Navigating the complex world of healthcare compliance can feel overwhelming, but it doesn't have to be. Whether you're a healthcare provider trying to keep up with regulations or a patient looking to understand your rights, asking the right questions is essential. In this article, we'll explore a comprehensive letter template designed to help you inquire about critical compliance issues effectively. So, let's dive in and empower you with the knowledge you needâkeep reading to discover how to craft your inquiry!

Clear and concise language.
Healthcare compliance inquiries often involve intricate regulations and standards, such as HIPAA (Health Insurance Portability and Accountability Act) which governs patient information security. These inquiries ensure adherence to legal requirements, maintaining the integrity of patient care systems in institutions like hospitals or clinics. A thorough investigation may address aspects such as data handling processes, employee training programs, and incident response protocols. Engaging with compliance officers typically clarifies existing policies--vital for safeguarding patient rights and promoting organizational accountability. Regular audits can highlight areas for improvement, ensuring ongoing alignment with federal and state regulations that shape the healthcare landscape.
Specific compliance topics.
Healthcare compliance inquiries often focus on critical topics such as HIPAA regulations, which mandate the protection of patient data across healthcare entities, including providers and insurance companies. Key aspects include adherence to privacy standards and procedures for safeguarding protected health information (PHI), emphasizing the importance of staff training and policy implementation. Other significant areas include the Anti-Kickback Statute, which prohibits financial incentives that might influence medical decisions, and Stark Law, which prevents physician self-referrals in Medicare-covered services. Regular audits and assessments are essential for ensuring compliance, and failure to adhere to these regulations can result in substantial fines and legal challenges, impacting the integrity of healthcare organizations in the United States.
Relevant documentation requests.
Healthcare compliance involves a thorough examination of regulations and practices within medical facilities. Documentation requests often include policies from the Health Insurance Portability and Accountability Act (HIPAA) regarding patient privacy (enforced since 1996), training records for employees on compliance standards (typically updated every year), and audit reports from the Office for Civil Rights (OCR) that assess adherence to federal guidelines. Additional documents might encompass incident reports related to compliance violations, quality control checklists, and meeting minutes from compliance committee gatherings held quarterly, which ensure that all staff remain informed on legal responsibilities and ethical standards in patient care. Properly maintained documentation is crucial for demonstrating compliance during inspections and preventing legal repercussions.
Contact information for follow-up.
Inquiries regarding healthcare compliance often necessitate clarity in communication and detailed contact information. Compliance officers must ensure their inquiries address specific regulations, such as HIPAA (Health Insurance Portability and Accountability Act) and Medicare guidelines. Key details in follow-up communication may include names of compliance personnel, direct phone numbers, email addresses, and mailing addresses for corporate offices, typically located in significant healthcare hubs like Washington, D.C., or specific state capitals. Additionally, establishing a timeline for response--often within 10 business days--can streamline the process. Maintaining transparency about the nature of the inquiry, including all pertinent regulations involved, reinforces the importance of efficient compliance practices.
Deadline for response.
Health organizations often face scrutiny regarding compliance with regulations, such as HIPAA (Health Insurance Portability and Accountability Act) in the United States. A formal inquiry may require a deadline for response, typically ranging from 30 to 60 days, depending on the complexity of the questions posed. This timeline is crucial for ensuring timely updates regarding compliance practices, privacy protections, and data management procedures. Communication regarding deadlines must clearly specify the date by which responses should be submitted, often aligning with regulatory standards and internal policy protocols to maintain accountability within the organization's operations.
