Are you navigating the complex world of medical billing and have questions lingering in your mind? You're not alone! Many patients find themselves puzzled by the details of their medical statements and insurance claims. In our article, we'll break down common inquiries and provide clear answers to help you understand your bills betterâso stick around and read more!
Patient information verification
Patient information verification is a critical step in the medical billing process, ensuring accuracy in billing and claims submission. During this process, details such as the patient's name, date of birth, insurance policy number, and contact information must be cross-referenced with the records provided by healthcare providers like hospitals and clinics. Accurate patient identification reduces the likelihood of billing errors and denied claims, ultimately streamlining revenue cycles within healthcare organizations. Healthcare facilities often implement verification processes at points of service, utilizing tools and software systems designed to capture real-time data updates, which are essential for maintaining patient records compliant with regulations established by agencies such as the Health Insurance Portability and Accountability Act (HIPAA).
Billing reference number
Medical billing inquiries often require detailed information to ensure proper communication and resolution. A billing reference number, such as 123456789, serves as a unique identifier for the specific case, facilitating tracking and follow-up. Patients experiencing discrepancies should provide pertinent details, including date of service (e.g., October 10, 2023), procedure codes (e.g., CPT 99213 for an office visit), and the name of the healthcare provider (e.g., Dr. John Smith at General Health Clinic). Clear communication is vital to address concerns related to charges, insurance coverage, or outstanding balances, ensuring patients understand their financial responsibilities and any potential errors in billing statements.
Date of service
Medical billing inquiries require precise details to ensure clarity and resolution. Each date of service, such as January 15, 2023, must be accurately referenced, connecting to specific medical procedures or consultations that were conducted. Diagnostic codes, like ICD-10 (International Classification of Diseases, Tenth Revision), should accompany any related services, such as X-rays or laboratory tests. Billing statements reflecting the total amount charged, insurance adjustments, and patient co-payments play a crucial role in understanding the final owed amount. Additionally, referencing the healthcare provider, such as St. Mary's Hospital, along with their National Provider Identifier (NPI) number strengthens the inquiry by confirming the legitimacy of the services rendered. Timely follow-ups on such inquiries are essential, often recommended within 30 days from the date the bill was issued, to avoid complications with payment processing.
Detailed charge explanation
Patients often seek clarity regarding detailed medical billing inquiries after receiving statements. Medical billing statements typically include charges from services rendered in healthcare settings, such as hospitals or clinics. For instance, a visit to a hospital emergency department may detail fees for an evaluation and management service, which could cost around $250, alongside additional charges for diagnostic tests like X-rays that may reach $100. Further, any administered medications, such as analgesics or antibiotics, can incur an extra $30. It is essential to break down these charges, including potential insurance adjustments, copayments, and coinsurance amounts, to ensure the patient understands the final balance due. Accurate billing codes utilized in the process, such as those from the Current Procedural Terminology (CPT), are crucial for audit compliance and reimbursement accuracy. Overall, a transparent explanation enables patients to navigate through their healthcare expenses confidently.
Contact details for further assistance
In medical billing inquiries, prompt and clear communication is essential. For direct assistance, individuals can reach out to the billing department of their healthcare provider or insurance company. Typically, these contact numbers are listed on billing statements, patient portals, or official websites. Common hours of operation (often from 8 AM to 5 PM local time) provide ample opportunity for inquiries. Additionally, some organizations may offer dedicated email addresses specifically for billing concerns, allowing for documentation of communications. For faster resolutions, it's advisable to have the patient account number, invoice number, and any relevant medical information readily available when contacting support representatives.
