Are you considering hormone therapy but feeling a bit overwhelmed by the risks involved? You're not alone, as many individuals face similar uncertainties when exploring their options. It's essential to have a comprehensive understanding of the potential benefits and drawbacks to make informed decisions about your health. Join us as we dive deeper into the critical aspects of hormone therapy risk assessment!
Patient Identification and Details
Hormone therapy risk assessment requires thorough patient identification and details to ensure personalized care. Key elements include patient demographics, such as age (critical for evaluating potential health risks), sex assigned at birth, and current gender identity for appropriate treatment, relevant medical history including previous hormonal treatments or surgeries, and existing health conditions like cardiovascular disease or diabetes that may impact therapy outcomes. Additionally, documenting family history of hormone-sensitive cancers, lifestyle factors like smoking or alcohol consumption, and current medications helps in assessing potential drug interactions. Proper identification ensures a tailored approach to hormone therapy, thereby enhancing patient safety and effectiveness of the treatment plan.
Purpose and Scope of Assessment
Hormone therapy risk assessment aims to evaluate the safety and potential complications associated with administering hormones, specifically estrogen, progesterone, or testosterone. This assessment targets individuals, typically within the age range of 18-65 years, seeking hormone replacement therapy for conditions such as gender dysphoria, menopause or hypogonadism. Key factors include medical history, current health status, family history of hormone-sensitive cancers, and lifestyle choices. The assessment process encompasses laboratory tests, such as hormone level evaluations and overall physical examinations. It serves to inform patients about potential risks, including cardiovascular issues, blood clots, and hormonal imbalance. This comprehensive evaluation ensures a personalized approach, aligning treatment with individual health profiles and minimizing adverse outcomes.
Medical History and Current Health Status
Chronic conditions such as hypertension (high blood pressure) or diabetes significantly impact the suitability of hormone therapy for patients. A comprehensive medical history review, highlighting any previous surgeries (e.g., hysterectomy, mastectomy), can reveal potential complications. Current health status, including body mass index (BMI) and laboratory results (cholesterol levels, liver function tests), aids in understanding the patient's overall risk profile. Additionally, family history of cardiovascular diseases or hormone-related cancers (e.g., breast cancer, prostate cancer) should be meticulously documented to assess hereditary risks associated with hormone treatment. Regular monitoring, including blood pressure readings and hormone levels, is crucial during therapy to ensure safe and effective management of side effects.
Potential Risks and Benefits of Hormone Therapy
Hormone therapy (HT), commonly used to manage symptoms associated with menopause or gender dysphoria, presents both potential risks and benefits worth considering. Benefits may include relief from hot flashes, improved mood stability, enhanced sexual function, and overall quality of life improvements. Specific medications, like estrogen or testosterone, can significantly alleviate discomfort associated with hormonal imbalances. On the other hand, potential risks include increased likelihood of cardiovascular events (such as heart attack or stroke), blood clots, and certain types of cancer (like breast or prostate cancer). Duration of therapy can also influence risk levels, making it vital for individuals to engage in thorough discussions with healthcare providers. Monitoring involves regular blood tests and check-ups to ensure that hormone levels remain within safe parameters and to evaluate the effectiveness of the treatment. An informed decision requires understanding individual health profiles, family histories, and personal values. Careful assessment facilitates safer pathways for those considering hormone therapy.
Informed Consent and Patient Understanding
Hormone therapy, commonly employed for gender transition or hormone imbalance treatment, carries several potential risks and benefits that are essential for patient understanding. Patients must be informed about cardiovascular risks, including increased likelihood of thrombosis or hypertension, especially in individuals over 35 years old. Breast development may occur, leading to changes in emotional well-being and body image perception. Additionally, metabolic changes can transpire, affecting weight management and cholesterol levels. Regular monitoring through blood tests for hormone levels and potential side effects is crucial, with follow-ups typically scheduled every three to six months. Patients should be aware of their treatment's legal and psychological implications, including the need for ongoing mental health support throughout therapy. Informed consent is vital, ensuring that patients fully comprehend their options and potential outcomes before commencing treatment.
Letter Template For Hormone Therapy Risk Assessment Samples
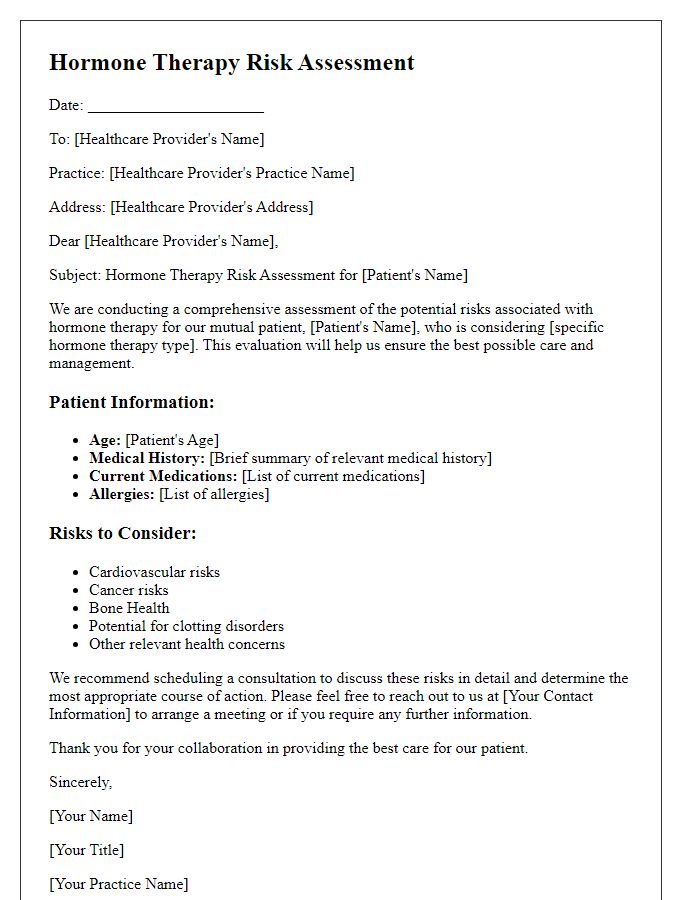
Letter template of hormone therapy risk assessment for healthcare providers.
