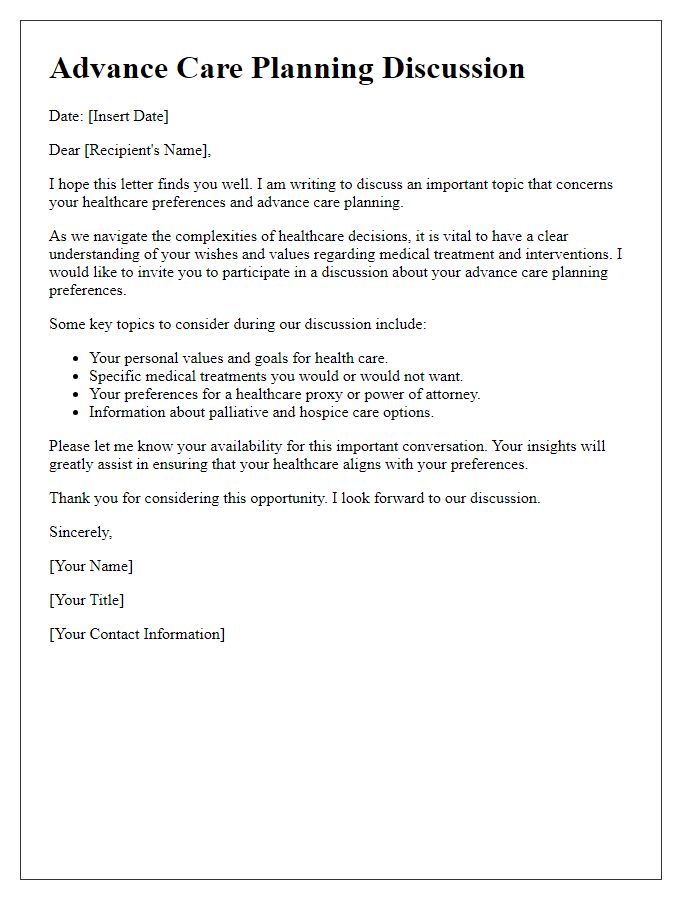
In today's fast-paced world, planning for the future is more important than ever, especially when it comes to making decisions about healthcare. An advanced directive is a powerful tool that ensures your wishes are respected, even when you can't voice them yourself. Crafting such a document may seem daunting, but it can provide peace of mind for you and your loved ones. So, let's dive into the nuances of advanced directive planning and explore how you can take charge of your health decisions moving forward!
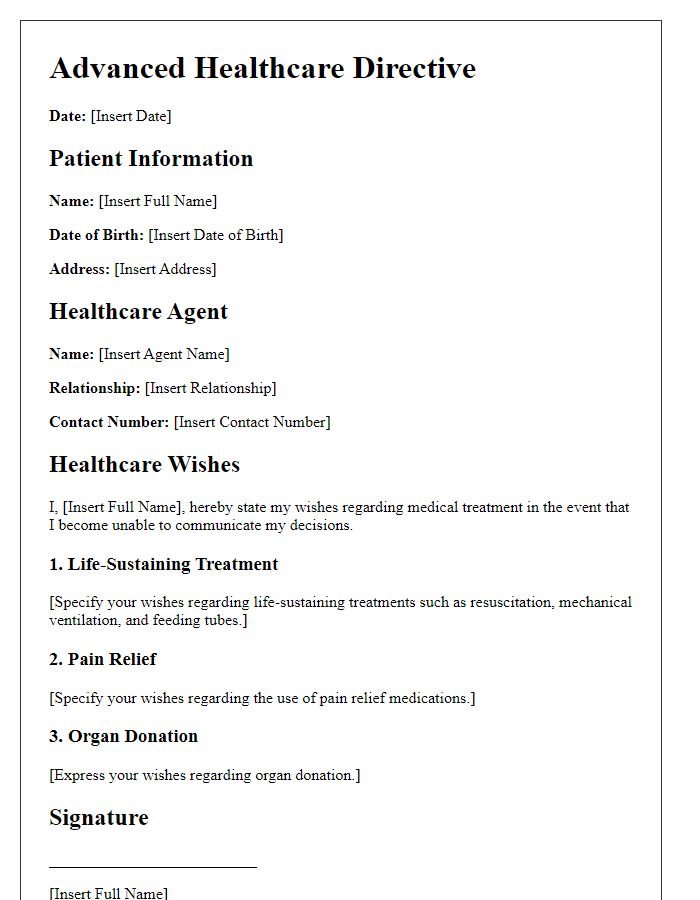
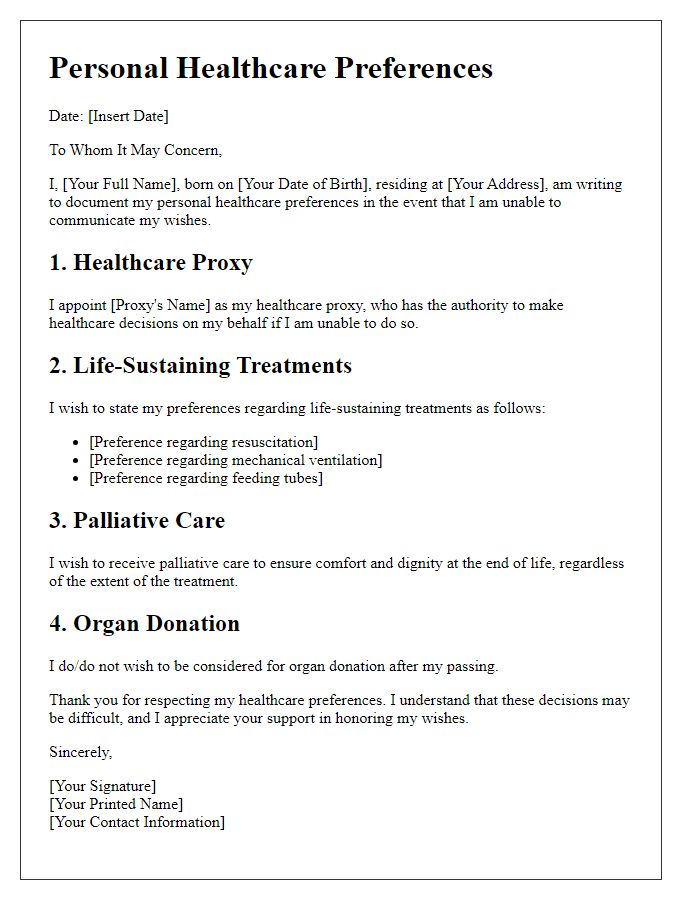
Personal Identification Information
Personal identification information is crucial in advanced directive planning. Individuals, such as adults over 18, should include full legal names, residential addresses (including city and state), and contact numbers (home, mobile) for clear identification. Additionally, date of birth helps ascertain age, while Social Security numbers (optional) provide unique identification. Emergency contacts, including names and phone numbers of family members or trusted friends, are essential for communication during medical emergencies. It is also advisable to document healthcare providers' information, such as names and practice locations, to facilitate seamless access to medical history and previous treatments, ensuring informed decision-making.
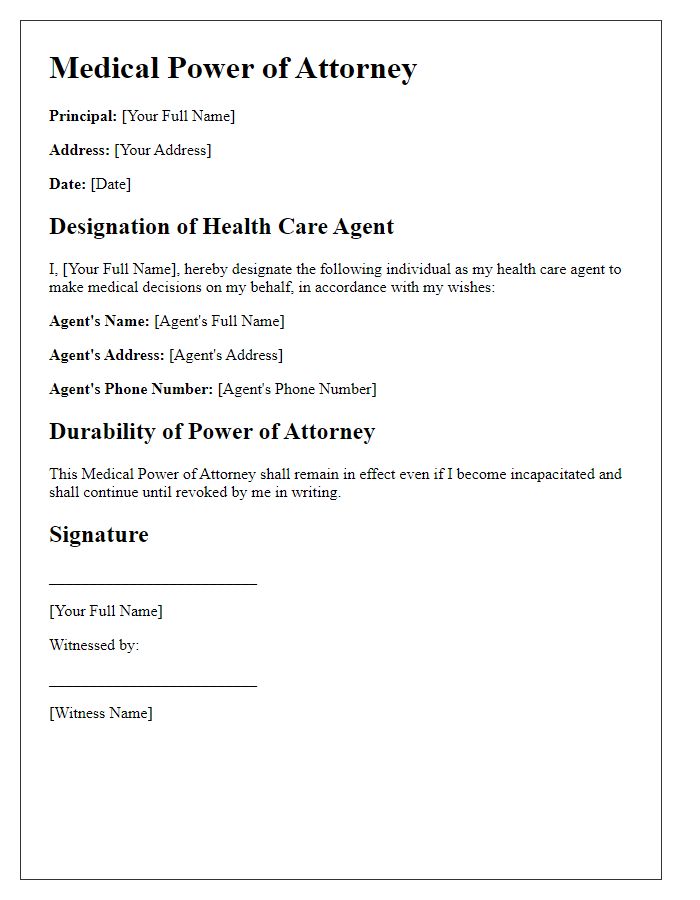
Health Care Agent Designation
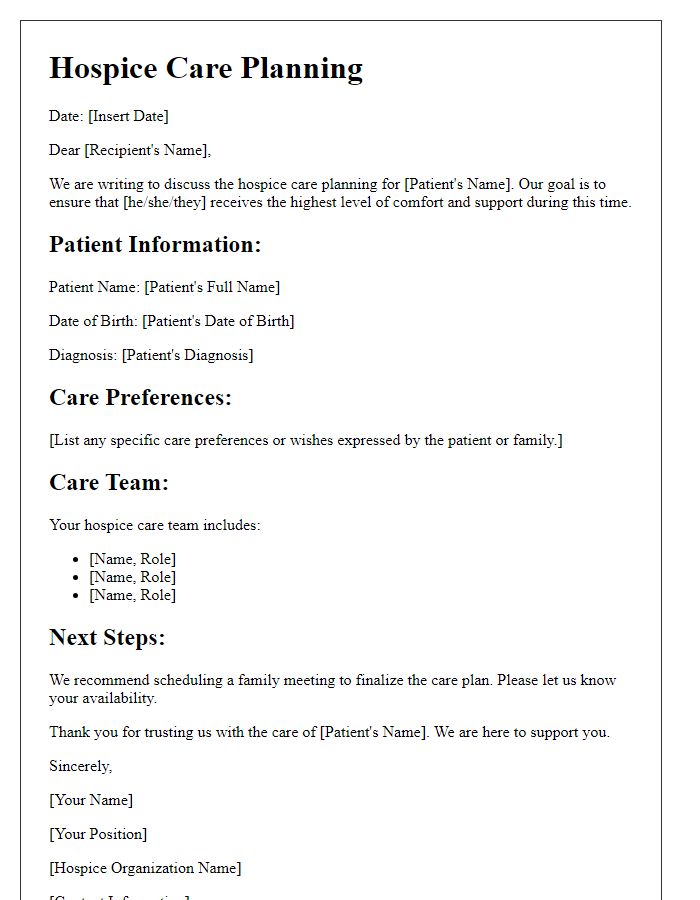
Advanced healthcare directives serve as crucial legal documents that empower individuals to designate a health care agent, ensuring that their medical decisions are respected when they can no longer communicate their wishes. This document, often structured to comply with state regulations and statutes, outlines specific preferences regarding medical procedures and end-of-life care, providing guidance in critical situations. The chosen health care agent, typically a trusted family member or close friend, should fully understand the individual's values and desires, particularly in circumstances such as terminal illness or incapacitating injuries. Beyond mere designation, these directives can encompass detailed instructions related to do-not-resuscitate (DNR) orders, life-sustaining treatments, and hospice care options, tailored to reflect personal beliefs and cultural considerations surrounding health and mortality. It is essential that individuals regularly review and update their directives to ensure alignment with their current wishes, especially after significant life events such as marriage, divorce, or the birth of a child.
