Are you considering joining a health insurance network but unsure where to start? You're not aloneâmany providers find navigating the complexities of network participation challenging yet rewarding. In this article, we'll explore the key steps to align your practice with a health insurance network effectively and the benefits it can bring to your patients and practice. Dive in to discover how you can optimize your participation and enhance your service offerings!
Introduction and Purpose
Health insurance network participation plays a crucial role in providing accessible healthcare services to members. Engaging with leading health insurance providers like Aetna, Cigna, and Blue Cross Blue Shield ensures a wide range of coverage options and enhanced patient experiences. The primary purpose of this participation includes expanding provider networks, improving financial arrangements, and fostering collaborative care models. Each aspect aims to optimize patient outcomes, reduce costs, and facilitate seamless access to necessary medical services. Such initiatives can ultimately lead to increased member satisfaction and a healthier population overall.
Qualifications and Experience
The application for participation in a health insurance network requires thorough documentation of qualifications and experience. Essential qualifications include relevant degrees, such as Doctor of Medicine (MD) or Bachelor of Science in Nursing (BSN), awarded by accredited institutions. Additionally, board certifications in specialties, such as Family Medicine or Pediatrics, validate the expertise of healthcare providers. Experience can be demonstrated through years of practice in clinical settings, including hospitals, outpatient clinics, and specialty care facilities. Participation in continued education programs, such as those accredited by the American Medical Association (AMA), further signifies dedication to maintaining current medical knowledge. Lastly, specific metrics like patient satisfaction scores or health outcomes can enhance the application, evidencing a commitment to quality care and positive patient experiences.
Network Benefits and Value Proposition
Health insurance network participation provides a significant array of benefits, ensuring patients receive access to high-quality healthcare services at reduced costs. Participating providers can leverage negotiated rates, offering patients lower out-of-pocket expenses for services such as routine check-ups, specialist consultations, and emergency care. Enhanced care coordination among network clinics (such as those in urban metropolitan areas) fosters improved patient outcomes, while preventive service coverage encourages individuals to seek wellness checks and vaccinations. Additionally, a robust network often includes a wide range of specialty providers, ensuring comprehensive care for chronic conditions like diabetes or cardiovascular disease. For health plans, maintaining a network enhances credibility, attracts more members (increasing overall enrollment by 15% annually), and strengthens the plan's position in competitive markets by demonstrating a commitment to member health and satisfaction.
Compliance and Regulatory Adherence
Health insurance network participation requires strict adherence to compliance and regulatory standards mandated by governing bodies such as the Centers for Medicare & Medicaid Services (CMS) and state insurance departments. Organizations must maintain accurate documentation of network agreements, provider credentials, and claims processing protocols to ensure alignment with regulations. Additionally, training programs for staff on compliance recognition and reporting mechanisms are essential to mitigate risks associated with fraud, waste, and abuse within the healthcare system. Regular audits and assessments are necessary to verify ongoing compliance and identify any areas for improvement, preserving both network integrity and patient safety.
Contact Information and Next Steps
Health insurance networks play a crucial role in providing accessibility to quality medical services. Each network comprises a variety of providers, including primary care physicians, specialists, hospitals, and outpatient clinics. Participating in such networks allows healthcare providers to collaborate effectively, ensuring that patients receive comprehensive care. Interested providers must submit necessary documentation and credentials to the insurance company, highlighting their qualifications, specialties, and availability. Following submission, verification processes commence, assessing provider qualifications and ensuring compliance with network standards. Successful participation enables providers to expand their patient base, streamlining referrals and facilitating coordinated care within a designated service area. Updates about participation status or additional requirements are communicated through formal channels, ensuring clarity in the onboarding process.
