When it comes to end-of-life care planning, having a clear and compassionate approach is more important than ever. It's a journey that involves not only understanding your own wishes but also ensuring that they are communicated effectively with your loved ones and healthcare providers. This process can seem daunting, but with the right information and support, it can lead to peace of mind and a sense of control during a challenging time. Join me as we explore essential advice and insights to help you navigate this deeply personal aspect of life and ensure your preferences are honored.
Patient Information and Details
End-of-life care planning offers critical support to patients and families navigating complex medical decisions. Key elements include advance directives, healthcare proxy appointments, and preferences regarding pain management and palliative care. Patients often consider personal values, cultural beliefs, and previous experiences with illness when articulating end-of-life wishes, potentially involving family discussions for clarity. Documentation, regulated by state laws, ensures that an individual's choices are honored; documents may include a living will or Do Not Resuscitate (DNR) order. Regular reviews of the plan, especially during significant health changes, enhance ongoing communication between patients, loved ones, and healthcare providers to align treatment goals with personal preferences, ultimately ensuring dignity and comfort in the patient's final days.
Goals and Values in Care
End-of-life care planning encompasses critical decisions regarding the preferences and values of an individual nearing the end of life. This process often involves discussions about goals that prioritize comfort, dignity, and respect for personal wishes. Establishing clear communication about healthcare preferences in advanced directives, such as living wills or healthcare proxies, ensures that individuals' choices regarding life-sustaining treatments and palliative care align with their personal beliefs and values. In addition, support from healthcare professionals plays a vital role in navigating emotional and practical aspects of end-of-life decisions. Planning discussions may take place in various settings, including homes, hospices, or hospitals, and should consider the involvement of family members and loved ones for a holistic approach to care. Such proactive measures can significantly enhance the quality of life in the final stages for patients in places like nursing homes or residential care facilities, while also reducing anxiety for both the affected individuals and their families.
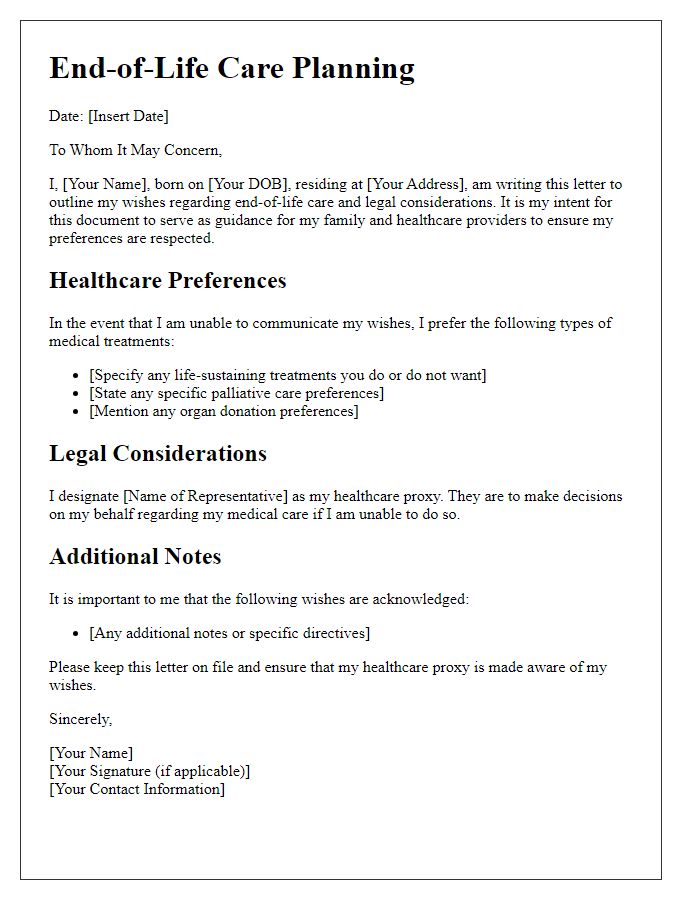
Medical Treatment Preferences
End-of-life care planning is essential for ensuring that an individual's medical treatment preferences are respected. Patients should communicate their wishes regarding interventions, such as resuscitation, intubation, and artificial nutrition. Documenting a Living Will (a legal document specifying medical preferences) is crucial for clarity in critical situations. Engaging in conversations with healthcare providers about palliative care options can enhance comfort during the end of life, focusing on quality over quantity. Identifying a Healthcare Proxy (a designated individual responsible for making decisions) can also provide peace of mind. Such planning ensures that individuals' desires are honored, honoring autonomy in healthcare decisions.