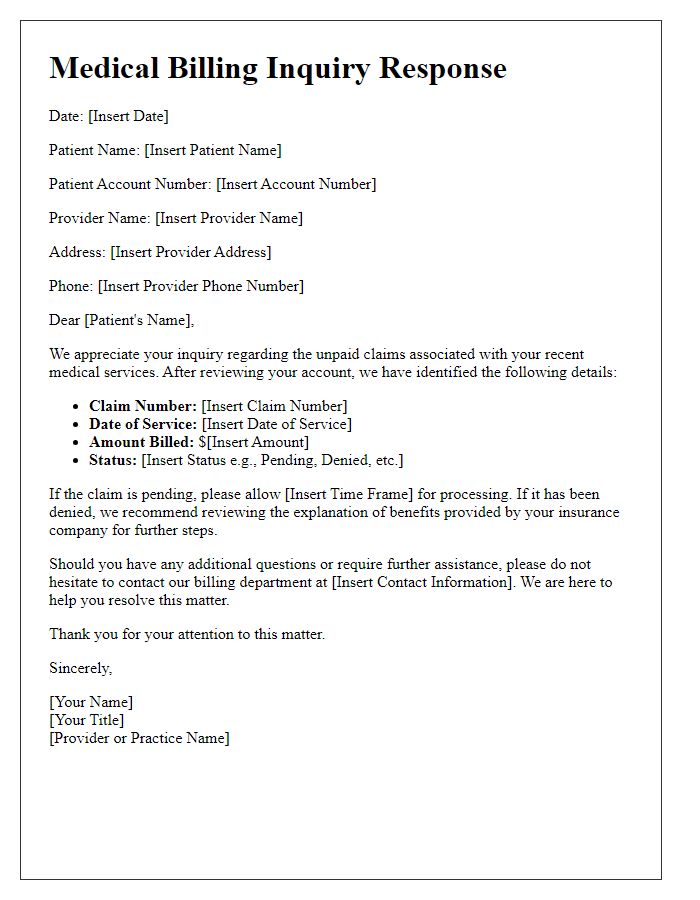
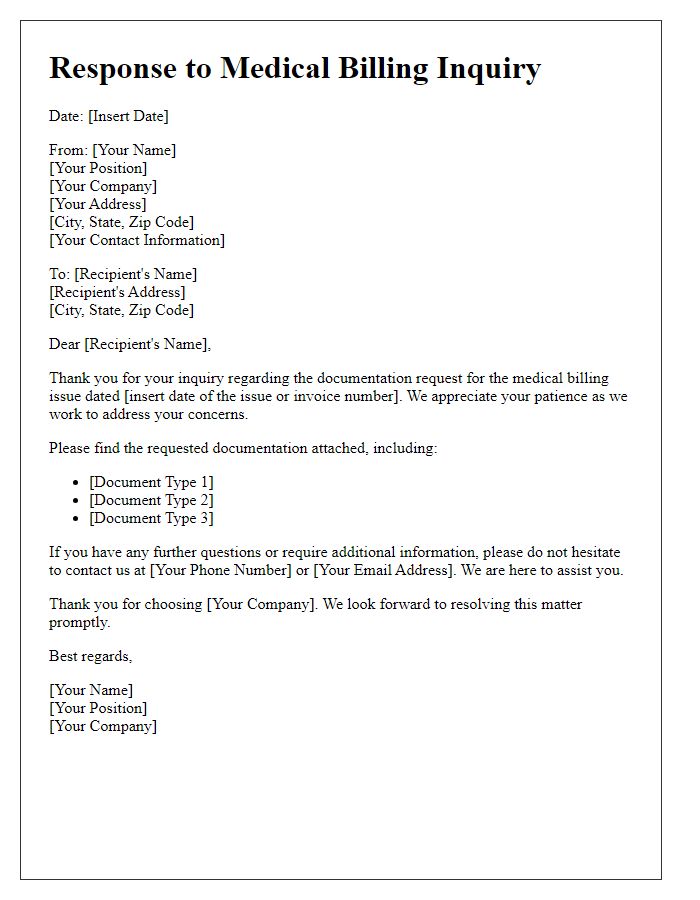
Letter Template For Medical Billing Inquiry Response Samples
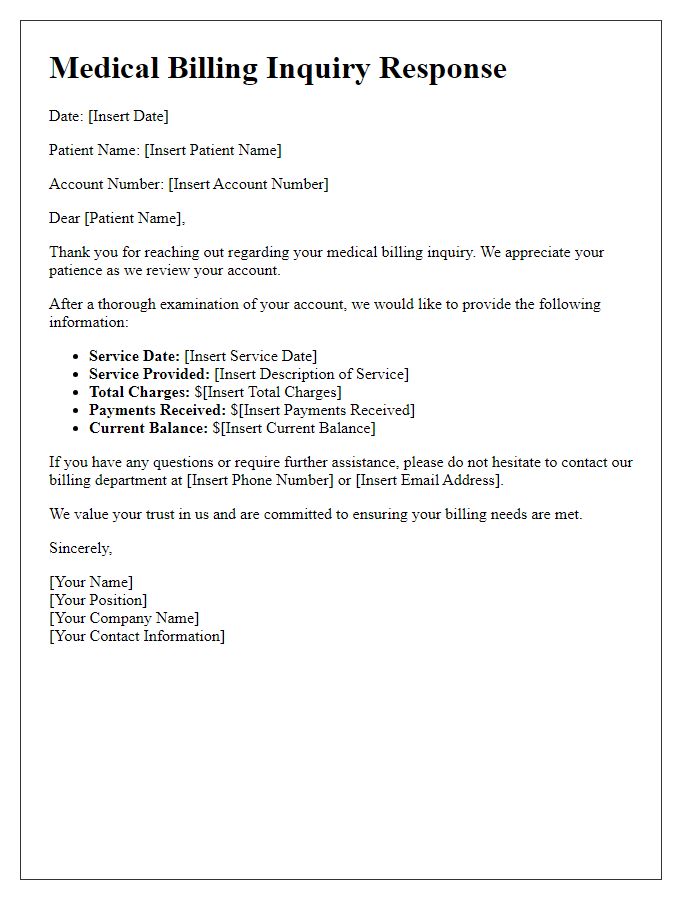
Letter template of medical billing inquiry response for patient account review.
