Preparing for an endoscopy might seem daunting, but it doesn't have to be! Understanding what to expect and how to get ready can help ease your mind and ensure a smooth procedure. It's essential to follow the preparation instructions closely to ensure accurate results and a comfortable experience. To learn more about the specific steps you need to take before your endoscopy, keep reading!
Patient Information
Endoscopy preparations require patients to follow specific instructions to ensure a successful examination. Fasting is necessary, typically beginning 6 to 8 hours prior (no food or drink). Medications must be discussed with the healthcare provider, as some may need adjustments, especially anticoagulants (like warfarin) and diabetes medications (such as insulin). Patients should arrange for transportation to and from the facility, as sedation during procedures can impair driving. Recommended attire includes comfortable clothing, avoiding jewelry, watches, or contacts. An explanation of the procedure's purpose (such as gastrointestinal evaluation) enhances understanding and compliance, all crucial in achieving optimal results during the endoscopy.
Dietary Restrictions
Patients undergoing endoscopy procedures must adhere to specific dietary restrictions to ensure optimal results and safety. For at least 24 hours prior to the procedure, individuals should consume only clear liquids such as water, broth, and clear juices (without pulp), which help maintain hydration while minimizing residue in the digestive tract. Solid foods, especially high-fiber items like fruits and whole grains, should be avoided to reduce potential interference during the examination. Additionally, any medications, including blood thinners, should be discussed with healthcare providers, as adjustments may be necessary. It is crucial to adhere strictly to these guidelines to enhance the accuracy of the endoscopic evaluation.
Medication Guidelines
Patients undergoing endoscopy procedures should adhere to strict medication guidelines to ensure safety and effectiveness. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as Ibuprofen and Aspirin, should be discontinued at least 7 days prior to the procedure. Blood thinners, including Warfarin and Clopidogrel, may require special management; consult with a healthcare provider for specific adjustments. Medications for diabetes, such as Metformin, should be paused 48 hours before the procedure to minimize the risk of complications. Patients should also inform their physician of any over-the-counter supplements, particularly those containing fish oil or vitamin E, as these may increase bleeding risk. Clear communication about all medications, including dosages, is crucial to prevent adverse reactions during the endoscopy. Following these guidelines can contribute to a safer and more effective diagnostic or therapeutic procedure.
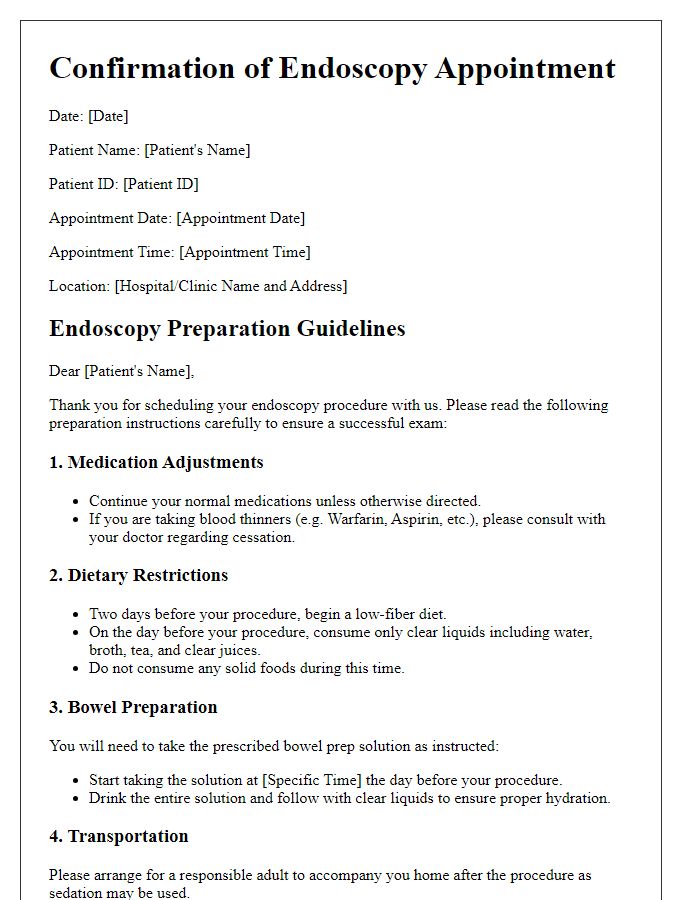
Appointment Details
Endoscopy preparation instructions are essential for ensuring a successful procedure. Patients are usually advised to stop eating solid foods at least eight hours prior to the appointment. Clear liquid consumption may be permitted until two hours before the scheduled time. For gastrointestinal endoscopies, it is crucial to follow bowel-cleansing instructions, often involving laxatives like polyethylene glycol, to ensure a clear view of the digestive tract. Specific medications, particularly blood thinners, may need to be adjusted, encouraging patients to consult their healthcare provider beforehand. The procedure typically takes place in specialized facilities equipped with advanced endoscopic technology, such as Olympus or Pentax devices, allowing for accurate diagnosis and treatment. Post-procedure observations often occur in recovery areas, with staff monitoring vital signs and patient comfort for a few hours before discharge.
