When it comes to navigating allergies, having a well-structured management plan can make all the difference in ensuring safety and well-being. From identifying triggers to outlining emergency responses, a comprehensive letter can act as a guide for families, schools, and caregivers alike. It's essential to keep the communication clear and supportive, paving the way for understanding and collaboration. Ready to learn how to craft the perfect allergy management plan letter? Read on for helpful tips and templates!

Patient Information
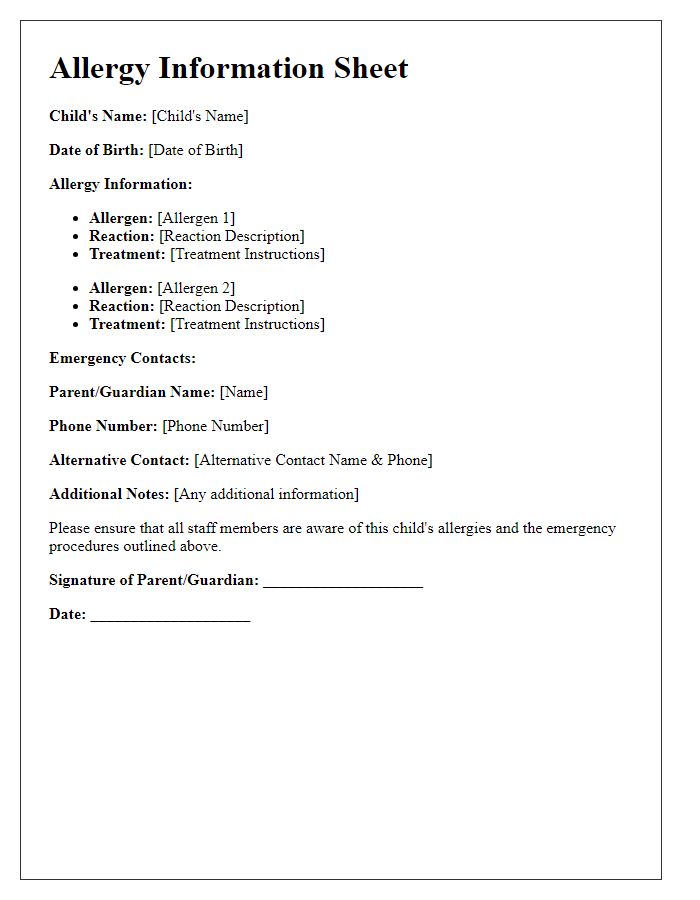
Patient information is essential for effective allergy management plans. Accurate details include name, age, address, and emergency contact numbers. Allergy history requires information on specific allergens identified, such as pollen from oak trees (Quercus) or dust mites (Dermatophagoides), along with documented reactions, including symptoms like hives or anaphylaxis. Medical history may involve previous treatments for allergies, such as antihistamines or epinephrine injections, and a record of healthcare providers involved in the patient's care, such as allergists or primary care physicians. Current medications should also be listed, including dosages and frequency, ensuring the elimination of potential drug interactions that may exacerbate allergic reactions. Regular updates to this information enhance the effectiveness of the overall allergy management strategy.
Allergy Triggers and Symptoms
An allergy management plan outlines critical details for individuals with allergies, emphasizing allergy triggers and associated symptoms. Common allergens include pollen from flowering plants, dust mites in household environments, certain food items like peanuts or shellfish, and insect stings from bees or wasps. Symptoms may manifest as skin reactions, such as hives or eczema, respiratory issues like asthma attacks or nasal congestion, and digestive disturbances including nausea or vomiting. Emergency situations might necessitate the use of epinephrine auto-injectors (EpiPens) in case of severe anaphylactic reactions, which require immediate medical attention. Proper identification and understanding of these elements are essential for effective allergy management.
Emergency Contact Details
Allergy management plans require detailed emergency contact information to ensure quick assistance during an allergic reaction. Primary contact should include parents or guardians, with mobile numbers specified for immediate communication; for example, Jane Doe, 555-1234. Additional contacts should provide backup support, such as a close relative; for instance, John Smith, 555-5678. It is crucial to include the physician's information, such as Dr. Emily Lee, Allergy Specialist, with office number 555-9876, along with any relevant hospital contact details, like City General Hospital, 555-4321, to facilitate prompt medical intervention. Clear labeling of contacts helps create a structured response during emergencies associated with allergic reactions.
Medication and Dosage Instructions
An effective allergy management plan requires precise medication and dosage instructions for individuals with allergies, specifically addressing various allergens like pollen, dust mites, and certain foods. Epicenters of allergens may include regions known for high pollen counts, such as the Southeastern United States during the spring months. First-line medications typically involve antihistamines, such as Cetirizine, at dosages of 10 mg once daily for adults, which can alleviate symptoms like itching and sneezing. Additionally, intranasal corticosteroids, like Fluticasone propionate, are recommended at a dosage of 200 mcg once daily to reduce nasal inflammation. For severe allergic reactions, individuals should carry EpiPens, which deliver 0.3 mg of epinephrine intramuscularly, necessary for emergency situations triggered by allergens, such as peanuts or bee stings. Each medication should be tailored to the individual's age, weight, and specific allergic triggers for optimal efficacy.
Action Steps for Allergic Reactions
Allergic reactions can vary in severity, making it essential to have a comprehensive allergy management plan. Immediate recognition of symptoms, such as hives or difficulty breathing, is crucial for effective response. For individuals with a known allergy, like peanuts or shellfish, carrying an epinephrine auto-injector (EpiPen) is mandatory. Each auto-injector typically contains a dose of 0.3 mg of epinephrine, which can counteract life-threatening anaphylaxis. Additionally, schools and workplaces should maintain a list of emergency contacts and locations of first-aid kits equipped with antihistamines. Regular training on identifying allergic reactions and administering treatments ensures preparedness. Storing medication properly, at room temperature and away from direct sunlight, is vital to maintain efficacy. Regular check-ups with an allergist provide updated action steps tailored to individual allergies.
Letter Template For Allergy Management Plan Samples
Letter template of Allergy Management Strategy for Healthcare Professionals


Comments