Legal and Financial Arrangements
End-of-life care planning encompasses critical legal and financial arrangements that ensure an individual's wishes are respected during their final stages of life. Important documents such as advance healthcare directives or living wills outline preferences for medical treatment and designate a healthcare proxy, typically a family member or trusted friend, to make decisions on one's behalf, as seen in many U.S. states. Durable powers of attorney allow for the delegation of financial decisions, ensuring that legal affairs are managed effectively, especially in states like California, where specific regulations apply. Additionally, discussions regarding funeral arrangements and pre-paid funeral plans can alleviate burdens on loved ones, providing peace of mind and financial clarity. Healthcare costs can escalate dramatically during end-of-life care, making conversations about insurance coverage and assets essential to avoid financial strain. Regular reviews of these arrangements, ideally every few years or after significant life events, help to ensure alignment with an individual's evolving preferences and circumstances.
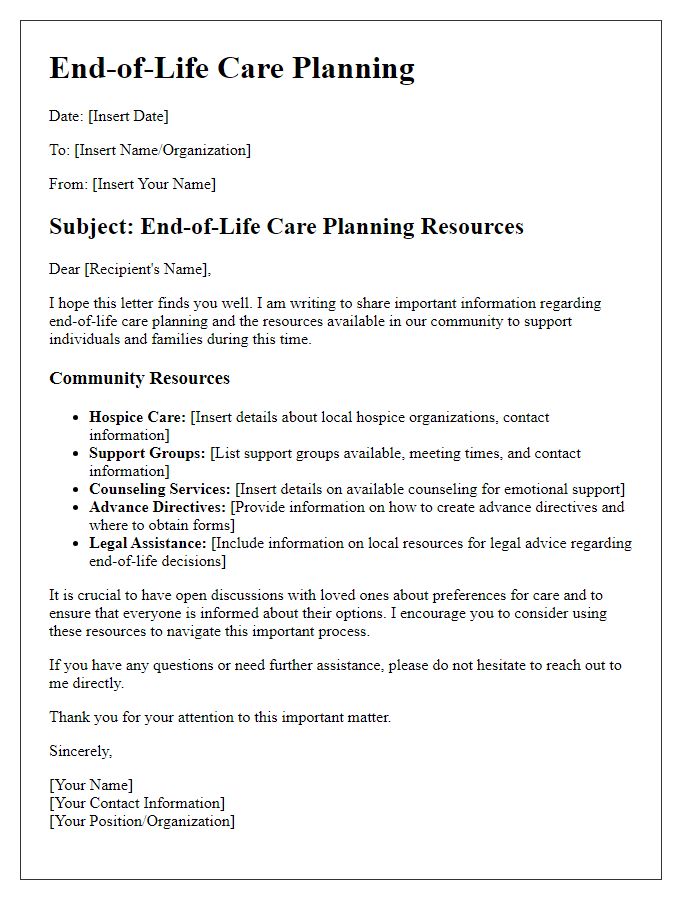
Communication with Family and Caregivers
End-of-life care planning is crucial for ensuring that individuals receive the appropriate support and comfort during their final days, particularly in sensitive environments such as hospitals or hospice care facilities. Communicating effectively with family members, friends, and caregivers about preferences and wishes regarding medical treatment and emotional support can help alleviate concerns and foster a collaborative atmosphere. Important elements include discussing advance directives, which outline patient preferences concerning life-sustaining treatments, and ensuring clarity on do-not-resuscitate (DNR) orders to reflect the patient's desires. Establishing a care team composed of healthcare professionals, social workers, and spiritual advisors can provide holistic support, addressing physical, emotional, and spiritual needs. Open and honest dialogue within this team can facilitate understanding and empathy, making the end-of-life experience more dignified and aligned with the patient's values.
