Are you preparing for an epilepsy monitoring appointment and feeling a bit overwhelmed? You're not aloneâmany face uncertainty about what to expect during this crucial process. In this article, we'll break down the key aspects of a monitoring appointment, helping you feel informed and ready. So, grab a cup of your favorite beverage and read on to discover everything you need to know!
Patient Identification
Epilepsy monitoring appointments are crucial for accurately diagnosing and managing seizure disorders in patients. During these evaluations, which commonly take place in specialized centers or hospitals, healthcare professionals closely observe patients for seizure activity, typically using electroencephalography (EEG) technology. This process involves electrodes applied to the scalp, monitoring brain wave patterns (usually over 24 to 72 hours). Patient identification is essential to ensure personalized care, which includes reviewing the patient's unique medical history, previous seizure episodes, and any relevant medication usage (such as antiepileptic drugs). Proper identification also helps facilitate communication among medical staff and enables tailored recommendations for treatment plans based on observed seizure types and frequencies.
Appointment Details
Epilepsy monitoring involves a series of specialized assessments to evaluate seizure activity in patients diagnosed with epilepsy, a neurological disorder affecting over 65 million people worldwide. During the appointment, which typically takes place at a dedicated epilepsy center like Cleveland Clinic or Mayo Clinic, healthcare professionals will conduct EEG (electroencephalogram) tests, capturing brain wave patterns. Duration of monitoring can vary, ranging from 24 hours to several days, depending on the patient's specific needs. Patients may be asked to maintain a seizure diary, documenting triggers and symptoms that can assist in the evaluation. Continuous supervision by seizure response teams ensures safety and immediate intervention, generally utilizing video telemetry to correlate physical symptoms with brain activity. Post-evaluation, neurologists will analyze data to customize treatment plans, which might include medications, lifestyle changes, or surgical options for seizure control.
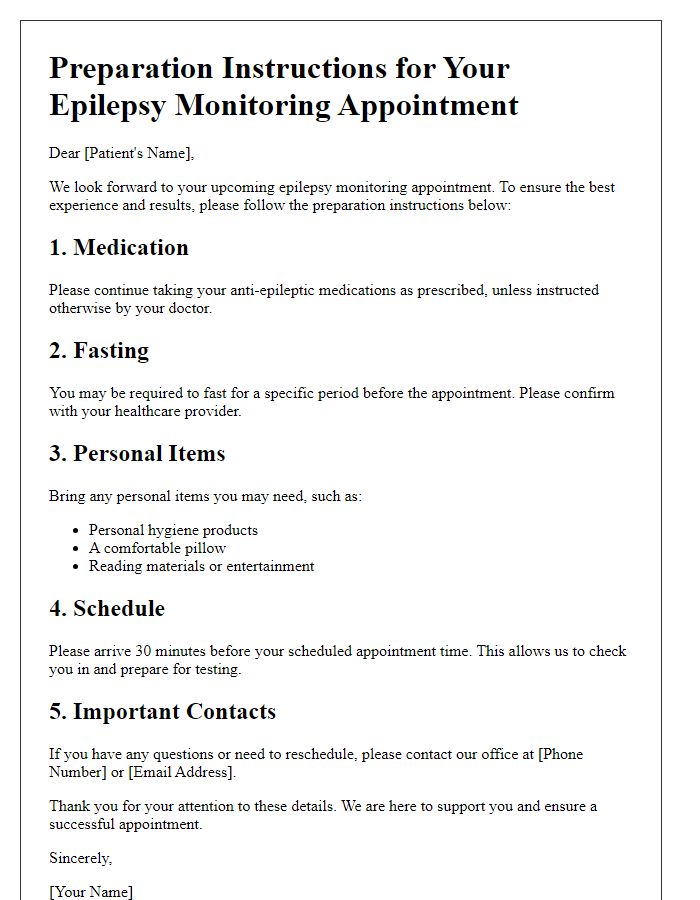
Preparation Instructions
Epilepsy monitoring appointments at specialized centers typically require thorough preparations to ensure accurate results. Patients should keep seizure diaries detailing frequency, duration, and triggers for at least two weeks before the appointment. Medications (anticonvulsants such as Lamotrigine or Keppra) should be discussed with healthcare providers regarding adjustments, as changes may enhance seizure occurrence during monitoring. Patients are advised to avoid caffeine and alcohol 48 hours prior to the appointment to minimize interference with the monitoring process. It is essential to arrange transportation, as some patients may experience increased seizure activity during the evaluation. Comfortable clothing suitable for a multi-day stay at epilepsy monitoring units (EMUs) should be packed, and personal items like toiletries should be prepared for convenience. Accompanying family members or caregivers should also be briefed on the patient's medical history and potential emergency protocols.
