When navigating the world of health insurance, understanding out-of-network claims can feel like a daunting task. Many people are caught off-guard when they discover that their favorite healthcare provider doesn't fall under their insurance plan's network. This article aims to clarify the intricacies of out-of-network claims, shedding light on what to expect and how to effectively handle these situations. So, if you're looking to demystify your insurance claims process, stick around to learn more!
Patient Information
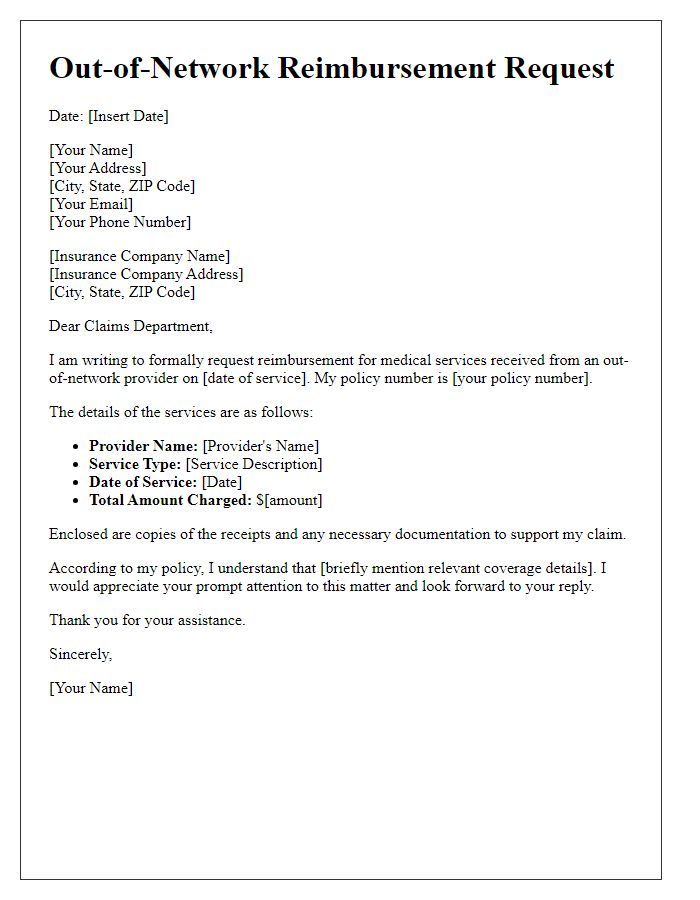
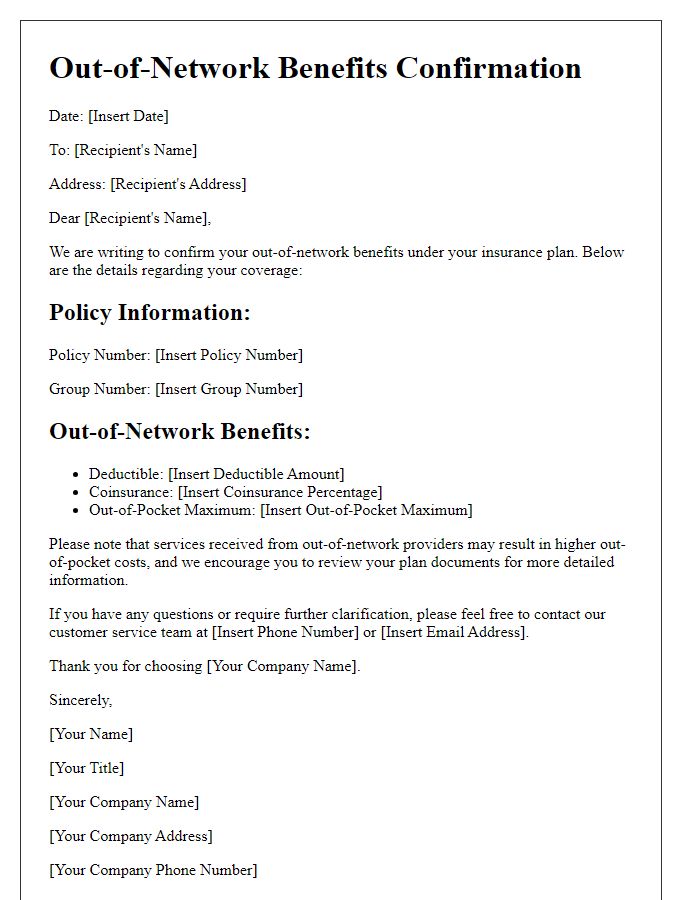
A clear understanding of out-of-network claims can significantly impact patient experience and financial responsibility, especially in contexts involving healthcare services provided by facilities or specialists outside an insurance provider's established network. For example, patients receiving treatment at institutions like Memorial Sloan Kettering Cancer Center may find themselves navigating complex claims processes after surgery or therapy sessions. This complexity often arises when specialty care, such as chemotherapy or radiation therapy, is needed and the chosen provider does not have a contractual agreement with the patient's insurance carrier, leading to higher out-of-pocket costs. Proper documentation is essential, including