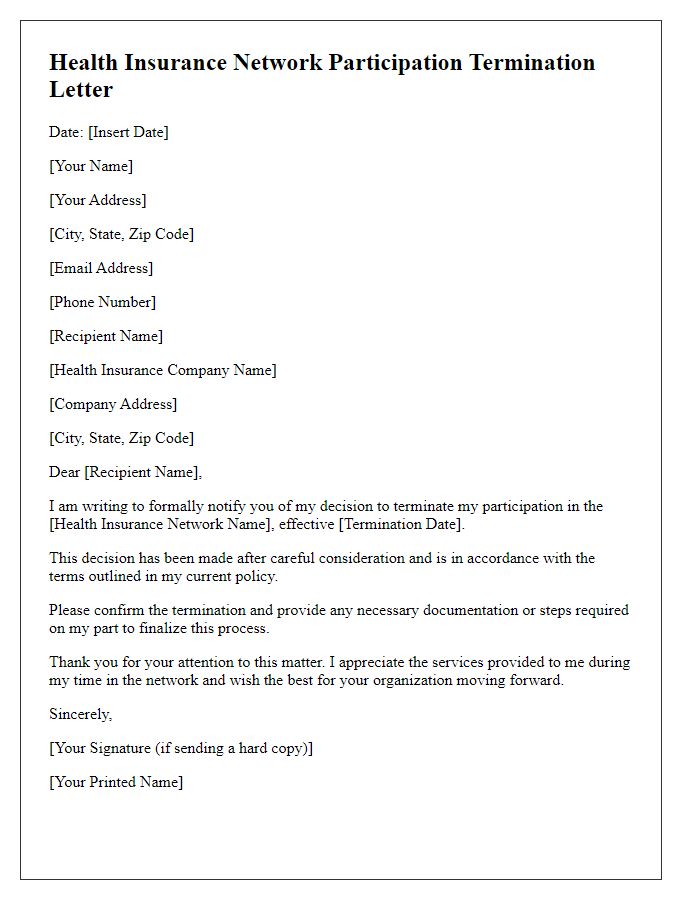
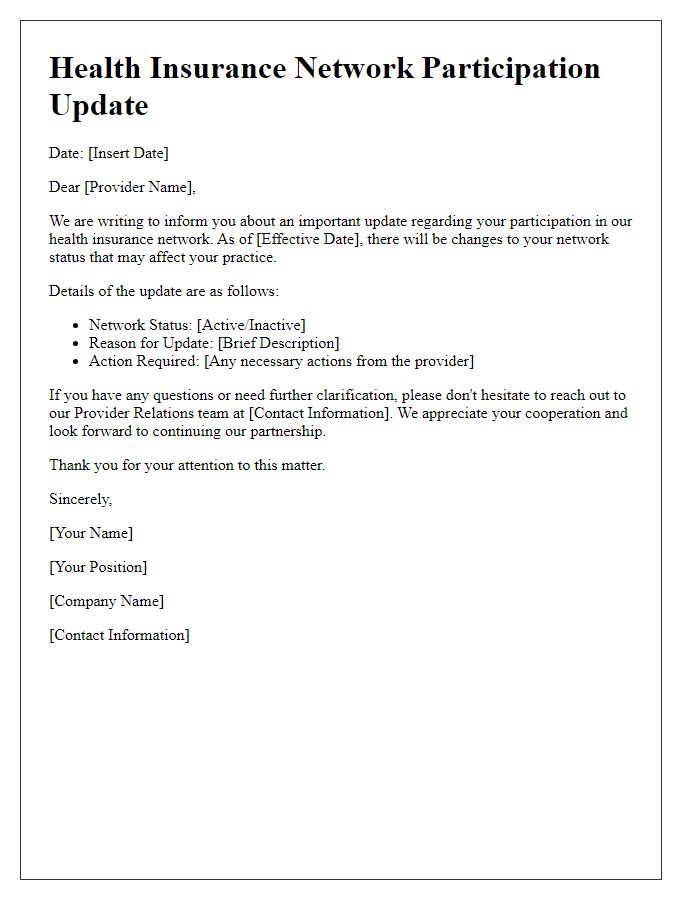
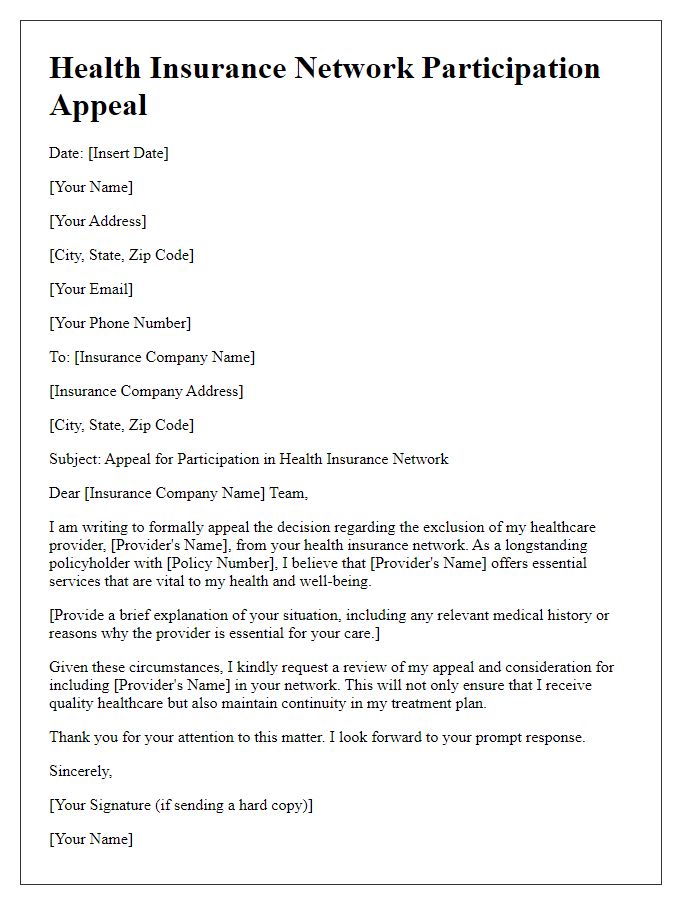
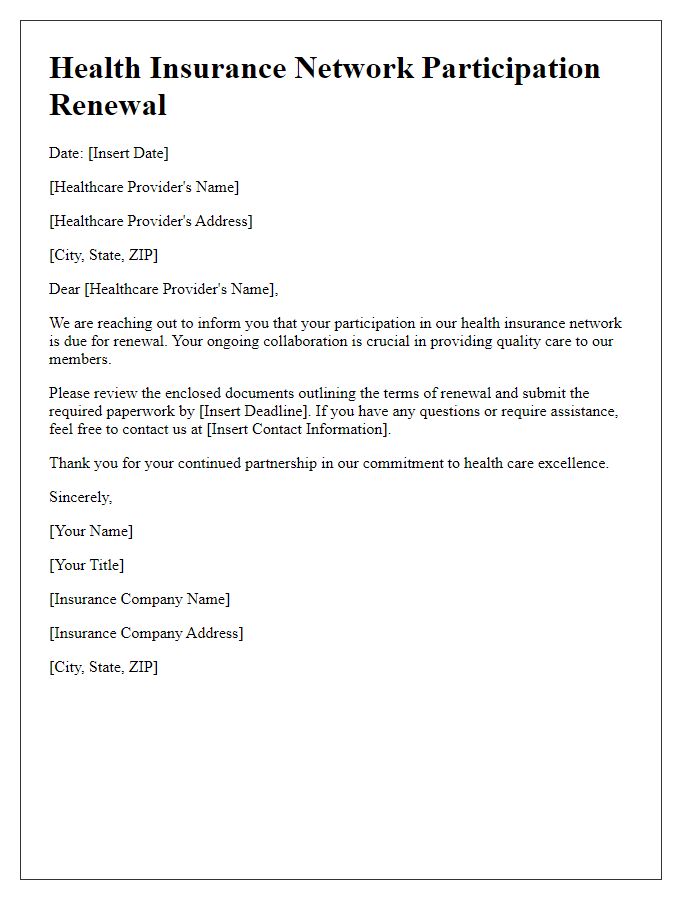