Contact Information
Epilepsy monitoring appointments are crucial for individuals diagnosed with epilepsy, often conducted at specialized facilities such as neurology clinics or hospitals. These appointments aim to observe brain activity using electroencephalograms (EEGs) to determine seizure types and frequency. Patients usually undergo a series of tests over several days, during which they may have the opportunity to trigger seizures naturally or through controlled stimuli. Staff, including neurologists and epilepsy nurse practitioners, provide guidance and support throughout the process to ensure accurate results. Proper preparation, including medication management and sleep deprivation if instructed, significantly impacts the effectiveness of these assessments in tailoring treatment plans.
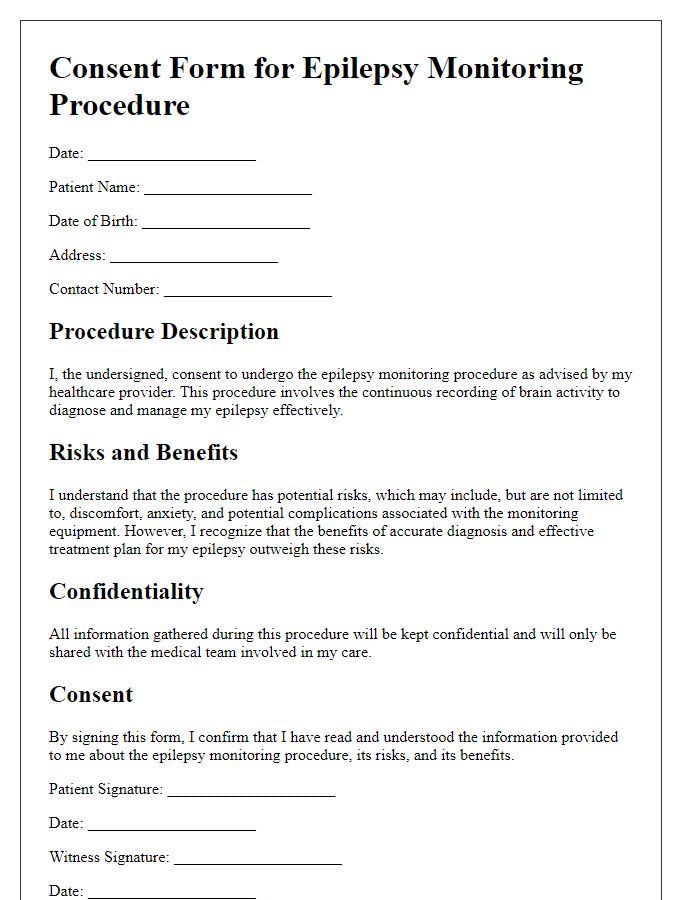
Privacy and Confidentiality
During an epilepsy monitoring appointment, maintaining privacy and confidentiality is crucial to protect sensitive medical information. Patients, often individuals diagnosed with epilepsy - a neurological disorder characterized by recurrent seizures - must feel secure regarding their personal data. Healthcare professionals are required to adhere to stringent guidelines, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, which mandates the safeguarding of patient information. Additionally, medical facilities, like specialized epilepsy centers, implement robust protocols that limit access to patient records, ensuring that only authorized personnel can view sensitive information. Furthermore, patients are encouraged to discuss any concerns regarding privacy with their healthcare providers to enhance their overall experience during monitoring procedures.