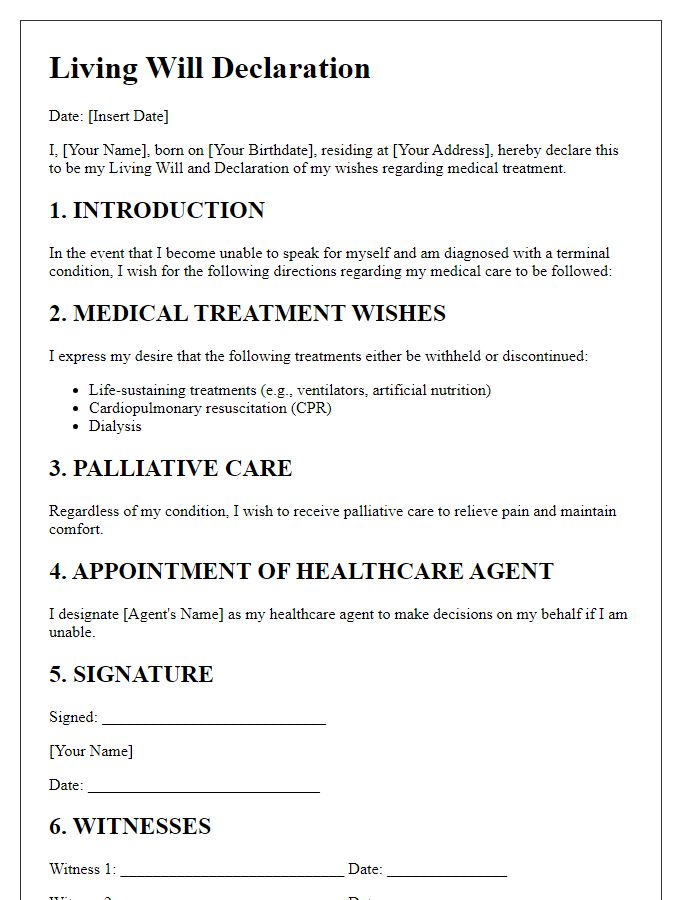
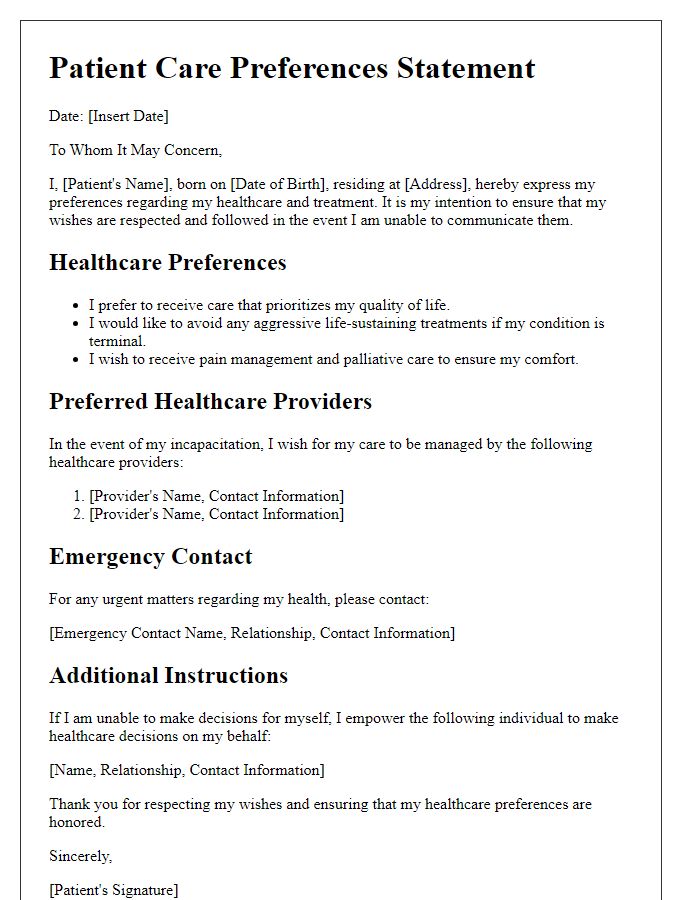
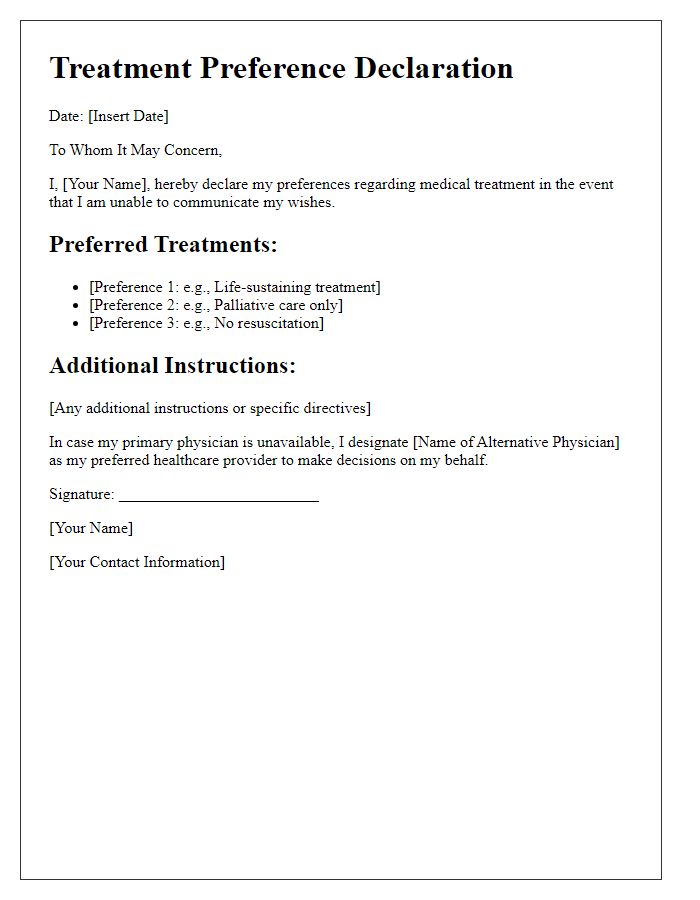
Treatment Preferences
An advanced directive outlines treatment preferences for individuals facing medical decisions in critical situations. This document allows patients to specify their desires regarding life-sustaining treatments, such as mechanical ventilation, resuscitation, and feeding tubes, particularly in scenarios of terminal illness or incapacitation. Patients can detail their wishes, ensuring that healthcare providers respect their choices, such as opting for palliative care, which focuses on comfort, rather than aggressive interventions. This legal instrument, often recognized in all 50 states of the USA, serves as a crucial communication tool for families and medical staff, clarifying the individual's values and wished-for quality of life during serious health crises. It ultimately aims to alleviate the burden of decision-making on loved ones during emotionally charged moments.
