In the ever-evolving world of healthcare, ensuring the precision of medical coding is paramount for effective patient care and billing practices. Accurate coding not only facilitates proper reimbursement but also enhances patient safety through clearer documentation. With the complexities of coding rules and regulations, regular accuracy checks are essential to maintain compliance and streamline operations. Dive deeper into this crucial topic and discover best practices for achieving flawless medical coding in our article!
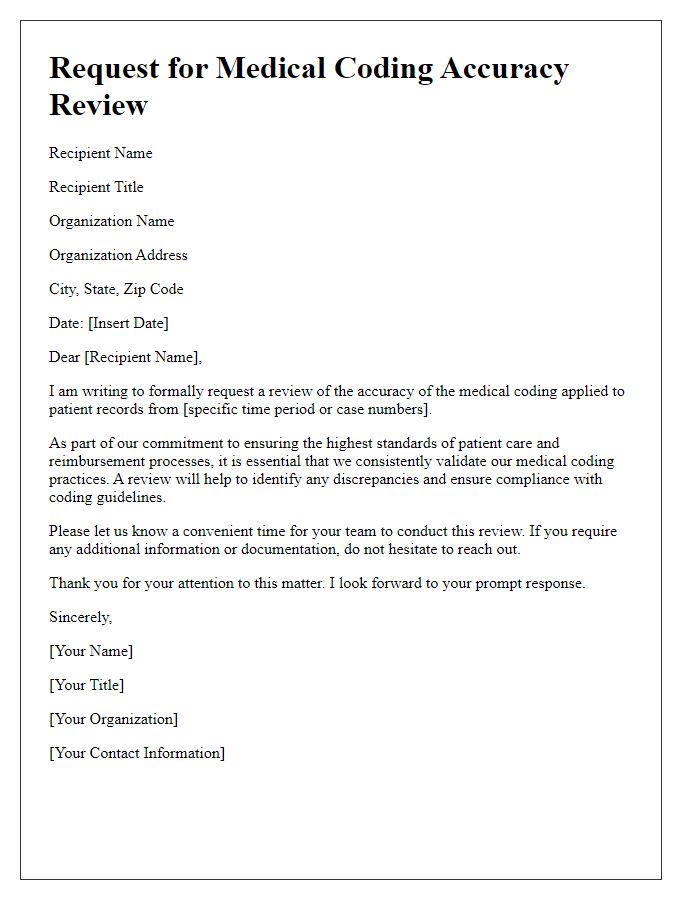
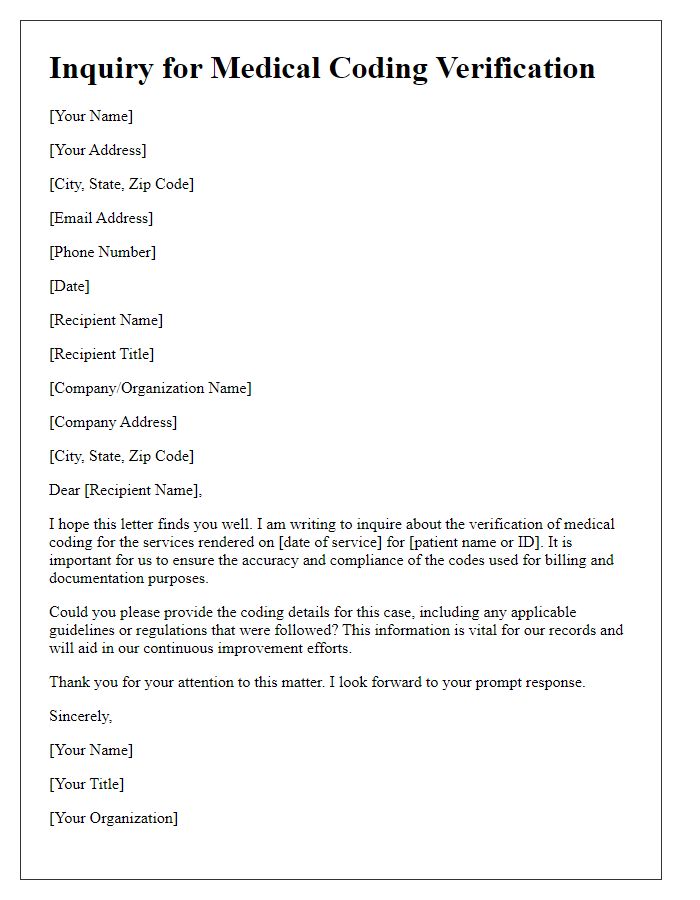
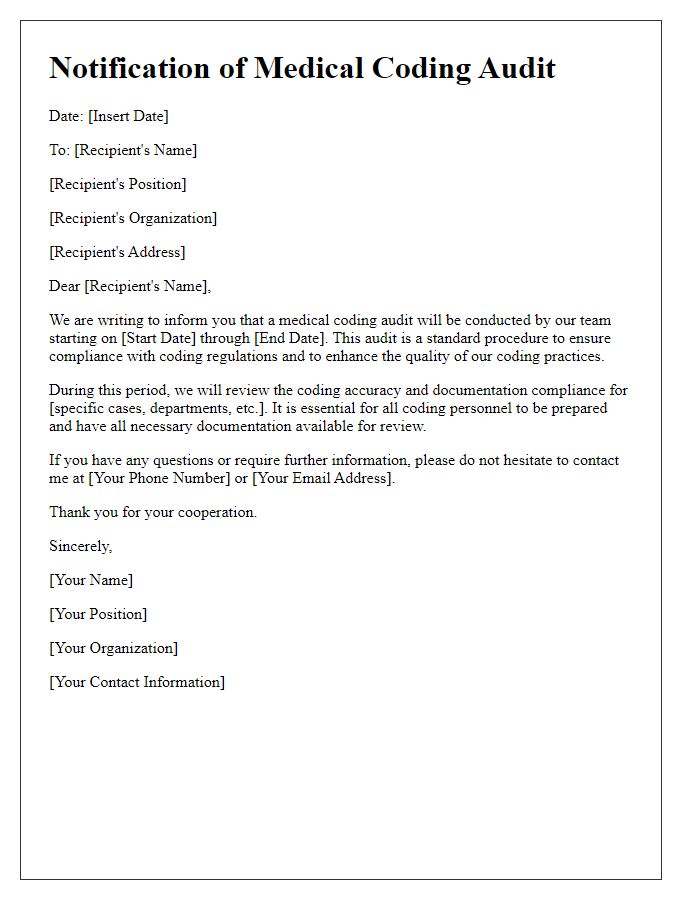
Patient Information Verification
Patient information verification is crucial in ensuring accurate medical coding within healthcare facilities. Accurate identification of patients, including their names, dates of birth, and insurance details, directly influences the integrity of medical records. Discrepancies in demographic data can lead to errors in coding claims, affecting reimbursement processes and compliance with regulations from entities like the Centers for Medicare & Medicaid Services (CMS). Each patient's encounter must be carefully evaluated against established coding guidelines such as ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) to ensure proper categorization of diagnoses and procedures. Consistent audits of patient information are essential for maintaining data accuracy over time, leading to improved patient outcomes and streamlined administrative operations.
Detailed Medical Record Review
In the realm of healthcare documentation, conducting a detailed medical record review is essential for ensuring coding accuracy in medical billing systems, like ICD-10 (International Classification of Diseases, Tenth Revision) and CPT (Current Procedural Terminology) guidelines. This review process typically encompasses analyzing various patient records, including encounter notes, lab results, and imaging studies, to identify any discrepancies or missing information that could lead to incorrect coding or reimbursement issues, such as denied claims or audits by organizations like the Centers for Medicare & Medicaid Services (CMS). The reviewer closely examines elements including patient demographics, diagnosis specifications, treatment plans, and procedural details, ensuring alignment with coding standards established by entities such as the American Academy of Professional Coders (AAPC). Key performance indicators (KPIs) such as code assignment accuracy rates (ideally above 95%) and query response timelines are monitored to enhance overall coding integrity, ultimately impacting departmental revenue cycles and compliance with healthcare regulations.
