Hello there! When it comes to ensuring seamless patient care, a well-crafted referral notification letter is essential for any healthcare provider. Not only does it facilitate communication between specialists, but it also helps to keep patients informed and engaged in their treatment journey. Ready to learn how to create an effective specialist referral notification letter? Let's dive in!
Patient Information
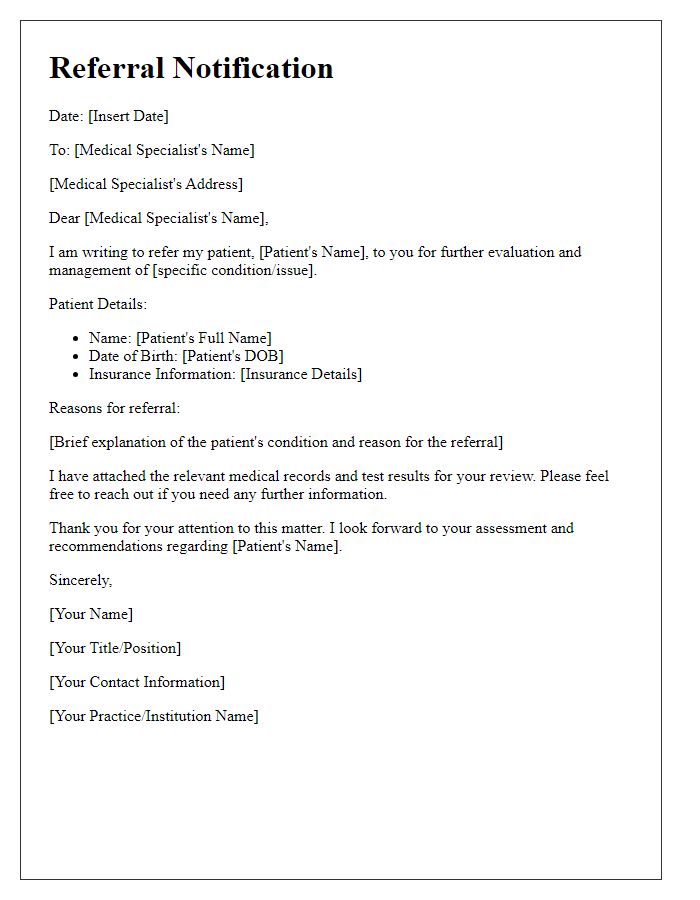
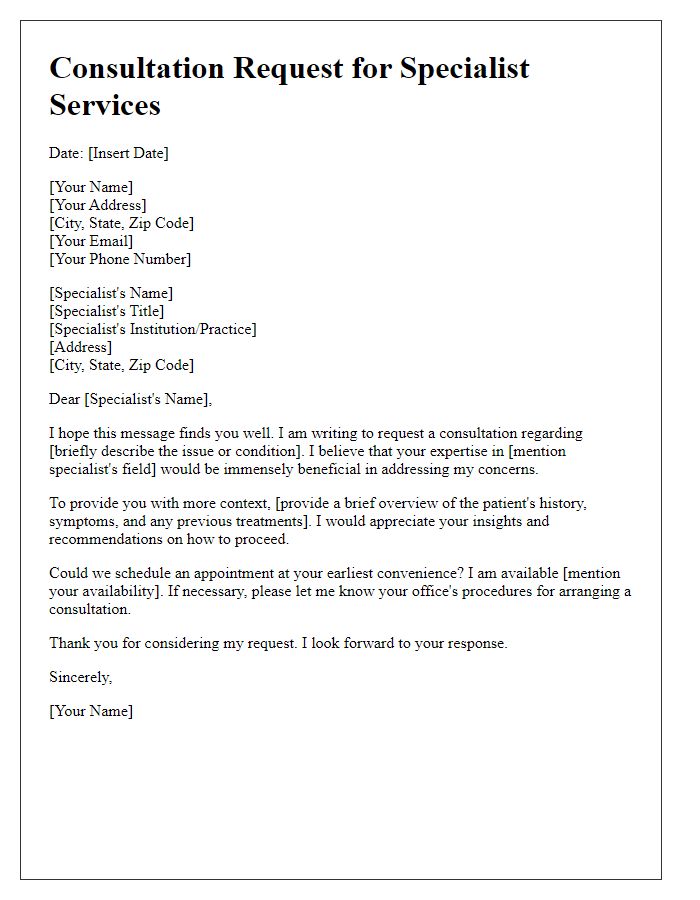
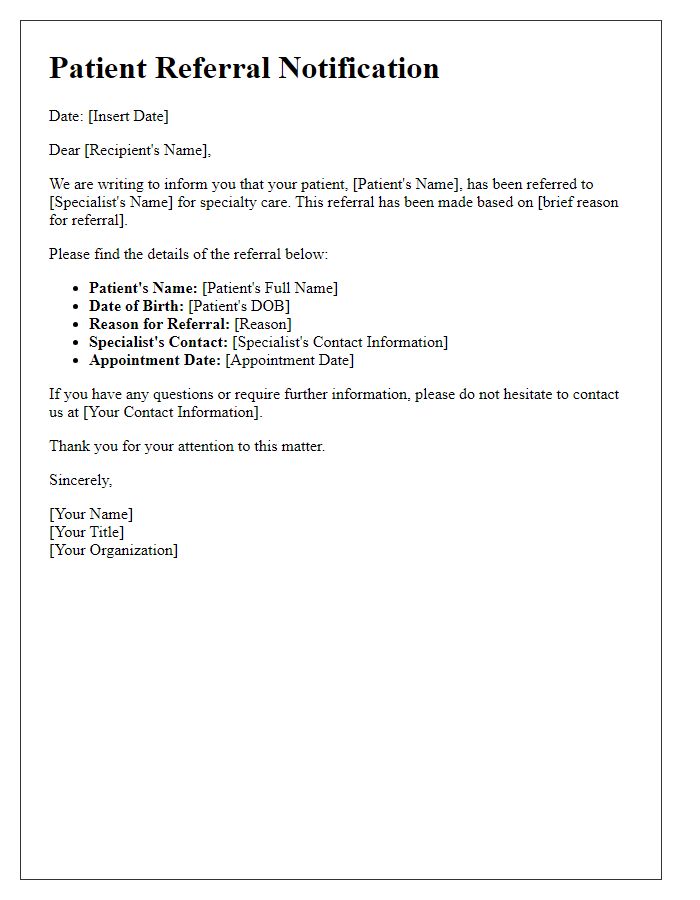
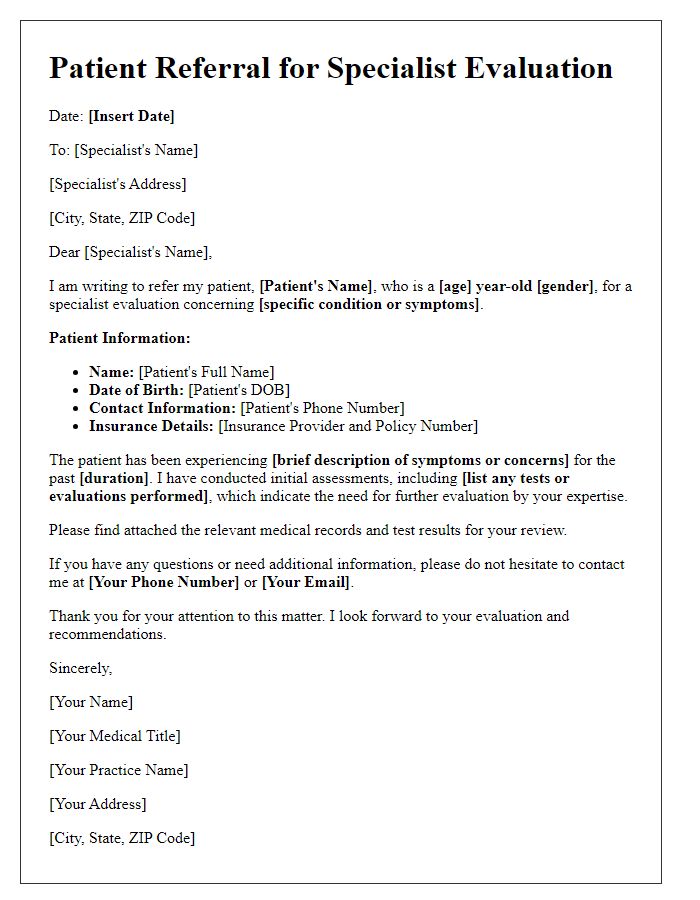
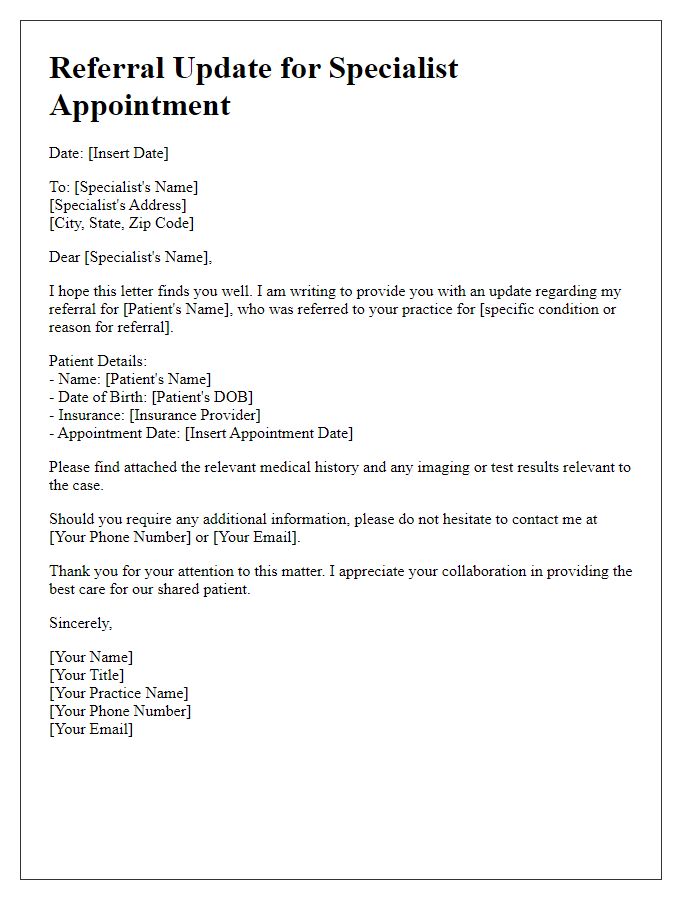
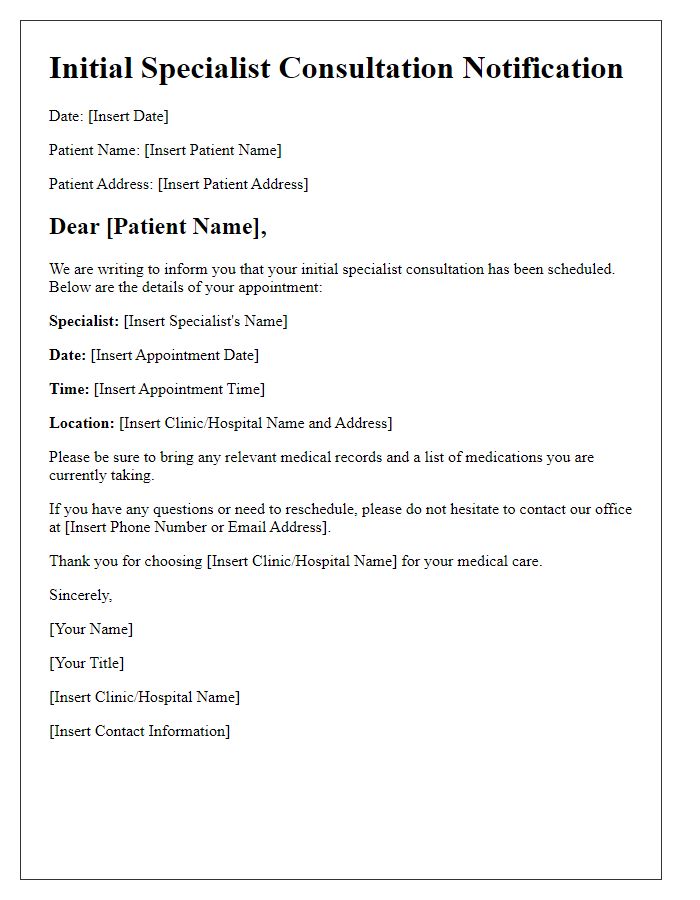
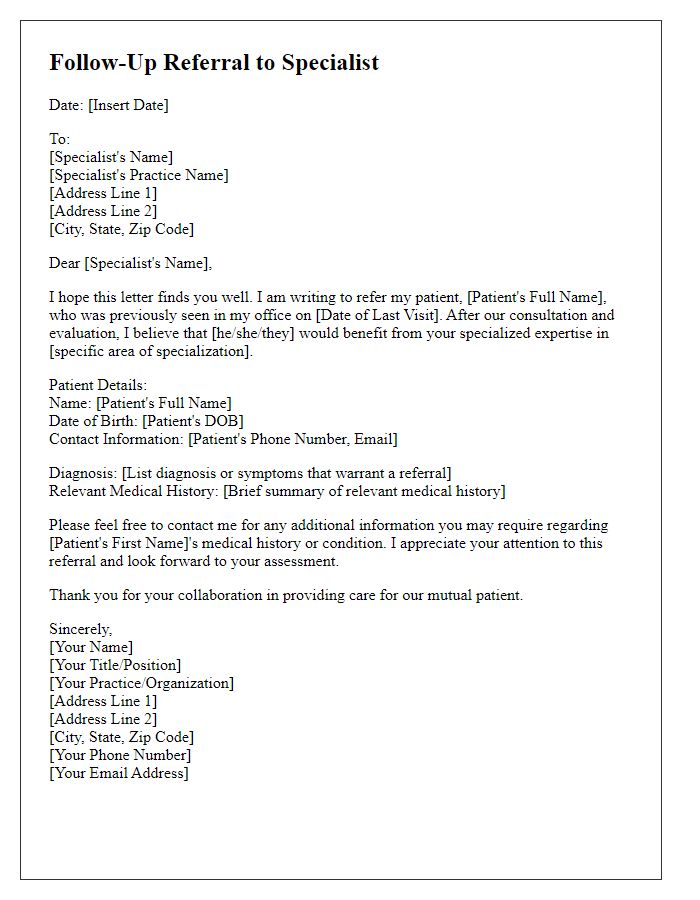
