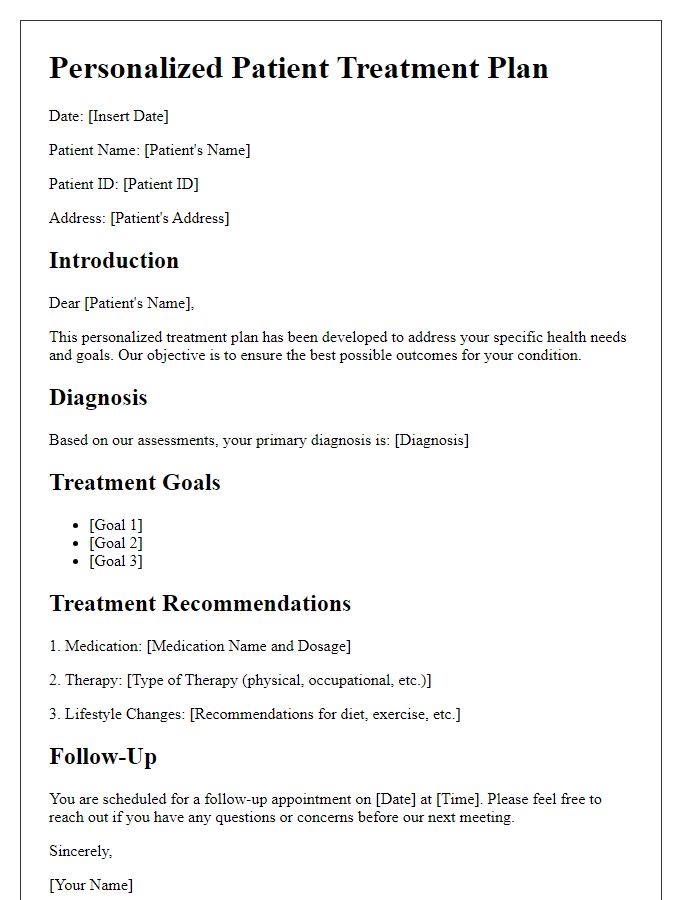
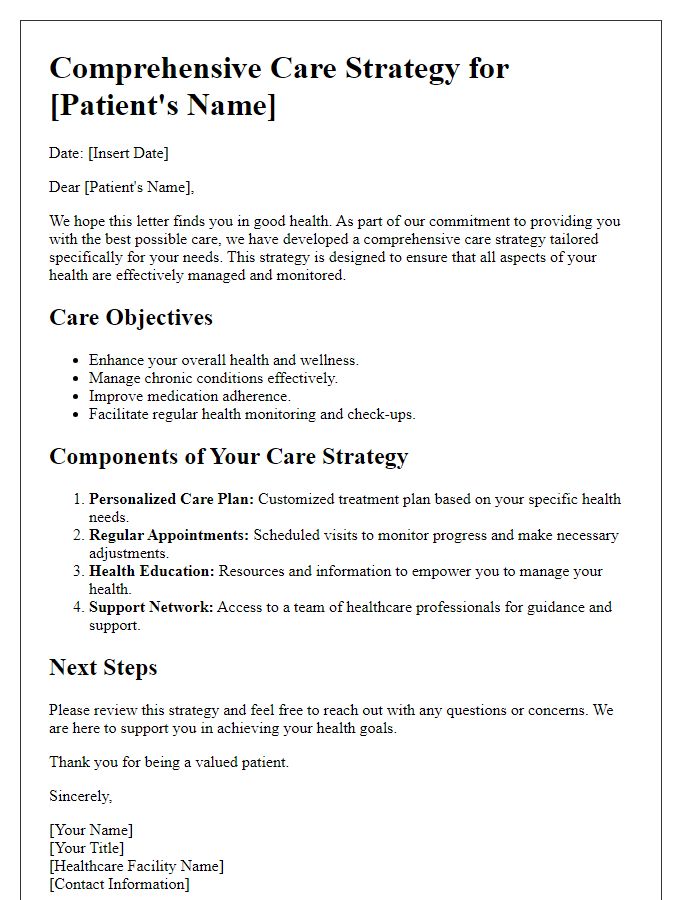
Creating a letter template for a patient treatment plan can be a valuable tool in healthcare communication. This document not only outlines the specifics of the treatment but also fosters clarity and understanding between the healthcare provider and the patient. By using clear language and a structured format, patients are more likely to feel informed and engaged in their care journey. Ready to dive deeper into crafting the perfect treatment plan letter? Keep reading!
Patient Identification Details
Patient identification details consist of critical elements such as full name, including middle name for clarity, date of birth (e.g., January 1, 1980), gender (male or female), and unique identification number (patient ID or medical record number). Address information, including street, city, state, and zip code (e.g., 123 Main St, Springfield, IL, 62701), ensures accurate communication. Contact details, including phone number (such as home and mobile numbers), and email address enhance reachability for appointment scheduling and follow-ups. Insurance information should also be incorporated, detailing provider name, policy number, and group number, allowing for seamless billing and claims processing. Finally, emergency contact information is essential, listing full name, relationship to patient, and phone number to ensure timely assistance in urgent health situations.