Code Selection Accuracy
Medical coding accuracy check involves meticulous evaluation of assigned codes to ensure they correctly reflect patient diagnoses, procedures, and services rendered. Specific diagnostic codes, such as ICD-10-CM codes, must align with clinical documentation to maintain compliance with healthcare regulations. Accurate procedural codes, categorized under CPT codes or HCPCS codes, should clearly represent the services provided within a healthcare facility, for instance, a hospital or outpatient clinic. Review processes typically incorporate an analysis of coding compliance, adherence to payer guidelines, and potential revenue impact, emphasizing the importance of precision in medical record-keeping. Regular audits and training help maintain coding accuracy, leading to reduced billing errors, improved reimbursement rates, and enhanced quality of patient care.
Compliance with Coding Guidelines
Medical coding accuracy ensures compliance with established coding guidelines such as the International Classification of Diseases (ICD-10), which enables accurate representation of patient diagnoses. Adherence to the Current Procedural Terminology (CPT) codes is crucial for billing processes and requires meticulous attention to detail. Accurate coding leads to improved claims processing times and reduced denial rates from insurance providers. Regular audits and updates to coding practices support compliance with regulations set forth by entities like the Centers for Medicare and Medicaid Services (CMS), safeguarding against potential penalties. Enhanced coding accuracy directly impacts the quality of patient data submitted for research and public health reporting, ensuring healthcare facilities maintain their credibility and financial stability.
Feedback and Observation Documentation
Medical coding accuracy is crucial for proper billing and ensuring compliance with regulations. For instance, in hospitals like Mayo Clinic or Cleveland Clinic, accuracy can significantly impact reimbursement rates and patient care. Frequent audits highlight areas of improvement, such as the incorrect assignment of codes like ICD-10 or CPT, affecting claims submissions. Observation of coding practices reveals that common errors include omitted modifiers, unbundled services, or inaccurate diagnosis coding, which can lead to claim denials. Comprehensive training programs and regular feedback sessions enhance coder performance, ensuring adherence to standards set by entities like the Centers for Medicare & Medicaid Services (CMS). Continuous education on updates in coding guidelines is essential for maintaining high accuracy.


Comments