Are you curious about your options when it comes to contraception? Navigating the world of birth control can feel overwhelming with so many choices available. It's important to have a clear understanding of each method to make informed decisions that suit your lifestyle and health needs. Let's dive deeper into the various contraceptive options and help you find the perfect fit for your unique situationâread on to learn more!
Personal and Medical History
Personal and medical history plays a crucial role in contraception consultations. Women's health professionals typically gather comprehensive information to assess individual needs. Key factors include age (reproductive ages typically ranging from 15 to 49 years), medical conditions (like hypertension, diabetes, or migraines), and current medications (such as anticoagulants or hormonal therapies). Family history is also significant, particularly regarding conditions like breast cancer or thrombosis. Lifestyle choices, including smoking status and frequency of alcohol consumption, can influence contraceptive options. Additionally, any previous experiences with contraceptive methods, including side effects or preferences, help tailor recommendations for effective and safe contraception.
Contraceptive Options Overview
A comprehensive contraceptive consultation provides essential information about various birth control methods available for individuals seeking to manage their reproductive health. Common options include hormonal methods such as birth control pills (oral contraceptives taken daily), contraceptive patches (worn on the skin and changed weekly), and long-acting reversible contraception (LARCs) like intrauterine devices (IUDs), which can provide protection for several years. Barrier methods, including male condoms (effective against STIs and pregnancy) and female condoms, are also popular choices. Additionally, permanent solutions like tubal ligation and vasectomy can be considered for those who do not want children in the future. Understanding effectiveness rates, side effects, and personal health factors is crucial in making an informed decision. Seeking guidance from a healthcare professional ensures personalized advice tailored to individual needs and lifestyle.
Discussion of Benefits and Risks
In the context of contraception consultation, understanding the benefits and risks associated with various methods is essential for informed decision-making. Hormonal contraceptives, such as the combined oral contraceptive pill, can provide effective pregnancy prevention (over 99% efficacy with perfect use) while regulating menstrual cycles and alleviating acne. However, potential risks include increased blood clotting (thrombosis) and side effects like nausea or mood changes. Additionally, long-acting reversible contraceptives (LARCs), like intrauterine devices (IUDs), offer prolonged protection (3 to 10 years, depending on the type) and require minimal maintenance. Risks associated with IUDs may include pelvic inflammatory disease (PID) and discomfort upon insertion. Barrier methods, such as condoms, not only prevent pregnancy but also protect against sexually transmitted infections (STIs), though they have lower efficacy rates (approximately 85% with typical use). Each method's suitability depends on individual health profiles, lifestyle preferences, and long-term reproductive goals. Factors such as age, medical history, and lifestyle should guide the discussion to ensure optimal contraceptive choices.
Individualized Recommendations
Contraceptive options provide individuals with the ability to manage reproductive health effectively. Hormonal methods, including birth control pills, patches, and implants, offer convenience through monthly or long-term contraception. Barrier methods like condoms and diaphragms require user action at the time of intercourse, ensuring immediate effectiveness. Intrauterine devices (IUDs), placed by healthcare professionals, can offer protection against pregnancy for several years. Natural family planning relies on tracking menstrual cycles and fertility signs, promoting awareness of reproductive patterns. Emergency contraception, such as the morning-after pill, is crucial for preventing unintended pregnancies after unprotected intercourse. Individual health factors, medical history, and lifestyle choices play significant roles in determining the most suitable method of contraception. Regular consultations with healthcare professionals ensure tailored recommendations and empower individuals to make informed decisions about their reproductive health.
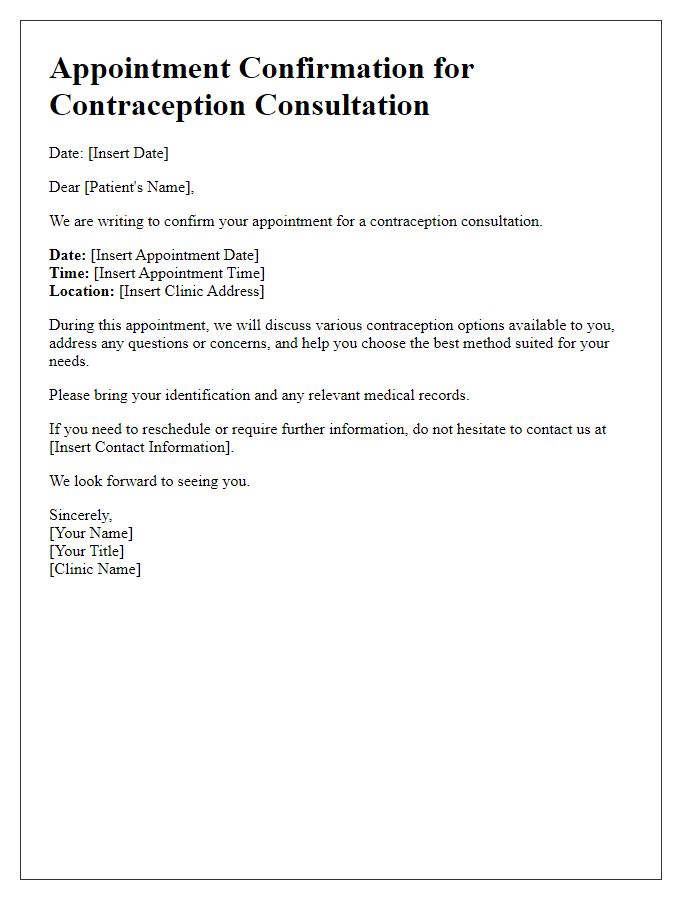
Follow-up and Monitoring Plan
A comprehensive follow-up and monitoring plan for contraception consultations ensures effective management and patient satisfaction. Regular appointments, typically scheduled every three to six months based on the contraceptive method, are essential for assessing side effects, such as mood changes or weight fluctuations that may occur with hormonal methods like birth control pills or implants. Blood pressure checks (with a focus on levels exceeding 140/90 mmHg) are critical for patients using methods containing estrogen, like the combined oral contraceptive pill, to prevent potential cardiovascular risks. Screening for sexually transmitted infections (STIs) should be considered during follow-ups, particularly for IUD users. Educational resources regarding proper usage and troubleshooting (e.g., addressing issues like missed pills) enhance patient confidence. Additionally, personalized discussions about maintaining adherence to the contraceptive regimen support overall reproductive health. For patients considering future pregnancies, consultations can address fertility restoration timings and transition strategies.



Comments