Letter Template For End-Of-Life Care Planning Advice Samples
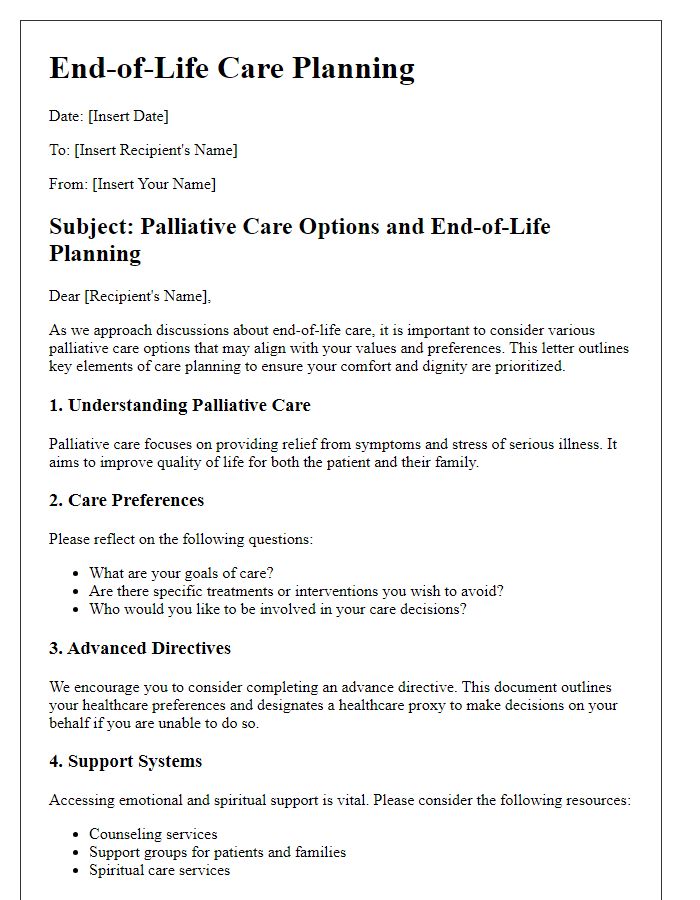
Letter template of end-of-life care planning for palliative care options
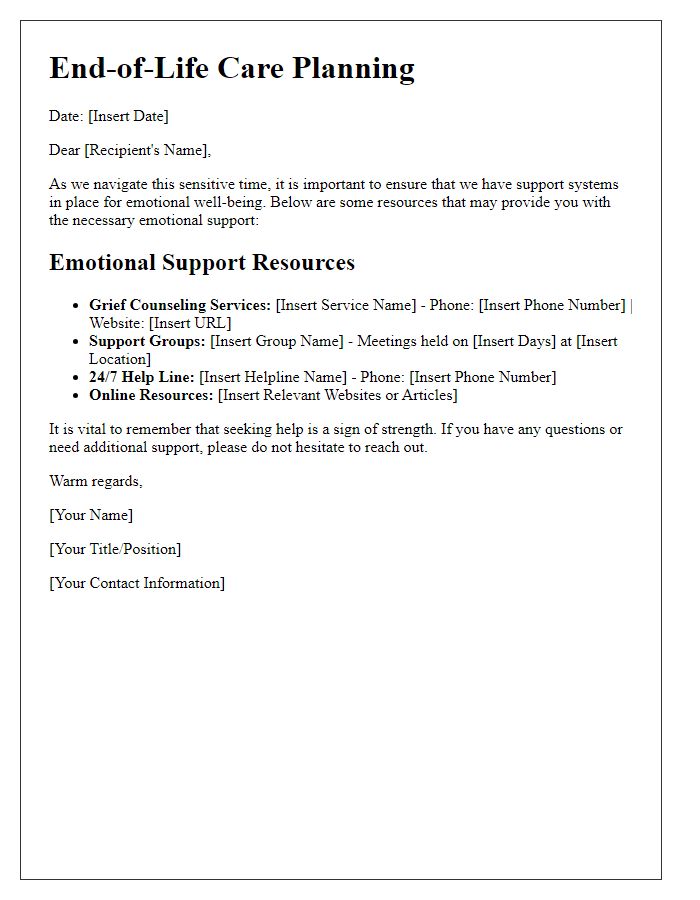