detailed invoices, physician notes, and treatment plans, as these details will help substantiate the claim submission. Moreover, patients should pay close attention to the specific terms outlined in their insurance policies regarding reimbursement for out-of-network services, as co-pay rates and coverage caps can vary widely depending on the plan provider, often governed under specific rules of the Affordable Care Act.
Service Details
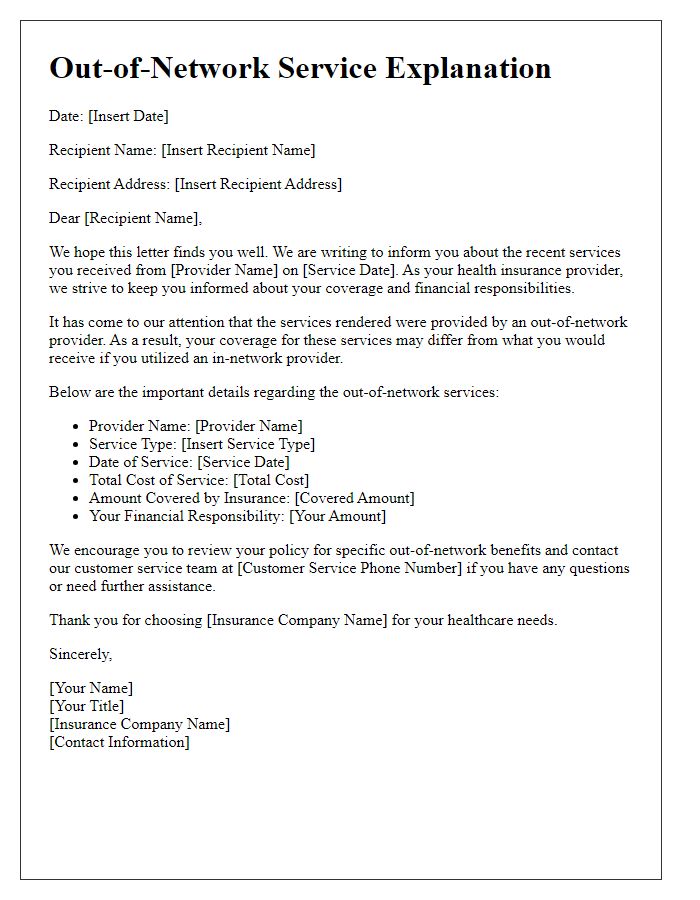
Out-of-network claims can arise from medical services accessed outside an insurance provider's network, often leading to higher out-of-pocket expenses for patients. For instance, a patient's recent visit to a specialized orthopedic surgeon in New York City resulted in an unexpected bill of $1,200, significantly above the in-network rate. Such services might include advanced imaging (like MRI scans), surgeries, or consultations. Patients must consider factors like the reason for selecting an out-of-network provider, availability of in-network options, and potential impact on overall healthcare costs. Proper documentation, including itemized bills and referral letters, can assist in the claims process. Understanding insurance policies, including deductible thresholds and reimbursement percentages, remains crucial for managing financial responsibilities effectively.
