When it comes to managing a chronic condition, staying informed and proactive is crucial for your health and well-being. Writing a care plan update letter not only keeps your healthcare team in the loop but also empowers you with a clear understanding of your ongoing treatment. This template can help you articulate your current status, any changes in your symptoms, and your goals moving forward. Ready to take control of your health journey? Let's dive deeper into how to craft the perfect update!
Patient Information
Patient information is critical in chronic condition care plans, serving to personalize treatment and monitor progress. Patients typically include first name, last name, and date of birth, which help identify individuals clearly within medical databases. The address details (including city, state, and zip code) ensure correct correspondence and facilitate home visits if necessary. Contact numbers, including a primary phone and emergency contact, contribute to timely communication regarding updates or changes in care plans. Medical history encompasses chronic conditions such as diabetes, hypertension, or heart disease, ensuring healthcare providers can develop tailored interventions. Current medications, dosage information, and treatment schedules are essential for avoiding drug interactions and monitoring adherence. Lastly, the inclusion of healthcare provider contacts fosters coordinated care among different specialists or clinics involved in the patient's health journey.
Summary of Condition
Patients with chronic conditions require ongoing management and assessments to ensure optimal health outcomes. Conditions such as diabetes, hypertension, or asthma necessitate continuous monitoring and intervention strategies tailored to individual needs. Comprehensive care plans must include details such as medication adherence rates, lifestyle changes, and symptom tracking developed through regular consultations with healthcare professionals. Updates on laboratory results, like HbA1c levels for diabetes management or blood pressure readings for hypertensive patients, are essential for adjusting treatment protocols. Regular follow-ups at designated healthcare facilities ensure that complications are identified early, contributing to enhanced patient quality of life. Collaborative efforts among care teams, patients, and support systems are crucial in creating effective chronic condition care plans.
Current Medications and Treatments
For individuals managing chronic conditions, a comprehensive understanding of current medications and treatments is essential for effective care. Commonly prescribed medications, such as Metformin for type 2 diabetes, may require dosage adjustments based on blood glucose readings, typically monitored through fingerstick tests that reveal daily fluctuations. Additional treatments could include lifestyle modifications like a low-sodium diet to manage hypertension, often emphasizing the importance of reducing sodium intake to below 2,300 mg per day. Regular consultations with healthcare providers, including endocrinologists or cardiologists, ensure that the treatment plan remains aligned with the evolving health status of the patient. Monitoring side effects and drug interactions is crucial, as over 50% of patients aged 65 and older take multiple medications concurrently. Integrating support from healthcare teams and family members plays a pivotal role in enhancing adherence to prescribed regimens, ultimately improving overall well-being.
Recent Tests and Results
Recent medical tests reveal significant insights into managing chronic conditions, such as diabetes and hypertension. Blood glucose levels averaged 150 mg/dL over the past month, indicating potential adjustments to dietary intake and medication may be necessary. Blood pressure readings frequently recorded at 145/90 mmHg suggest a closer review of antihypertensive medications and lifestyle modifications like increased physical activity. Cholesterol levels also showed a total of 240 mg/dL, classifying as borderline high, prompting possible dietary changes and the introduction of statins if necessary. The comprehensive analysis of lab results underscores the importance of regular monitoring and a tailored care plan to enhance overall health outcomes.
Updated Care Plan and Recommendations
Chronic conditions like diabetes require continuous monitoring and adjustment of care plans to ensure optimal health outcomes. The updated care plan includes specific blood sugar target levels, typically a fasting level of 70-130 mg/dL, to manage glucose effectively. Regular check-ups every three months are recommended to assess HbA1c levels, aiming for below 7% to minimize complications. Nutritional guidelines emphasize a balanced diet rich in whole grains, lean proteins, and fiber while limiting processed sugars. Exercise routines should incorporate at least 150 minutes of moderate aerobic activity weekly, such as brisk walking. Medication adjustments may be necessary, particularly for oral hypoglycemics or insulin therapy, depending on individual responses tracked through daily log assessments. Engagement with a certified diabetes educator and support groups can enhance adherence to these recommendations, fostering a supportive community for individuals managing their chronic condition.