Letter Template For Epilepsy Monitoring Appointment Samples
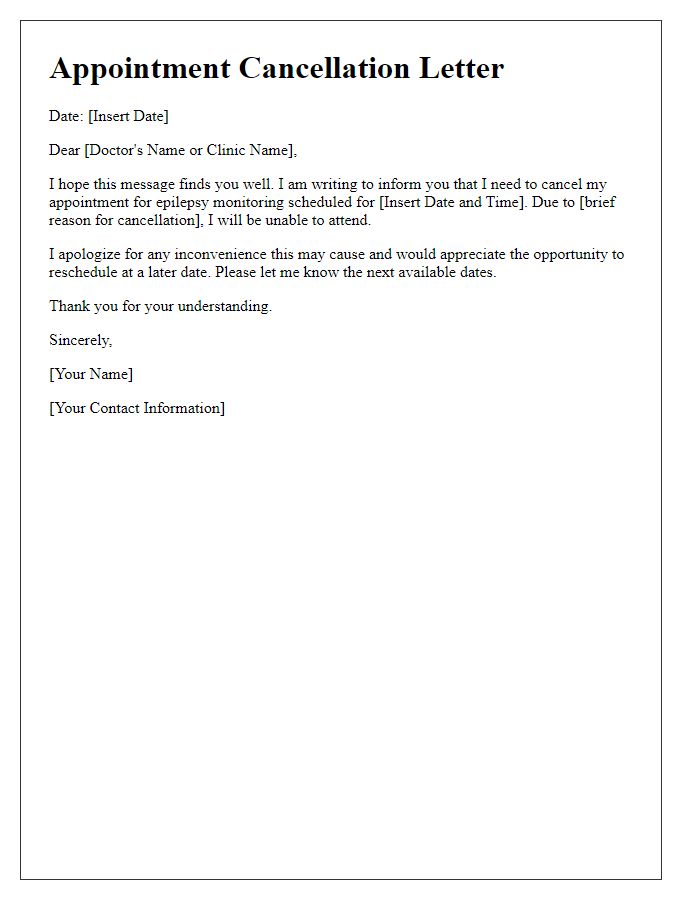
Letter template of request for epilepsy monitoring appointment confirmation
Letter template of preparation instructions for an epilepsy monitoring appointment
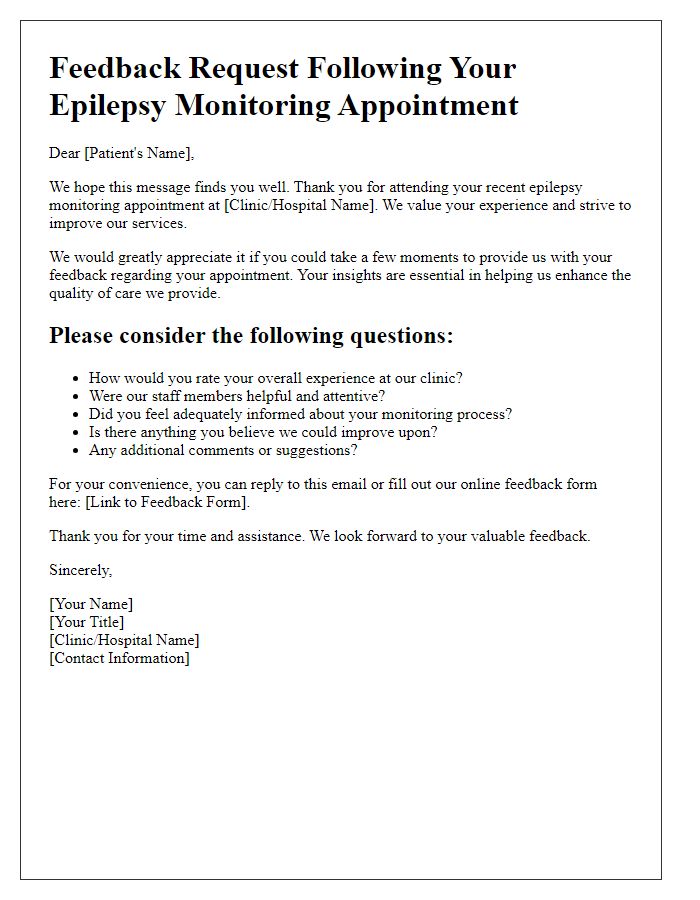
Letter template of inquiry about epilepsy monitoring appointment results


Comments