Letter Template For Healthcare Compliance Inquiry Samples
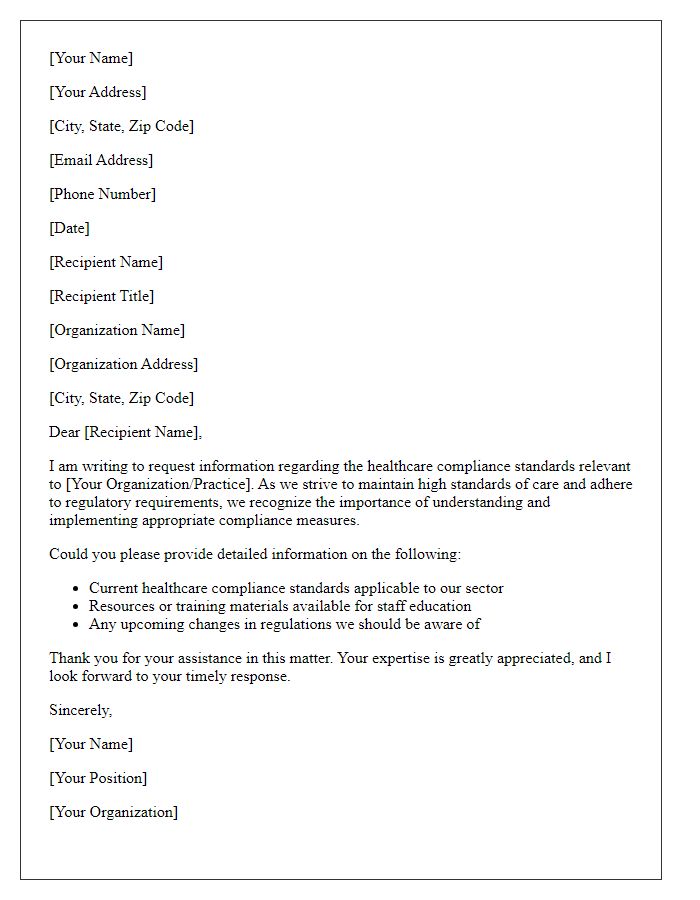
