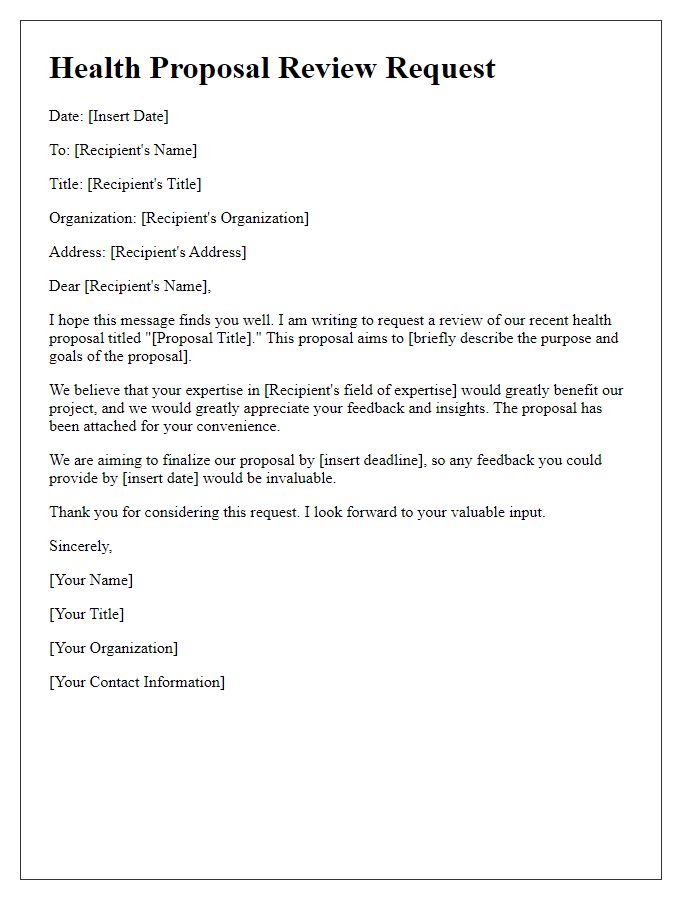
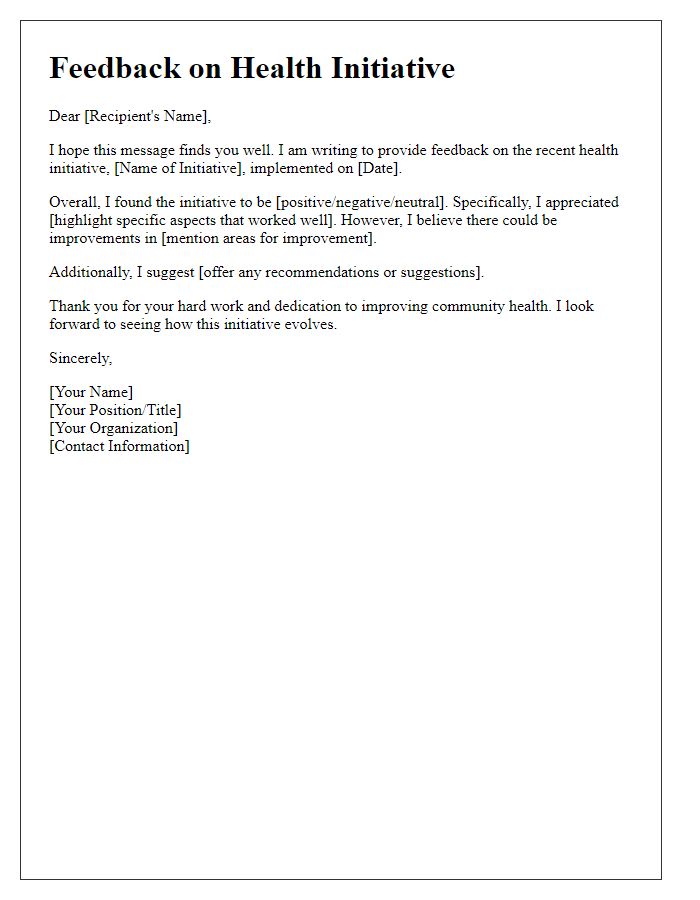
Are you looking to enhance your health proposal evaluation skills? Navigating the complexities of assessing health initiatives can be daunting, but with the right framework and understanding, you can make impactful decisions. In this article, we'll explore essential tips and best practices to streamline the evaluation process and ensure your proposals align with desired health outcomes. Ready to dive deeper into the world of effective health proposal evaluation? Let's get started!
Clear objective statement
A health proposal evaluation ensures that project objectives align with public health goals, such as reducing obesity rates in specific communities (for example, targeting a 10% decrease in the urban population of Houston by 2025). This involves assessing program effectiveness, cost-effectiveness, and community impact while adhering to behavioral frameworks such as the Social Ecological Model. Evaluators must rigorously analyze data collected from surveys and health metrics, using statistical tools to measure significant changes in health behaviors or outcomes. A clear objective statement forms the backbone of this evaluation, guiding stakeholders through specific, measurable goals like improving physical activity levels among middle school students by 15% within the first year of implementation.