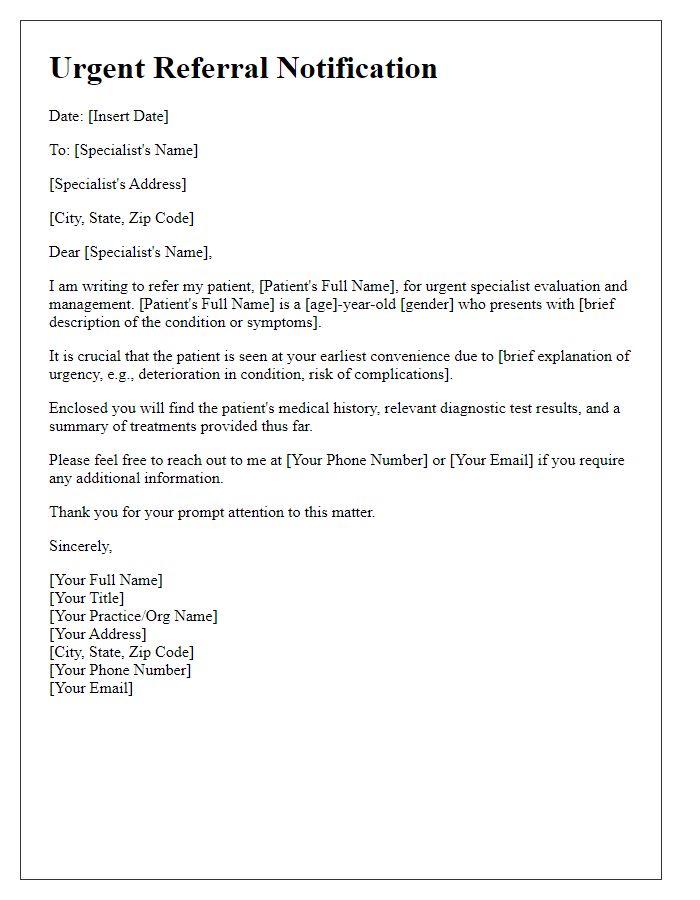
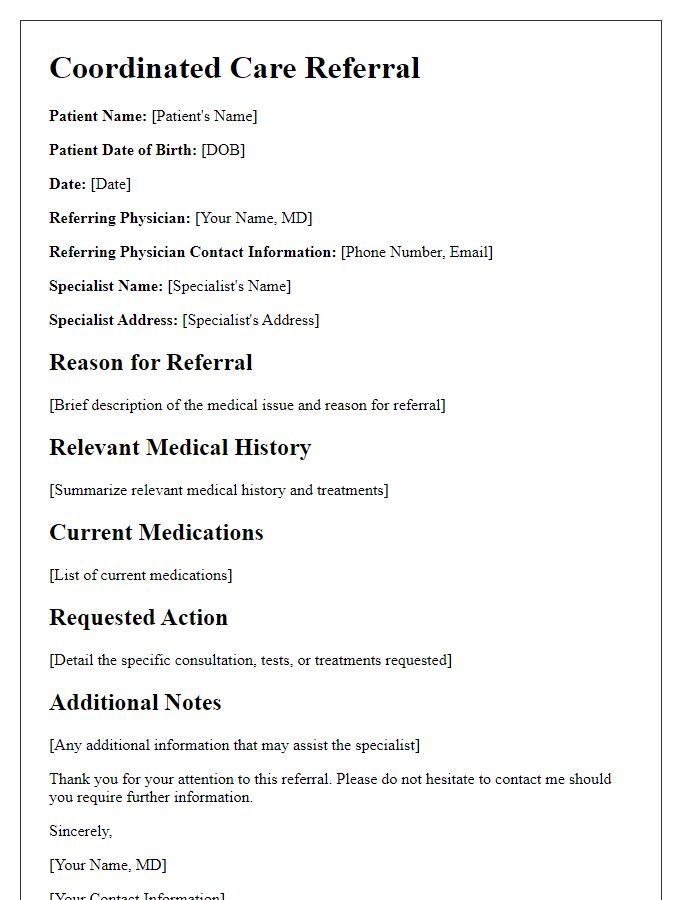
Patient referrals often require clear and detailed communication to ensure seamless transitions in care. The notification typically includes essential patient information such as the patient's full name (e.g., Johnathan Smith), date of birth (e.g., January 15, 1985), and medical record number (e.g., MRN 123456789). Additionally, crucial referral details should highlight the referring physician's name (e.g., Dr. Emily Jones) and contact information, specifying the specialty (e.g., cardiology) of the specialist (e.g., Dr. Robert White) to whom the patient is being referred. Important clinical information, such as diagnosis (e.g., hypertension) and relevant medical history, should be included to provide context for the specialist's review. Patients may also need to be informed about the appointment details, including date, time, and location (e.g., Cardiology Clinic, 123 Health St, Anytown) as well as any required preparations or tests prior to the visit.