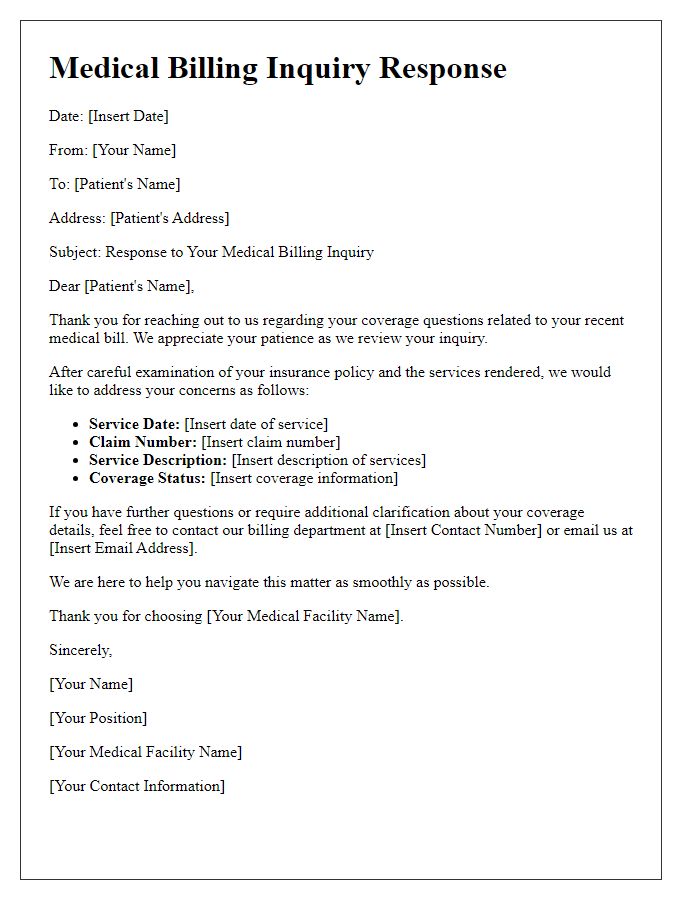
Letter template of medical billing inquiry response for coverage questions.
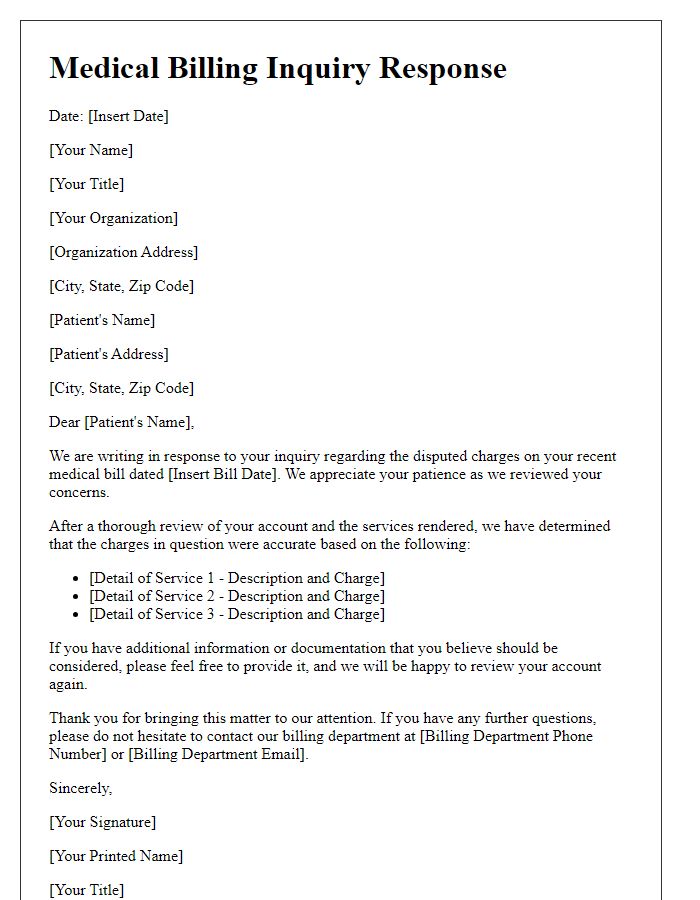
Letter template of medical billing inquiry response for disputed charges.
Letter template of medical billing inquiry response for explanation of benefits.

Letter template of medical billing inquiry response for claim status update.
Letter template of medical billing inquiry response for billing error correction.
Letter template of medical billing inquiry response for appeal process guidance.
Letter template of medical billing inquiry response for payment plan request.


Comments