Contact Information
Patients should ensure they have clear contact information for their healthcare provider prior to endoscopy, an important diagnostic procedure conducted in medical facilities. This includes the name of the gastroenterologist or specialist conducting the procedure. Office phone numbers (typically with specific area codes) should be noted for inquiries about preparation instructions or appointment confirmations. Additionally, the address of the medical center or hospital where the endoscopy will take place is crucial, including any relevant suite numbers or departments to avoid confusion on the day of the procedure. Emergency contact information or after-hours phone numbers may also be beneficial for addressing urgent concerns related to pre-procedural instructions or medications.
Letter Template For Endoscopy Preparation Instructions Samples
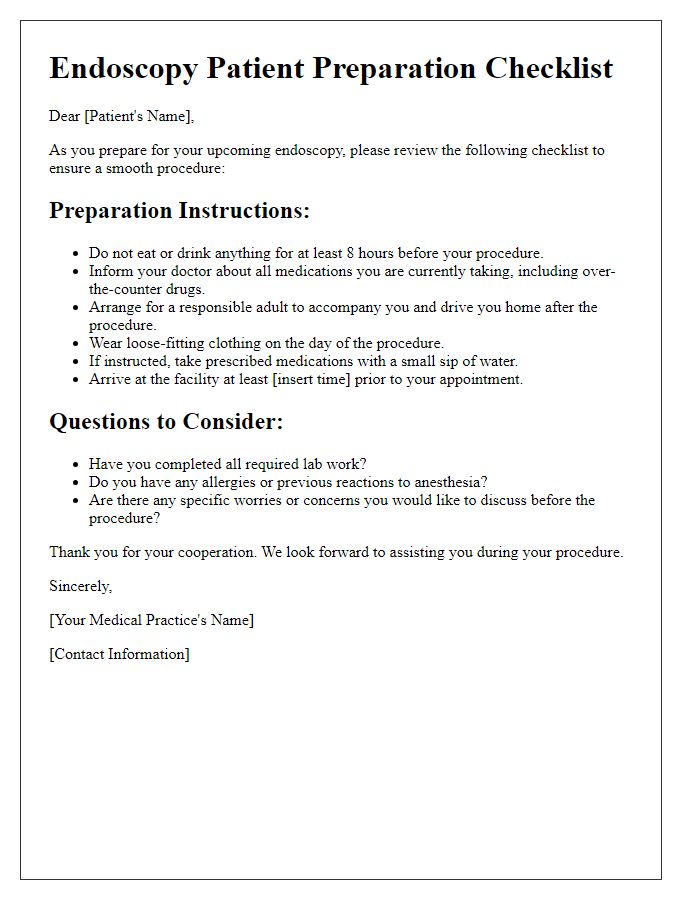
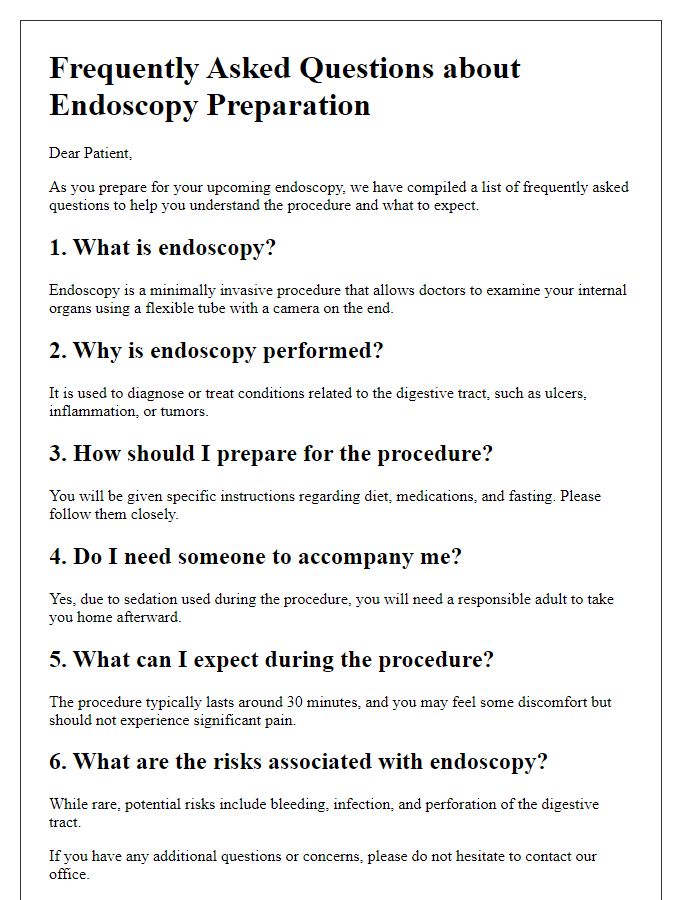
Letter template of endoscopy procedure prep instructions for healthcare providers.
Letter template of appointment reminder with prep instructions for endoscopy.
Letter template of personalized endoscopy prep instructions for specific conditions.


Comments