Provider Explanation
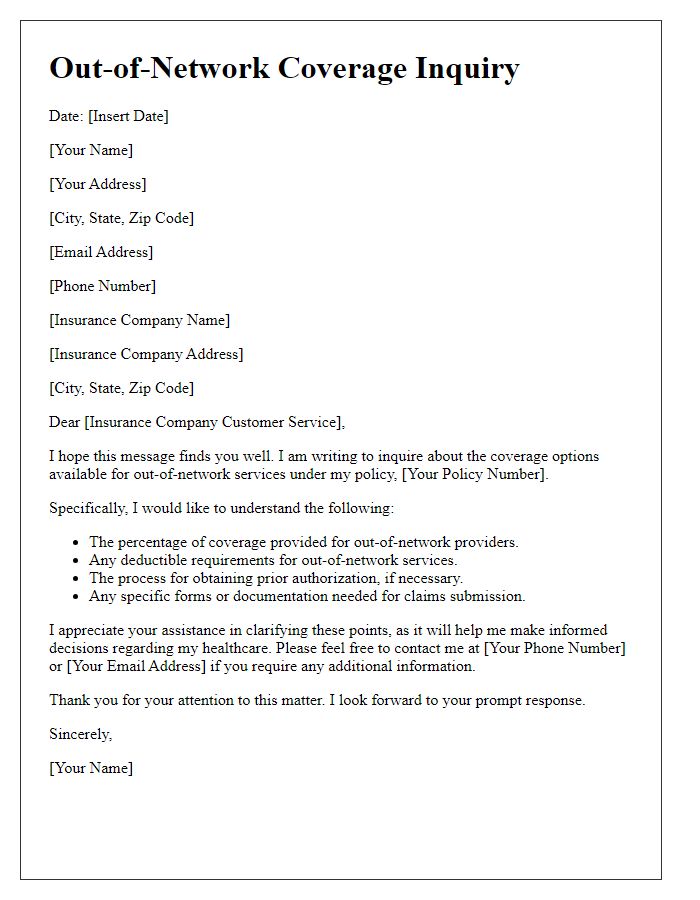
Out-of-network claims frequently lead to confusion for patients regarding reimbursement for services rendered by healthcare providers. The term "out-of-network" refers to medical practitioners or facilities that do not have a contractual agreement with a patient's health insurance plan, such as Blue Cross Blue Shield or Aetna. Patients may encounter higher costs (sometimes up to 100% of billed charges) for these services, particularly if their insurance policy has a high deductible or limited out-of-network benefits. Additionally, unexpected balance billing occurs when providers charge patients the difference between what the insurance covers and their billed rates, often complicating financial responsibilities. Understanding the terms of one's health plan, including coverage limits and potential reimbursements, is crucial for navigating the complexities of out-of-network claims.
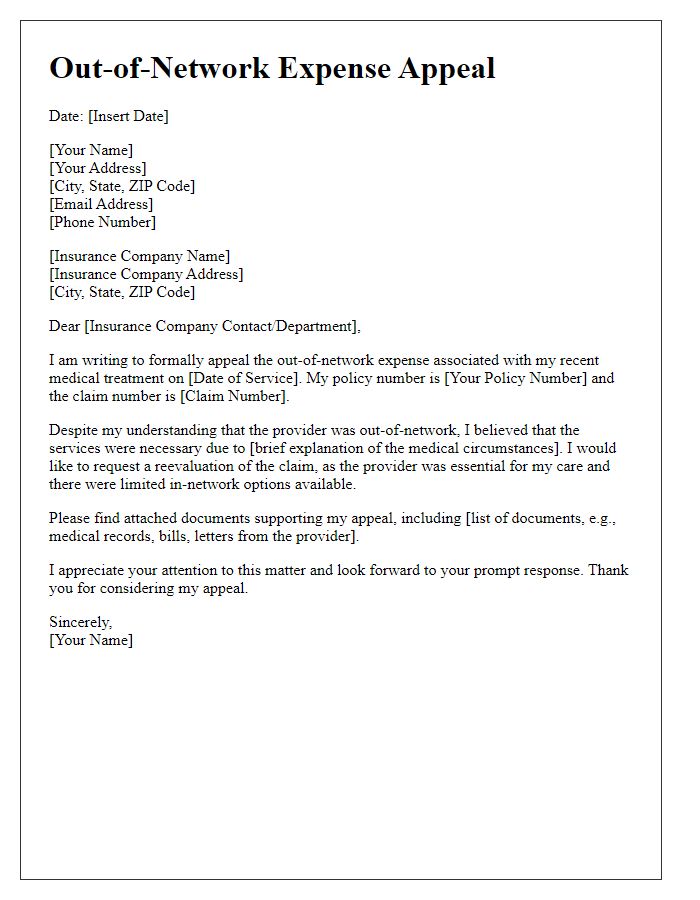
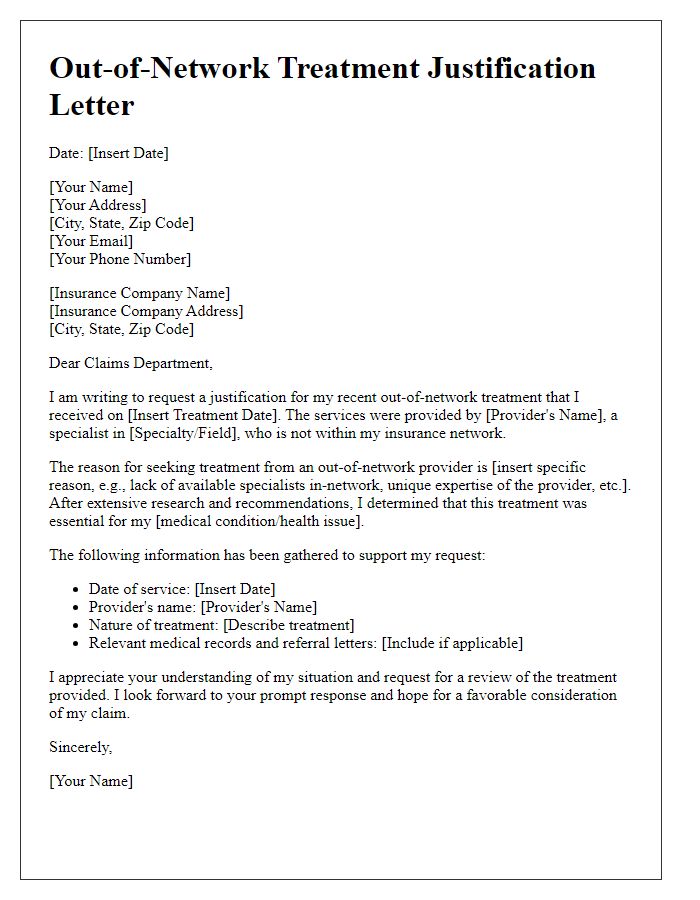
Reason for Out-of-Network Use
Navigating the complexities of health insurance can be challenging, especially when dealing with out-of-network claims. Out-of-network use often arises from urgent medical situations, whereby patients require immediate care that is not available through in-network providers. For instance, a patient suffering a heart attack may need treatment at a nearby facility even if it is out of network, as timing is critical and may directly influence outcomes. Additionally, certain specialized procedures or services, such as advanced cancer therapy or rare surgical interventions, may only be available from specific providers who are not part of the patient's insurance network. Geographic restrictions can also contribute; individuals living in rural areas may have limited access to in-network options, necessitating out-of-network care for essential services. It's crucial for patients to maintain detailed records of their healthcare decisions and communications with their insurance providers to support their claims for out-of-network reimbursement.
