In today's fast-paced healthcare environment, effective coordination among multi-disciplinary care teams is essential for delivering high-quality patient care. As healthcare providers across various specialties come together, clear communication and strategic collaboration become key components in ensuring that every patient receives comprehensive and personalized treatment. By breaking down silos and fostering teamwork, we can harmonize our efforts, streamline processes, and ultimately elevate patient outcomes. Join us as we explore the best practices for optimizing multi-disciplinary care team coordination in our latest article!
Clear communication objectives
Effective multi-disciplinary care team coordination relies on clear communication objectives that enhance collaboration among diverse professionals. Establishing specific goals, such as improving patient outcomes by 20%, facilitates focused teamwork within healthcare settings like hospitals, rehabilitation centers, and outpatient clinics. In weekly meetings, team members, including physicians, nurses, therapists, and social workers, should share updates on patient progress, utilizing electronic health records (EHR) for seamless information exchange. Strategies such as standardized handoff protocols and joint care plans can ensure that all professionals adhere to shared objectives. Regular feedback sessions can identify barriers, allowing teams to adjust tactics in real-time, thus maintaining an adaptive approach to patient care. Clear documentation of roles and responsibilities further supports accountability, fostering an environment of trust and efficiency.
Comprehensive team member contact details
Effective coordination among multi-disciplinary care teams hinges on comprehensive contact information for each team member. This includes essential details such as full names, professional titles (e.g., Physician, Nurse Practitioner, Social Worker), direct phone lines, email addresses, and specialized roles within the team. Ensuring that each member's area of expertise (e.g., cardiology, oncology, mental health) is clearly indicated contributes to streamlined communication. Additional information may encompass office locations, shift schedules, and preferred contact methods, fostering enhanced collaboration during patient management discussions, care plan adjustments, and urgent consultation requests. This systematic approach aids in optimizing patient care outcomes and reinforces a unified collaborative environment.
Role and responsibility clarification
Multi-disciplinary care teams play a crucial role in delivering comprehensive patient care, emphasizing the need for clear role and responsibility delineation among team members. Each discipline, whether it be nursing, social work, pharmacy, or physical therapy, contributes unique expertise essential for holistic treatment approaches. For instance, registered nurses manage day-to-day patient care and monitor vital signs. Social workers address emotional and social health issues (including resource access) while facilitating family dynamics. Pharmacists ensure medication management, focusing on potential drug interactions and side effects. Physical therapists design appropriate rehabilitation exercises tailored to individual patient needs. Clear communication strategies, utilizing tools like project management software or regular interdisciplinary meetings, enhance care delivery by fostering collaboration, minimizing misunderstandings, and improving patient outcomes. Engaging all team members actively fosters a cooperative environment essential for achieving shared goals in patient health improvement.
Patient-centered care plan outline
Patient-centered care plans are essential for ensuring cohesive communication among multi-disciplinary care teams. Each plan should include patient history details, including pertinent medical diagnoses such as Type 2 Diabetes or Hypertension. Specific goals should be outlined, targeting measurable outcomes like glucose level reduction (aiming for below 7% A1C within three months). The roles of team members should be specified, naming professionals such as primary care physicians, dietitians, and physical therapists. Regular follow-up schedules must be established, emphasizing bi-weekly check-ins at the healthcare facility, located at 123 Healthcare Lane, Springfield. Progress monitoring protocols should incorporate patient feedback and clinical metrics to adapt the care plan as needed effectively. Documentation of all communications and interventions is crucial for maintaining continuity in care delivery and enhancing patient engagement.
Scheduling and follow-up procedures
Multi-disciplinary care team coordination requires effective scheduling and follow-up procedures to ensure comprehensive patient management. The team typically comprises healthcare professionals such as physicians, nurses, social workers, and rehabilitation specialists, working together to address complex health issues. It is crucial to establish a centralized scheduling system for appointments, possibly utilizing software like Epic or Cerner to streamline communication across disciplines. Regular interdisciplinary meetings, scheduled bi-weekly or monthly, can facilitate updates on patient progress and treatment plans. Follow-up procedures should include shared electronic health records (EHR) that maintain continuity of care, detailing notes on patient interactions, interventions, and outcomes. Additionally, timely communication regarding any changes in patient status or urgent needs is critical for maintaining coordinated care.
Letter Template For Multi-Disciplinary Care Team Coordination Samples
Letter template of collaboration for multi-disciplinary care team meetings
Letter template of communication for multi-disciplinary healthcare collaboration
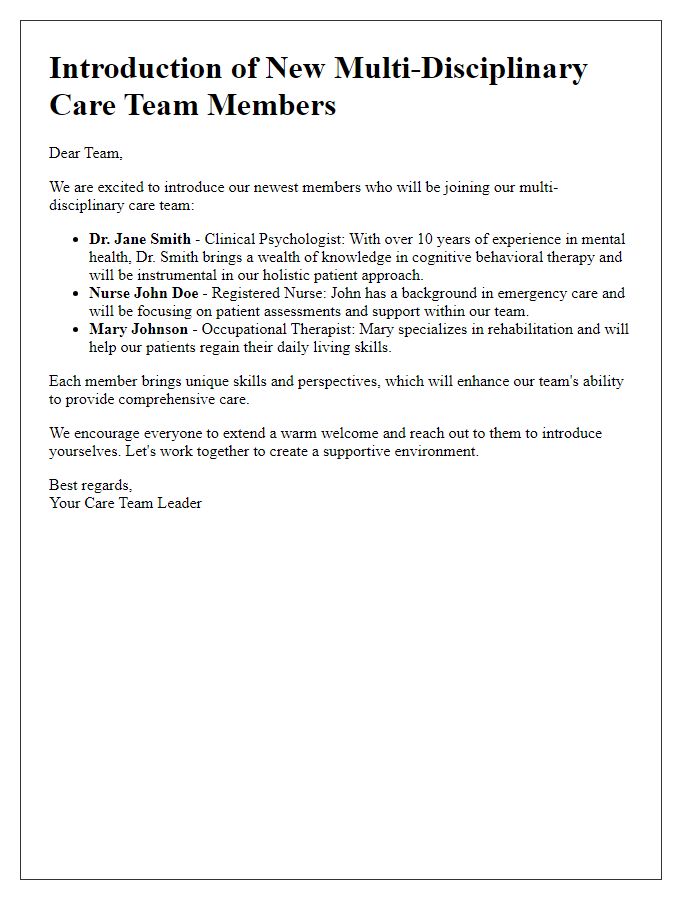
Letter template of introduction for new multi-disciplinary care team members


Comments