Diagnosis and Medical History
The treatment plan for patients diagnosed with Type 2 Diabetes Mellitus outlines critical components for effective management. This condition, prevalent in over 462 million individuals globally, is characterized by insulin resistance and high blood sugar levels. Medical history typically includes comorbidities such as hypertension, affecting approximately 50% of diabetes patients, and dyslipidemia. The patient may have a history of cardiovascular diseases, which are significant risk factors, contributing to increased mortality rates. Regular monitoring through HbA1c tests, which track average blood glucose over three months, is essential. Lifestyle changes are imperative, including diet modification to a low-glycemic index regimen and consistent physical activity, recommended at least 150 minutes weekly. Medication options, such as Metformin, aimed at lowering blood glucose levels, are common first-line treatments. Regular follow-up appointments in a healthcare setting, ideally every three months, will ensure adherence to treatment protocols and adjust plans based on individual progress.
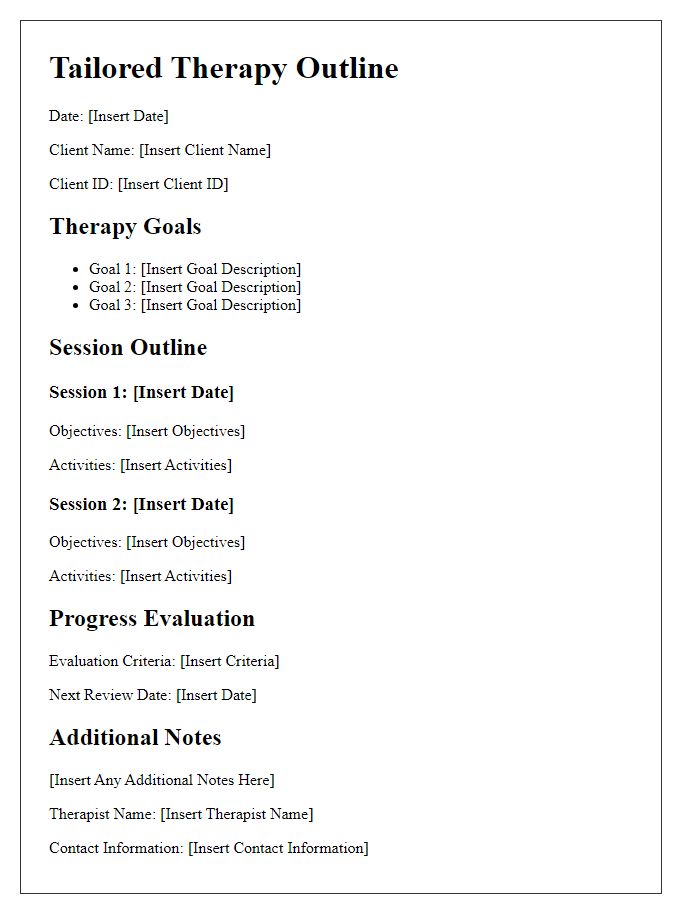
Treatment Goals and Objectives
A comprehensive treatment plan for patients focuses on specific goals and measurable objectives to guide their recovery process. Individualized goals can include reducing pain levels (targeting a decrease of 2 points on a 10-point scale within four weeks), improving mobility (aiming for a 20% increase in range of motion in affected joints within two months), and enhancing overall well-being (through regular assessment of mood and anxiety levels utilizing standardized scales like the Beck Depression Inventory). Objectives may involve attending physical therapy sessions twice a week at the local clinic, completing assigned home exercises daily for at least 30 minutes, and participating in support group meetings to foster community connections. Regular follow-ups, monitoring vital signs, and adjustments to the treatment approach ensure that goals remain achievable and relevant to the patient's evolving needs.
Proposed Treatment Interventions
Proposed treatment interventions for patients with chronic pain include a multidisciplinary approach. Physical therapy sessions, typically lasting 60 minutes and conducted twice a week, focus on strengthening exercises and flexibility training to enhance mobility. Pain management strategies, such as cognitive-behavioral therapy (CBT), aim to address psychological aspects and coping mechanisms, usually scheduled weekly. Medication adjustments may include non-steroidal anti-inflammatory drugs (NSAIDs) or opioids, with monitoring for effectiveness and side effects. Additionally, regular follow-up appointments every four weeks will assess progress and make necessary modifications to the treatment plan, ensuring a holistic and patient-centered approach to pain management.
Monitoring and Follow-up Schedule
A comprehensive monitoring and follow-up schedule is vital for managing chronic conditions effectively. Regular appointments, typically every four to six weeks, allow healthcare providers to assess symptoms and medication efficacy. For instance, diabetic patients should have blood glucose levels tested regularly, ideally before meals and at bedtime. Telehealth sessions provide convenience for patients living in remote areas while ensuring consistent monitoring. Additionally, lab tests, such as A1C levels for diabetes, should be conducted every three months to gauge long-term management. Keeping an updated medication list enhances medication adherence, which is crucial for treatment success. This structured schedule ensures timely interventions, contributing to improved patient outcomes.


Comments