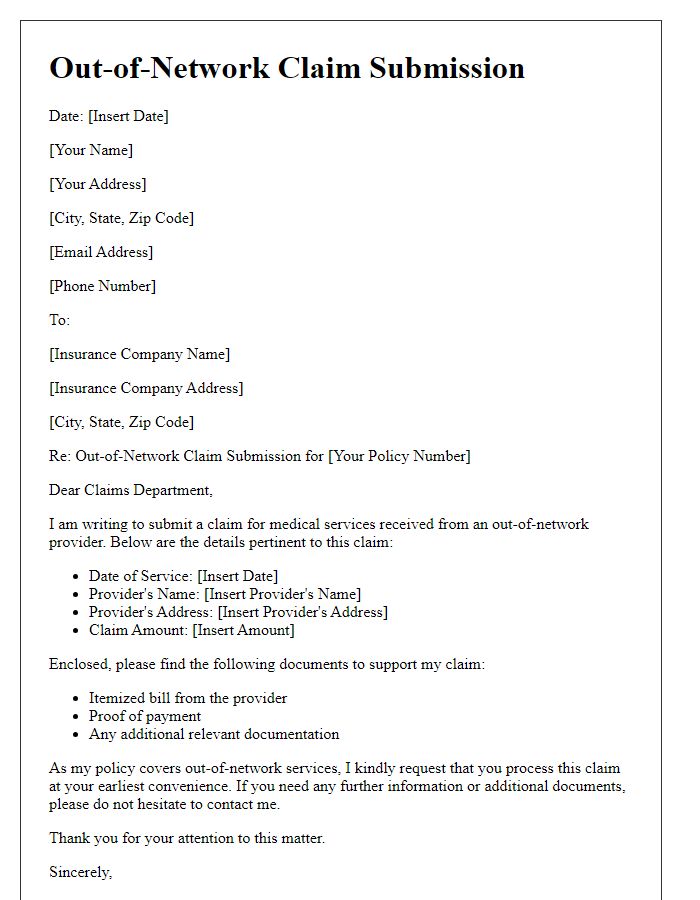
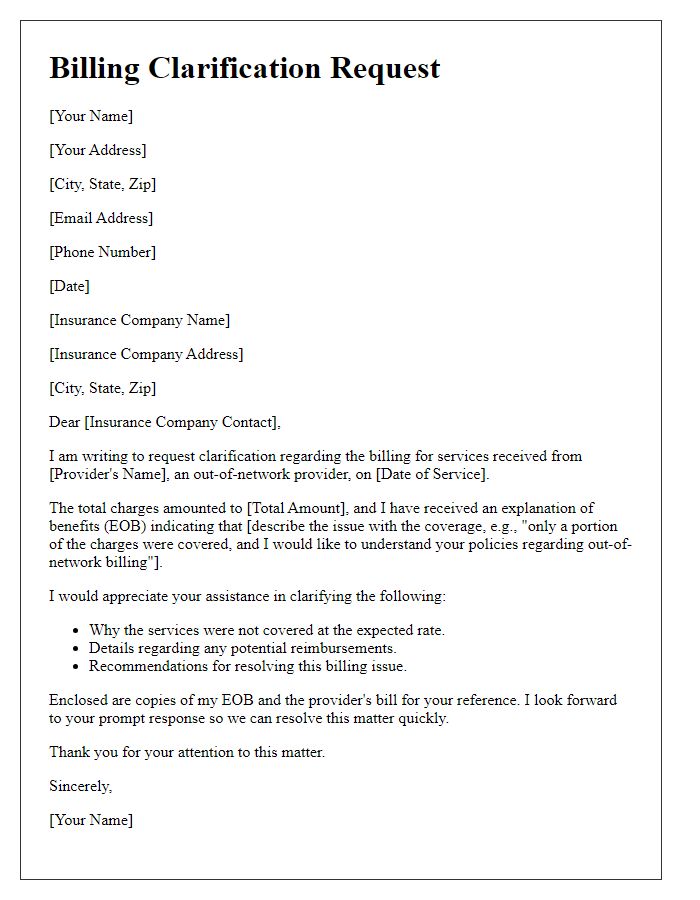
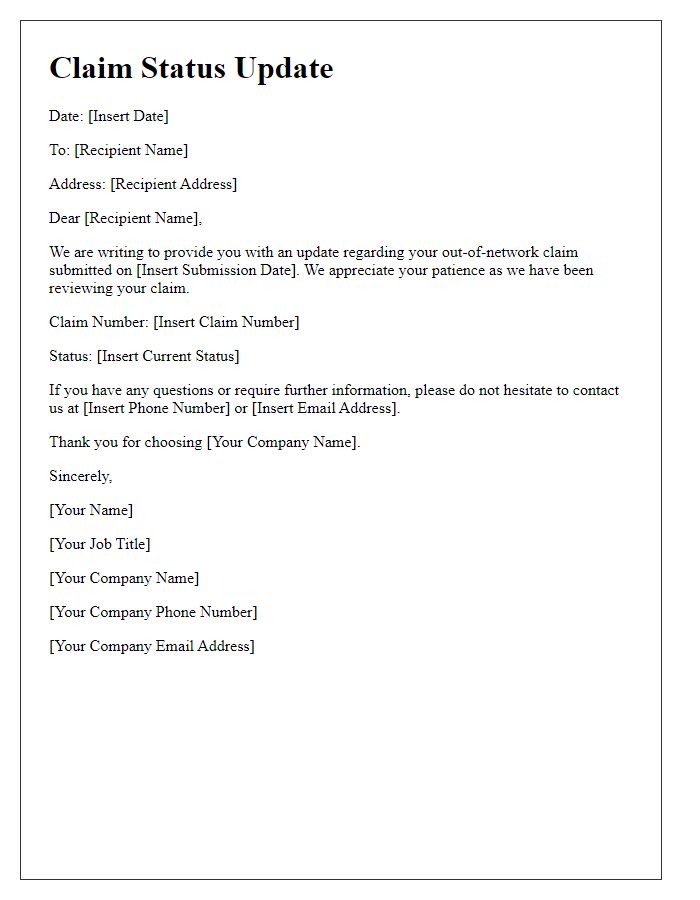
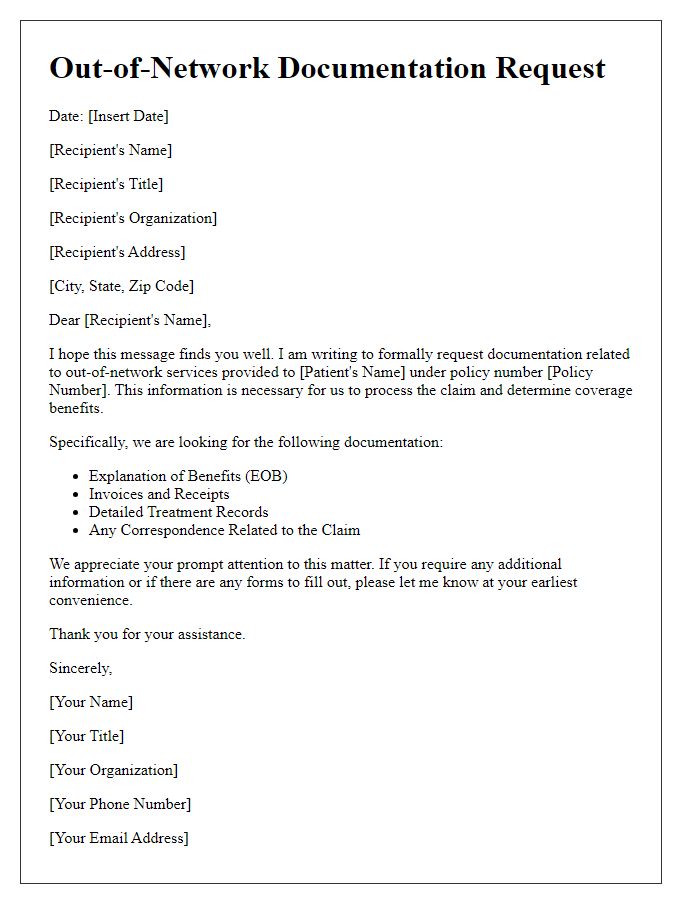
Supporting Documentation
When submitting an out-of-network claim, supporting documentation is crucial for validation. This may include detailed medical records, such as diagnosis codes (ICD-10) and treatment notes from healthcare providers, such as specialists or hospitals not contracted with insurance networks. Itemized billing statements should accompany the claim, listing exact charges incurred during procedures or consultations, as well as CPT codes indicating specific medical services rendered. A copy of the insurance card is also essential to verify policy details, along with a completed claim form provided by the insurance company. For effective processing, documentation should clearly outline the rationale for out-of-network services, addressing medical necessity and continuity of care, particularly in cases involving urgent or specialized treatment.


Comments