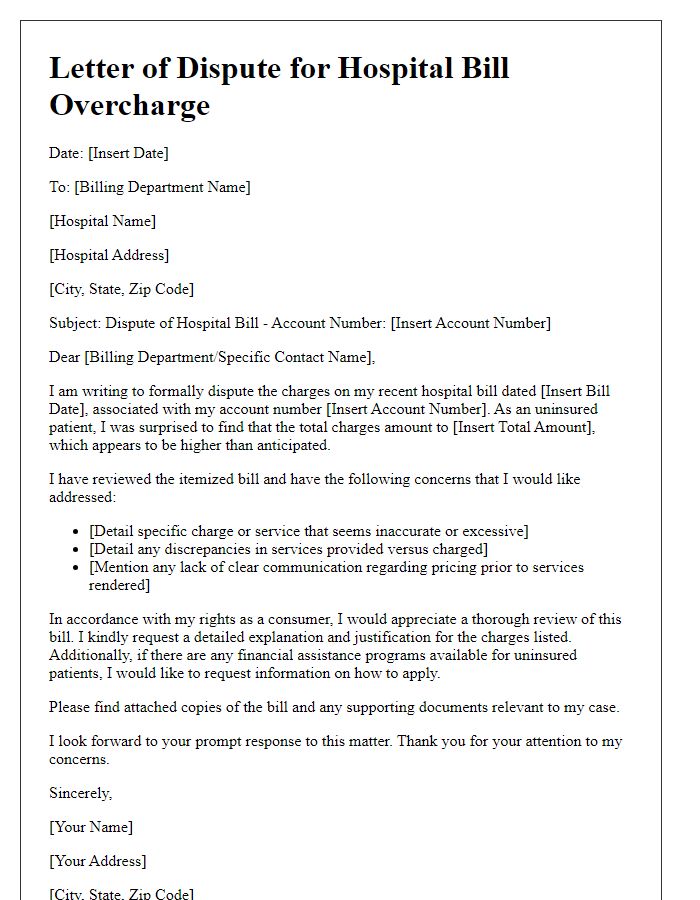
Letter template of hospital bill overcharge dispute for uninsured patients
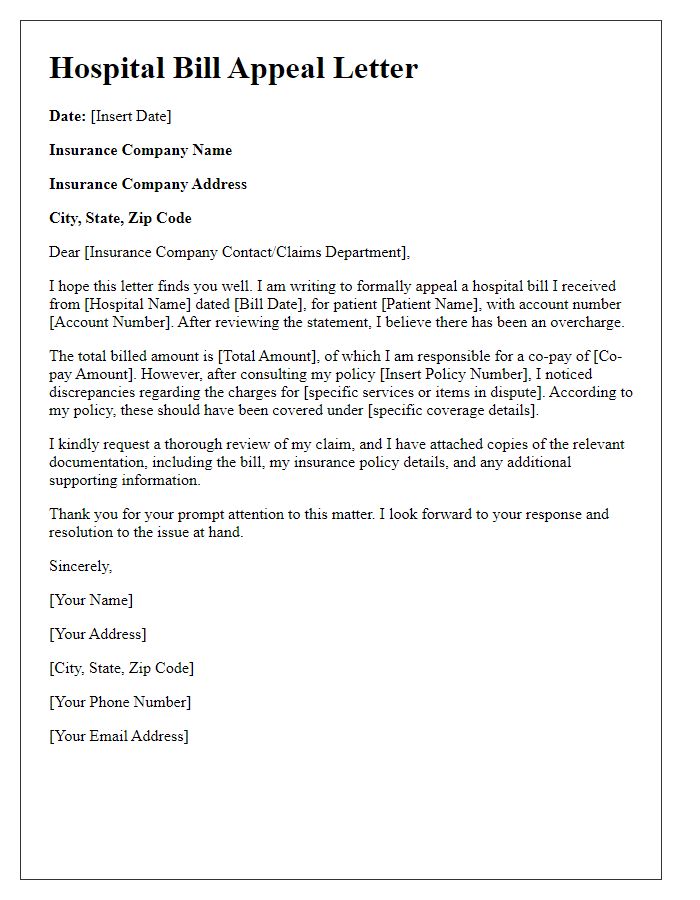
Letter template of hospital bill overcharge appeal for insured individuals



Comments