Letter template of end-of-life care planning for emotional support resources
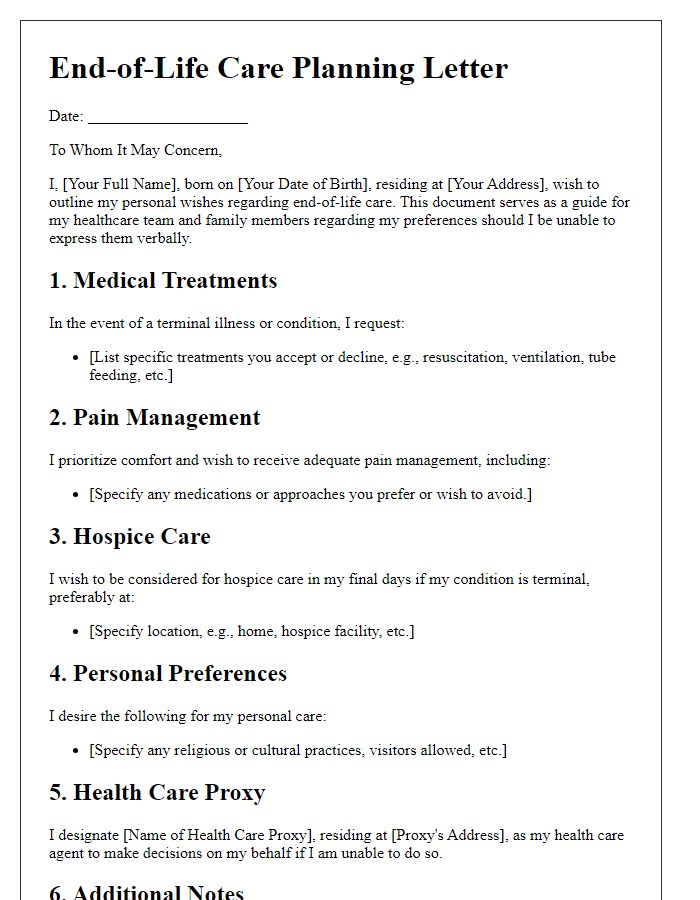
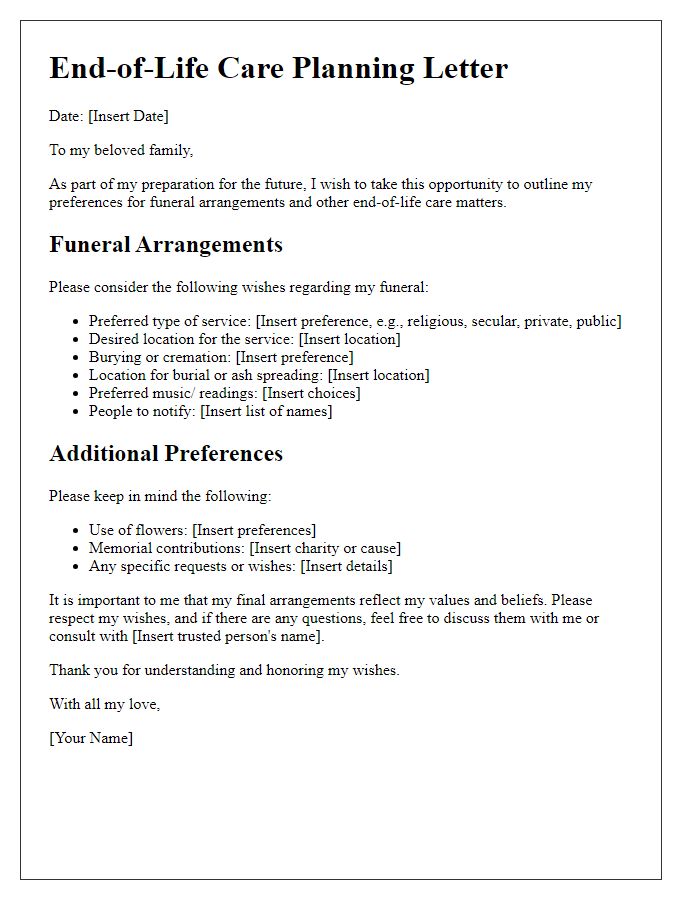
Letter template of end-of-life care planning for personal wishes documentation


Comments