When it comes to discussing advanced care directives, many people feel a sense of uncertainty or even anxiety. However, having these conversations is essential for ensuring that our loved ones understand our wishes regarding medical treatment when we may no longer be able to express them ourselves. An advanced care directive can provide peace of mind for both you and your family, ensuring that everyone is on the same page during challenging times. So, let's dive deeper into this important topic and explore how to navigate these discussions effectively.

Salutation and Introduction
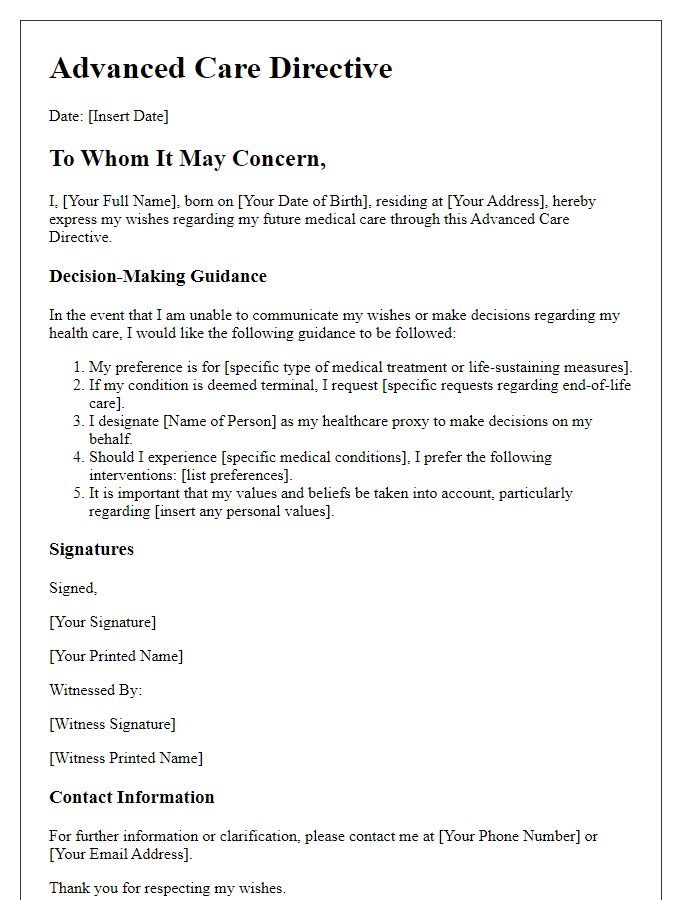
An advanced care directive serves as a crucial document outlining an individual's preferences for medical treatment in case of incapacitation, ensuring that healthcare decisions align with personal values and desires. Essential components include specific treatment options, preferences for end-of-life care, and a legally designated decision-maker. In various jurisdictions, such as the United States, the directives must comply with state laws to be valid, emphasizing the importance of understanding local regulations. Discussions around advanced care directives are notably sensitive, often involving family members, healthcare professionals, and legal advisors to ensure that the individual's wishes are respected and documented accurately.
Purpose and Importance of Discussion
An advanced care directive discussion is a crucial conversation that enables individuals to articulate their healthcare preferences and values in the event they are unable to communicate them themselves. The purpose of this discussion is to ensure that medical practitioners and family members are fully aware of a person's wishes regarding treatment options, life-sustaining measures, and palliative care. Importance lies in promoting autonomy, reducing uncertainty during critical moments, and alleviating the emotional burden on loved ones by providing clear guidance. By utilizing a letter template for this discussion, it becomes easier to structure thoughts, highlight key concerns, and foster open communication about deeply personal health-related decisions. This proactive approach significantly enhances the likelihood of aligning healthcare outcomes with individual desires.
Relevant Medical and Personal Information
A letter template serves as a vital tool in organizing relevant medical and personal information for advanced care directive discussions. This framework facilitates clear communication regarding an individual's healthcare preferences and choices. Essential details include medical history, such as chronic conditions and allergies, which provide healthcare providers crucial insights into a patient's needs. Personal information encompasses values, beliefs, and end-of-life preferences, ensuring that loved ones and medical professionals understand the individual's wishes. This comprehensive approach fosters informed decision-making, enhancing the alignment of medical care with the person's goals and desires.
Key Questions and Decisions
Advanced care directives encompass vital decisions regarding healthcare preferences during incapacitation. Key questions address personal values and beliefs, guiding choices about end-of-life care. Patients often consider scenarios like terminal illness, irreversible conditions, or persistent vegetative states, requiring clarity on interventions such as resuscitation, life support, or hospice care. Discussions should include appointing healthcare proxies, individuals authorized to make decisions when patients are unable. Legal considerations vary by jurisdiction, emphasizing the importance of understanding local regulations regarding medical decisions, documentation, and treatment protocols. The sanctity of personal autonomy and quality of life remains central to these discussions, shaping tailored directives reflecting individual desires and healthcare goals.
Closing and Next Steps
Concluding a discussion on advanced care directives often involves summarizing key points, addressing questions, and outlining future steps for implementation. Encourage individuals to reflect on their preferences regarding medical treatment and end-of-life care. Provide resources such as state-specific forms or guidelines, accessible through local health departments or websites like the National Hospice and Palliative Care Organization. Emphasize the importance of consulting healthcare professionals for understanding the implications and legal aspects of their directives. Schedule follow-up meetings to review completed directives or discuss any changes, ensuring a clear pathway for individuals to communicate their healthcare wishes with family members and medical providers.
Letter Template For Advanced Care Directive Discussion Samples
Letter template of advanced care directive overview for healthcare providers


Comments