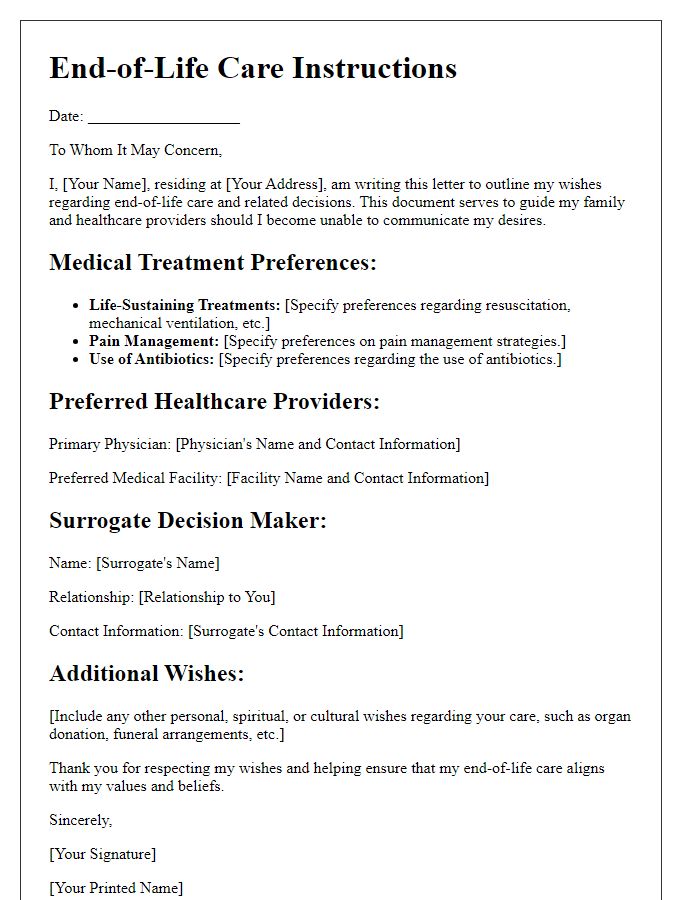
End-of-Life Wishes
An advanced directive planning letter template serves as a vital document, guiding individuals in articulating their end-of-life wishes. This structured framework encompasses essential components such as healthcare preferences, appointed decision-makers, and specific medical treatments to either pursue or decline. Clarity in language empowers patients, ensuring their values and desires are honored during critical moments. Utilizing this template, individuals can address various scenarios, from resuscitation efforts to pain management options, ultimately fostering peace of mind for both the individual and their loved ones. Such thorough preparation aids healthcare professionals in making informed decisions aligned with the patient's intentions, thereby enhancing the overall caregiving experience in sensitive times.
Signatures and Witnesses
Advanced directive planning involves outlining specific healthcare preferences, ensuring that decisions are made according to an individual's wishes during critical medical situations. The signing process requires two witnesses who must be present to confirm the individual's intent and understanding of the document. Witnesses must be qualified, typically not being family members or individuals with financial interests in the individual's estate, thereby maintaining objectivity. Each witness must sign and date the document, providing their full names, addresses, and contact information to verify their identity. Proper execution of these signatures and witnesses is crucial to uphold the legality and enforceability of the advanced directive in medical settings.


Comments