Comprehensive background
A comprehensive background in a health proposal evaluation includes an analysis of the healthcare system's structure, relevant health statistics, and existing policies. Health disparities (inequities in health status or healthcare access) among populations in specific regions, such as the southern United States, often impact the effectiveness of health interventions. For example, an examination of diabetes prevalence rates shows a staggering 12.5% among African American adults, highlighting the need for targeted initiatives. Moreover, understanding existing healthcare programs, such as Medicaid and Medicare, along with state-specific regulations, provides context for evaluating proposed solutions. Key stakeholders, including local health departments and community organizations, play vital roles in implementing health initiatives. Overall, a thorough evaluation demands a multi-faceted approach that encompasses both quantitative data (such as hospital admission rates) and qualitative insights (like patient satisfaction surveys).
Evidence-based research
Evidence-based research plays a crucial role in evaluating health proposals, particularly in understanding the effectiveness of interventions. Comprehensive studies, such as randomized controlled trials (RCTs) and meta-analyses, provide substantial data regarding outcomes. Parameters like sample size, control groups, and statistical methods underpin the validity of findings. When assessing proposals, it is essential to examine the quality of evidence, often rated using systems like the GRADE (Grading of Recommendations Assessment, Development, and Evaluation). Thorough review of existing literature, including journals such as The Lancet and the Journal of the American Medical Association, informs the decision-making process. By integrating empirical data and clinical expertise, stakeholders can ensure health proposals are poised for successful implementation and measurable impact.
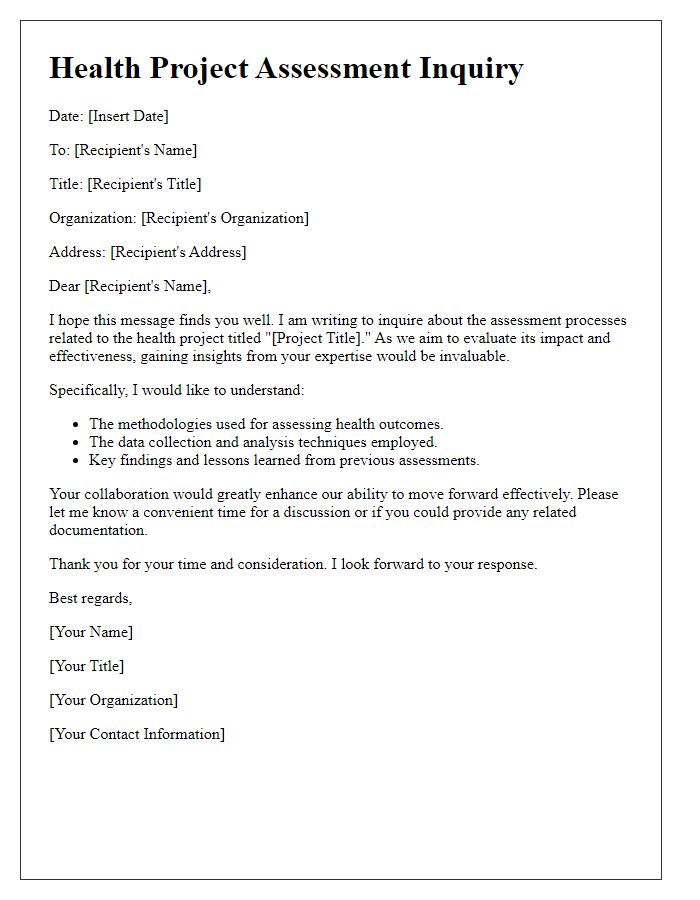
Detailed methodology
The detailed methodology for evaluating a health proposal involves structured steps designed to ensure comprehensive analysis and effective implementation. Phase one includes a literature review of relevant studies conducted between 2010 and 2023, focusing on over 200 peer-reviewed articles about similar health interventions targeting chronic diseases like diabetes and hypertension. Phase two entails stakeholder engagement, involving consultations with community health workers, local government officials from the Health Department, and relevant NGOs, ensuring at least five stakeholder meetings to gather diverse perspectives. Phase three integrates data collection through surveys administered to a sample size of 500 participants within identified demographics, such as age groups 30-50, ensuring a response rate of over 70%. Phase four encompasses quantitative analysis of the data using statistical software like SPSS to identify trends and outcomes, supplemented by qualitative interviews with at least 30 participants to gain deeper insights. The fifth phase focuses on disseminating the findings through community forums and presentations to the local health council, aimed at developing actionable recommendations based on a comprehensive evaluation of the health proposal's impact on community wellness.
Measurable outcomes
Measurable outcomes in health proposals are essential for assessing the impact of interventions on public health. Specific metrics, such as reduction in incidence rates (per 100,000 population) of chronic diseases like diabetes and hypertension, provide clear indicators of success. Additionally, patient satisfaction scores (using validated surveys) can gauge the quality of care received at healthcare facilities. Tracking hospital readmission rates (percentage within 30 days of discharge) can identify the effectiveness of discharge planning processes. Furthermore, implementation of preventive screenings (like mammograms and colonoscopies) increases early detection and can be quantified by participation rates (percentage of eligible populations screened). Cost-effectiveness analyses (comparing intervention costs to outcomes achieved) also offer valuable insights into the economic viability of health proposals. Monitoring these outcomes over a defined timeline allows for continuous improvement and accountability in public health initiatives.


Comments