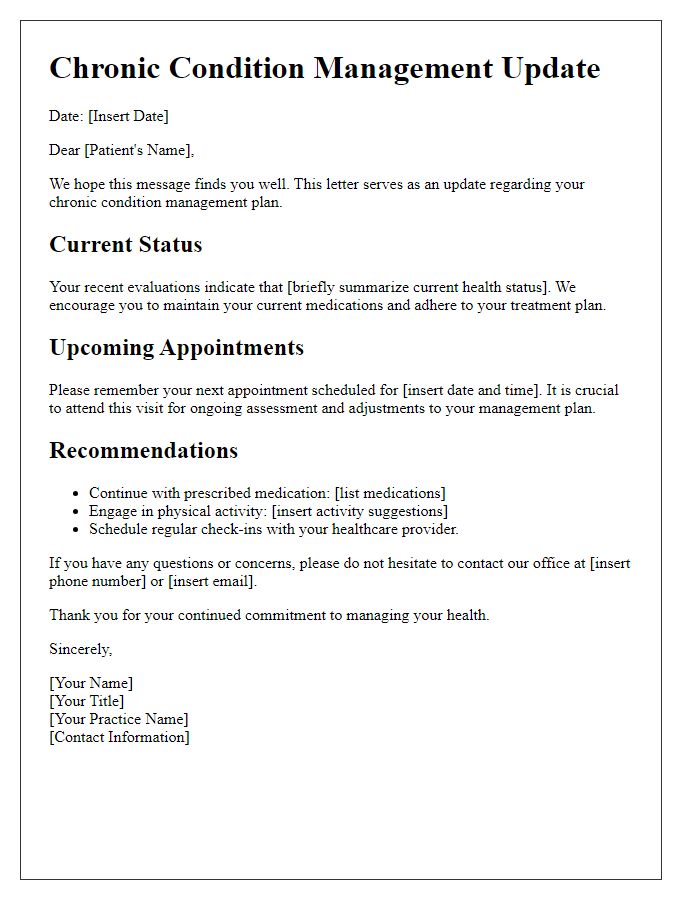
Letter Template For Chronic Condition Care Plan Update Samples
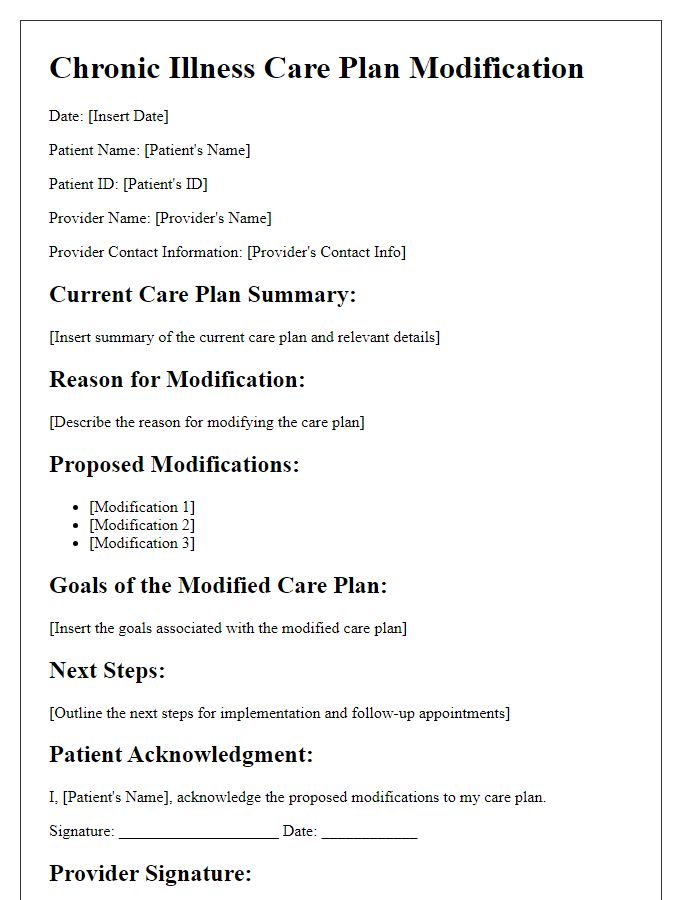
Letter template of patient-specific chronic illness care plan modification.
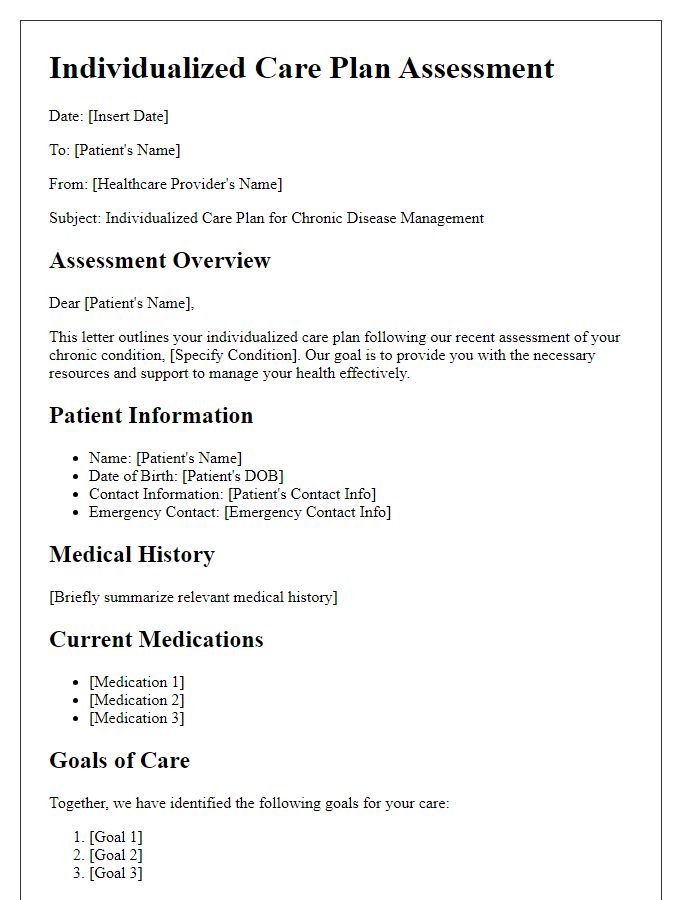
Letter template of individualized care plan assessment for chronic disease.


Comments