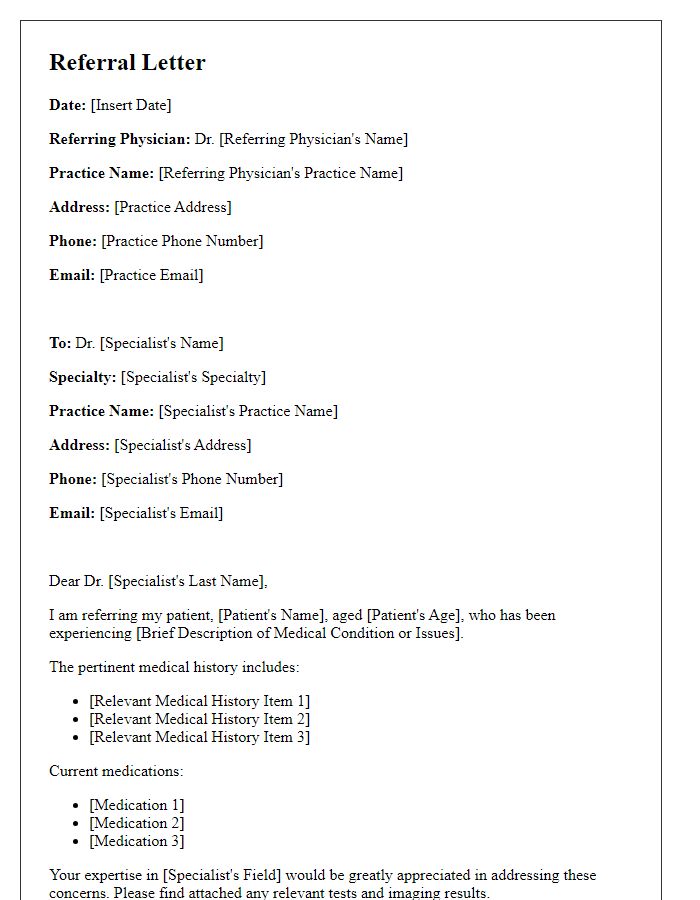
Referring Physician Details
Referring physician details include critical information that ensures effective communication and coordination in patient care. Key elements consist of the physician's full name, indicating credentials such as MD (Doctor of Medicine) or DO (Doctor of Osteopathic Medicine), along with the practice name, often located within a healthcare system like Massachusetts General Hospital. Contact details must include a direct phone number, usually formatted as (XXX) XXX-XXXX, a secure email address adhering to HIPAA guidelines, and the physical address of the practice to facilitate proper correspondence. Additional context may involve the specialty of the referring physician, such as Cardiology or Neurology, which can highlight the specific area of expertise relevant to the patient's condition. It's essential to include the patient's identification number or medical record number for accurate tracking and continuity of care.
Specialist's Information
A specialist referral notification provides essential information about the healthcare provider, ensuring proper communication in patient care. The specialist's name, such as Dr. John Smith, a board-certified orthopedic surgeon with over 15 years of experience at City Hospital of San Diego, is crucial. Contact details include a direct phone line, typically (555) 123-4567, and the specialist's office address, 123 Health Ave, San Diego, CA, 92101. It is important to note the specialties, exemplified by joint replacement and sports medicine, as specialties provide clarity on the care the patient requires. Additional context involves the referral reason, such as ongoing knee pain that affects mobility, with relevant patient information, including age (45) and relevant medical history, emphasizing the urgency of the referral.
Reason for Referral
Referral notifications often include essential details for proper understanding and follow-up. An effective referral notification should specify the patient's primary condition, such as chronic migraines, which may require evaluation from a neurologist specializing in headaches. Additionally, relevant medical history, including previous treatments like prescription medications or therapies, should be outlined clearly, especially indicating any adverse reactions or lack of efficacy. The referral should also highlight pertinent diagnostic tests, such as MRI scans taken in December 2022 that revealed no structural abnormalities, providing crucial context for the specialist. Proper documentation of the referring physician's contact details ensures an efficient communication process.
Required Documentation
A specialist referral notification requires essential documentation to ensure a seamless transfer of patient information. The required documents include a completed referral form that captures patient demographics, medical history, and presenting concerns. Additionally, the latest diagnostic results, such as imaging studies like MRI or CT scans, must accompany the referral to provide the specialist with crucial insights. Progress notes from recent consultations, detailing treatment plans and medications, are also vital for continuity of care. Finally, any relevant lab reports, including blood tests or biopsies, should be included to support the specialist's evaluation and subsequent recommendations.


Comments