If you've ever felt uneasy about changes in your medication prescription, you're not alone. Navigating the complex world of healthcare can be daunting, especially when it comes to managing your medications. It's essential to voice your concerns and seek clarity, ensuring that any adjustments made truly serve your best interests. In this article, we'll explore how to effectively contest changes in your medication prescription and advocate for your healthâso keep reading to learn more!
Patient Information
Contesting changes in medication prescriptions requires a thorough understanding of both the medical implications and the patient's unique situation. Patients often experience significant side effects or changes in their health outcomes when medication adjustments occur. For instance, switching from a generic to a brand-name medication (such as from lisinopril to Prinivil) could influence effectiveness or price, impacting patient adherence. Additionally, specific dosages (e.g., 10 mg vs. 20 mg) may trigger different physiological responses, necessitating careful consideration. It is crucial to document instances of adverse reactions or health improvements following initial treatments, such as Measurement of blood pressure levels, cholesterol counts, or mental health assessments. Evidence-based arguments, including medical studies or guidance from reliable institutions like the American Medical Association, can strengthen the case against unwarranted prescription changes.
Prescription Details
Contesting changes in medication prescription can be crucial for patients experiencing adverse effects. The prescription detail (such as Medications XYZ and ABC) should include the active ingredients, dosages (e.g., 10 mg for XYZ), and the frequency of administration (once daily). Important contextual factors include the patient's medical history, such as previous allergies or reactions to certain medications (like rash or nausea), and current health conditions (e.g., diabetes or hypertension). Any changes proposed by the healthcare provider, including the introduction of new medications (e.g., Medication DEF), must be scrutinized. The potential for interactions (e.g., between XYZ and DEF) or side effects should be documented to highlight concerns. A clear request for a review or re-evaluation based on evidence or documented experiences should be articulated, emphasizing the need for patient-centered care.
Reason for Contesting
Medication changes can significantly impact patient well-being and health outcomes, particularly in chronic conditions like diabetes or hypertension. Inaccurate dosages may lead to complications, such as hyperglycemia or elevated blood pressure. Additionally, factors like age (for example, elderly patients over 65) or concurrent medications can heighten the risk of adverse effects. Prior medication history can illustrate patient tolerance or allergies, informing the necessity of maintaining an established prescription. Documented studies indicate that abrupt changes in medication can lead to increased hospitalizations (over 20% in some demographics) and adverse reactions. Therefore, it is crucial to review the reasoning behind any alterations in prescribed medication closely.
Supporting Evidence
In medical practice, changes in medication prescriptions can significantly impact patient health outcomes. The process of contesting these alterations often requires robust supporting evidence, including clinical studies, patient records, and expert testimonies. For instance, a 2021 study published in the Journal of Clinical Medicine highlighted that abrupt changes in antihypertensive drugs led to increased hospitalization rates among individuals aged 65 and older. Furthermore, patient records from medical facilities like Johns Hopkins Hospital can provide historical data on how specific medications improve patient quality of life. Consulting with specialists, such as cardiologists or endocrinologists, may bolster the argument against unwarranted changes and underscore the necessity of adhering to proven treatment protocols.
Request for Review
Patients experiencing unexpected changes in medication prescription often face significant challenges in managing their health conditions. These alterations might occur due to insurance adjustments, pharmacy policies, or physician updates. For instance, a switch from a long-used medication like Metformin, commonly prescribed for type 2 diabetes, to a newer, less familiar alternative can induce confusion and anxiety. Specific concerns might arise regarding the efficacy of the new drug, potential side effects, or proper dosage adjustments. Healthcare providers, such as endocrinologists or primary care physicians, play a crucial role in guiding patients through these changes, ensuring that continuity of care is maintained. Effective communication with healthcare professionals is essential for patients to express their concerns and seek a comprehensive review of prescribed medications, promoting better health outcomes.