Letter Template For Health Insurance Network Participation Samples
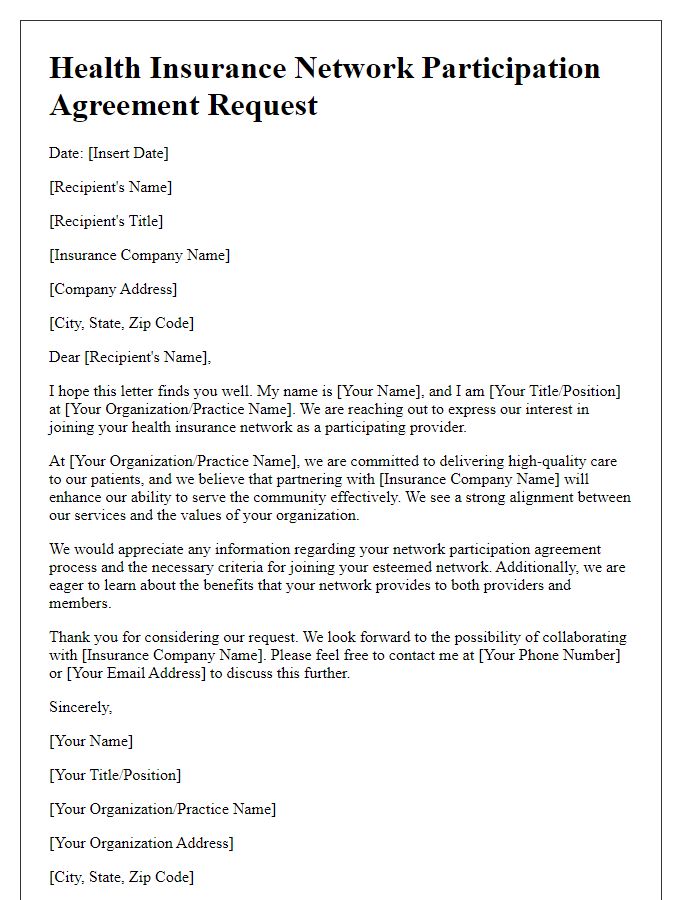
Letter template of health insurance network