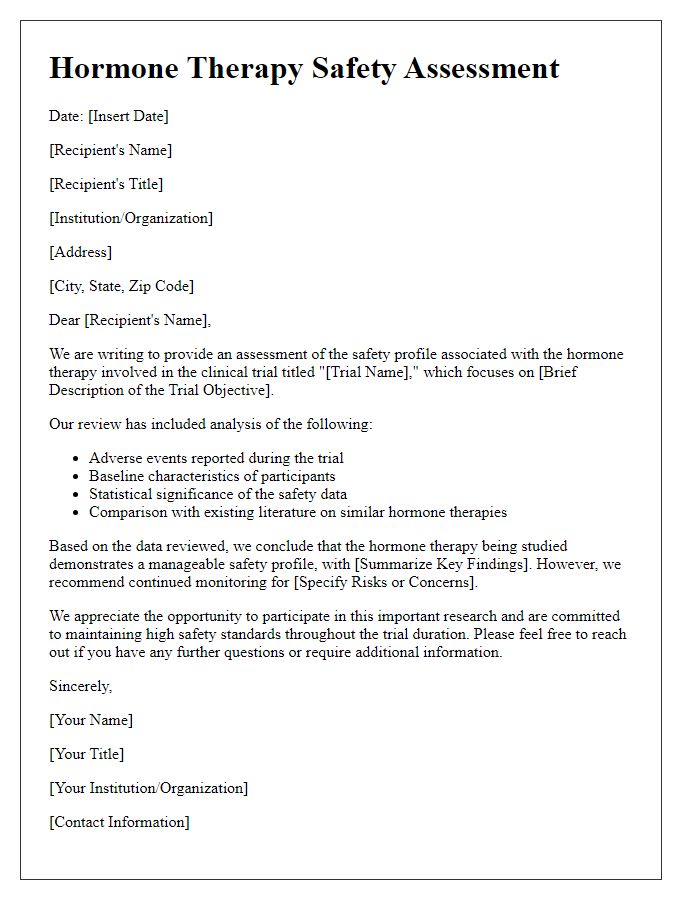
Letter template of hormone therapy safety assessment for clinical trials.
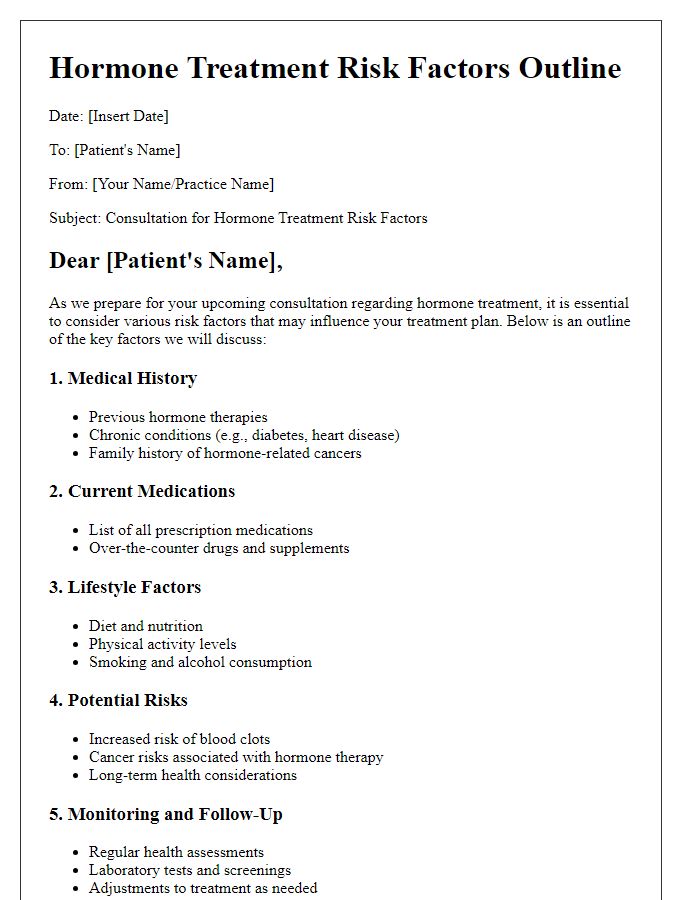
Letter template of hormone treatment risk factors outline for consultation.



Comments