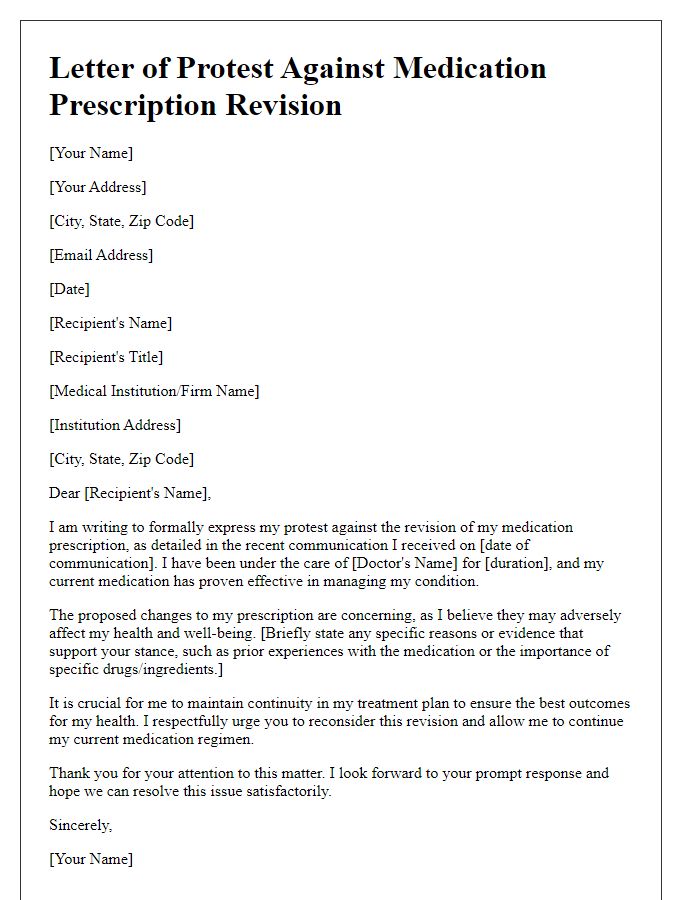
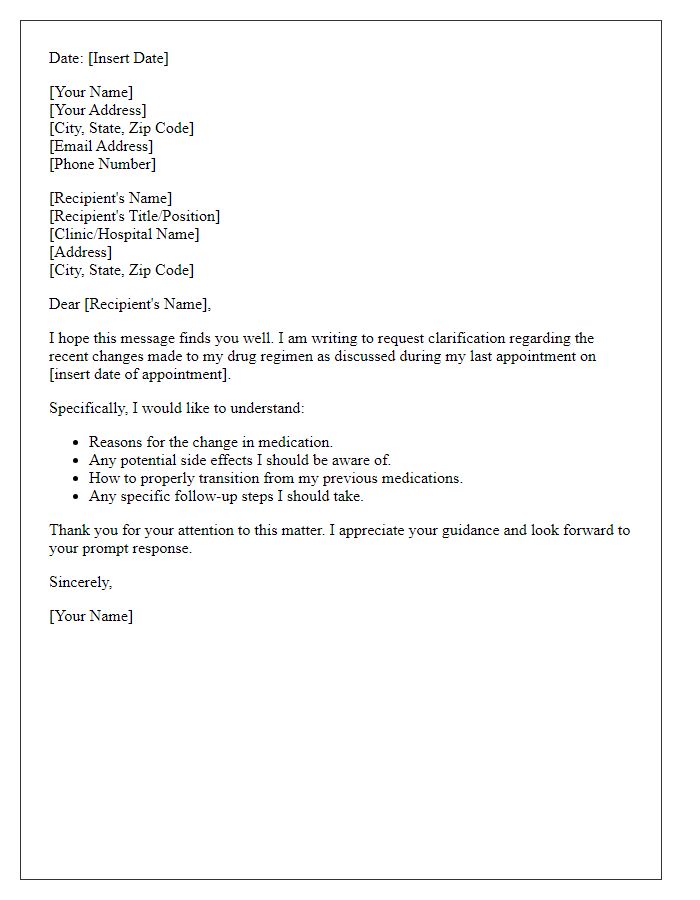
Letter Template For Contesting Changes In Medication Prescription Samples
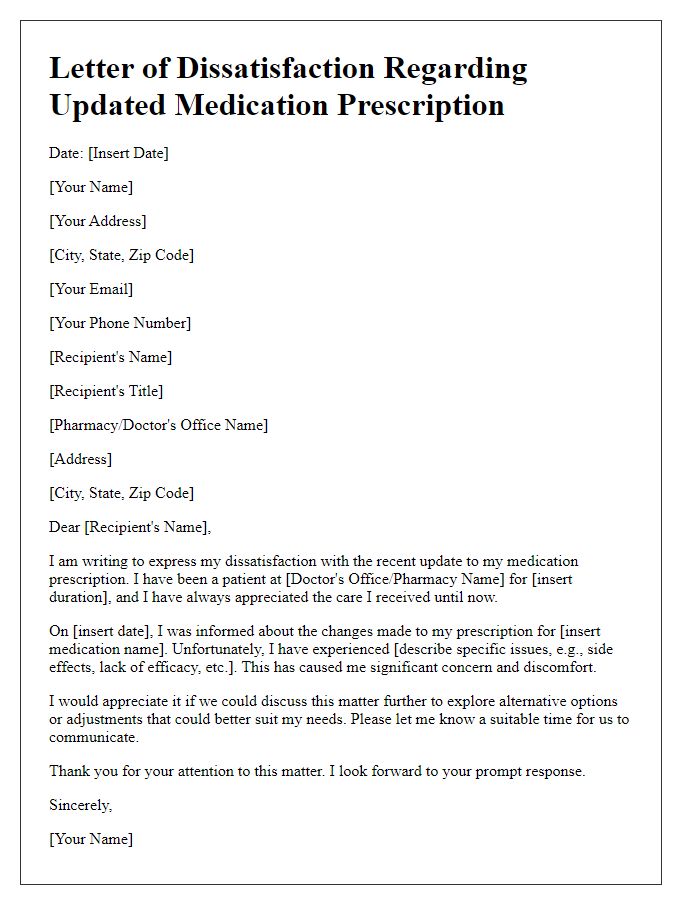
Letter template of dissatisfaction with updated medication prescription.



Comments