participation agreement request
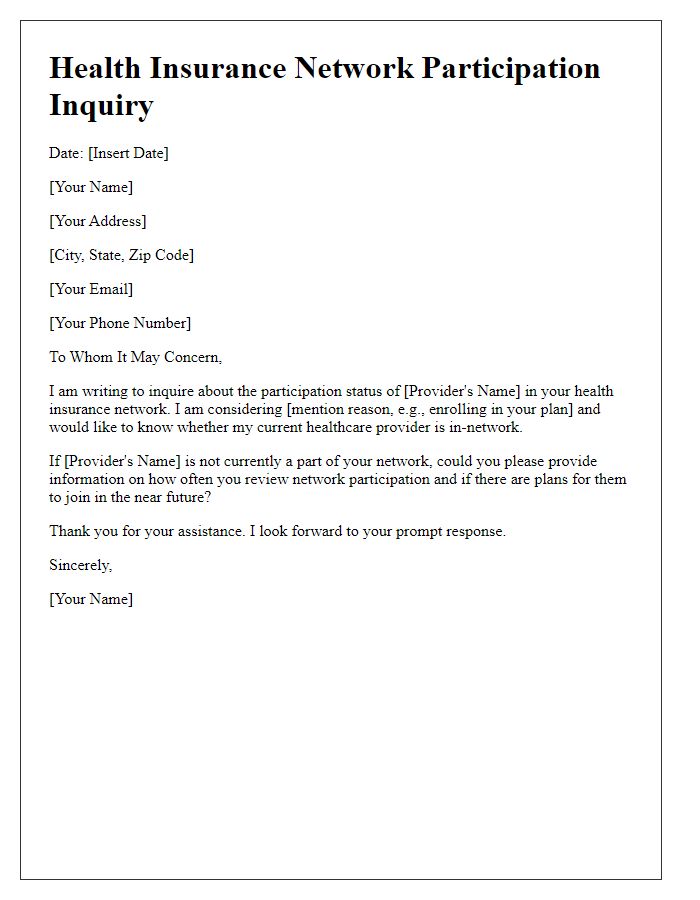
Letter template of health insurance network participation benefits explanation




Comments