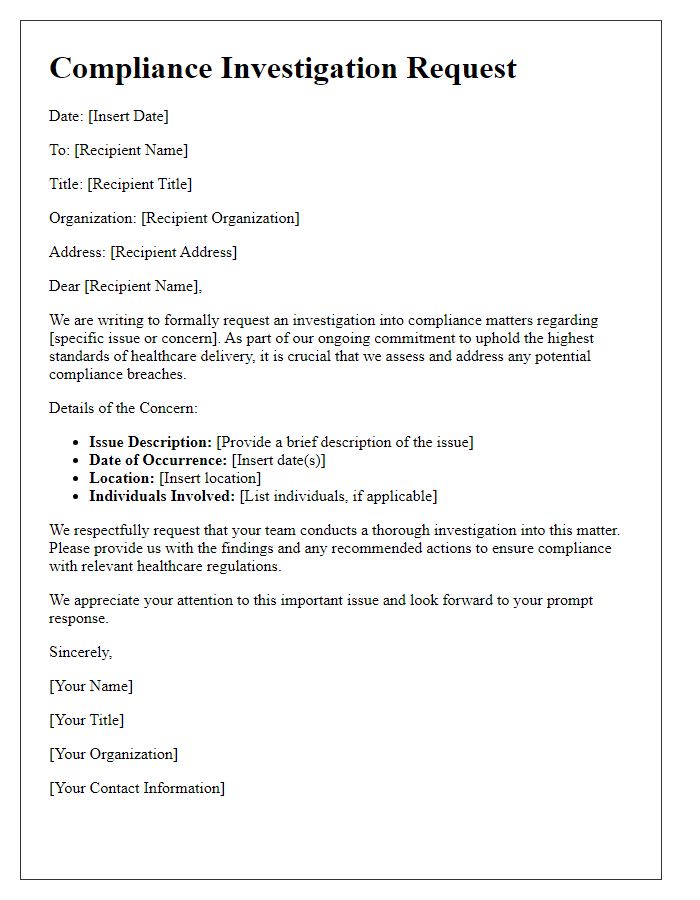
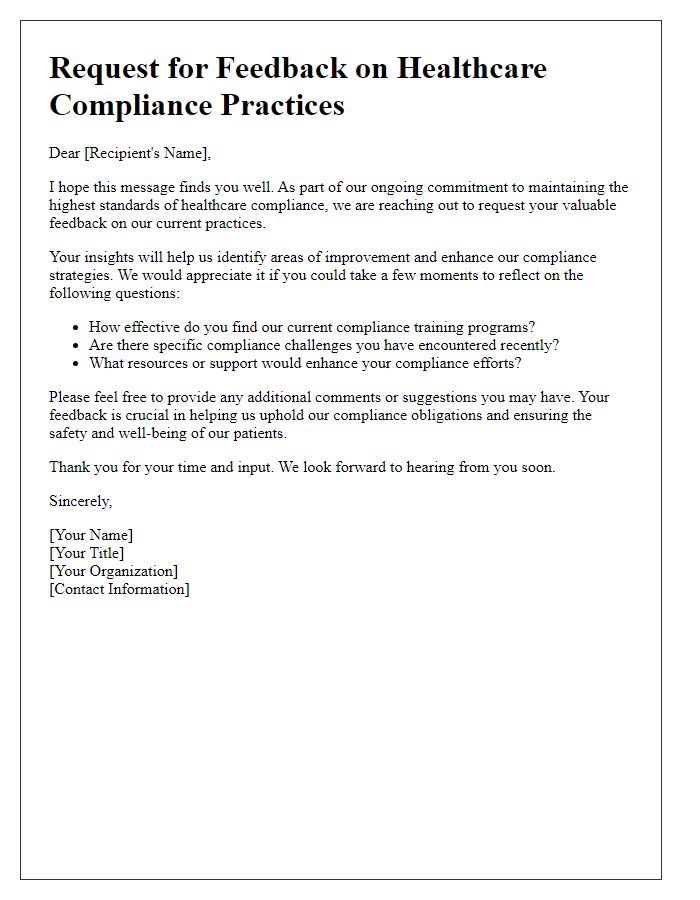
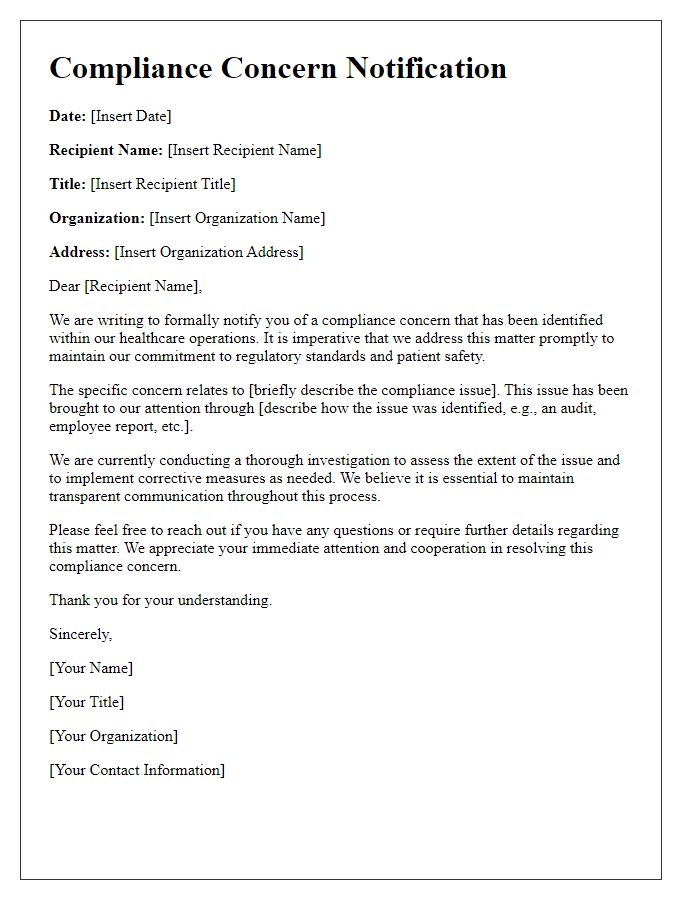
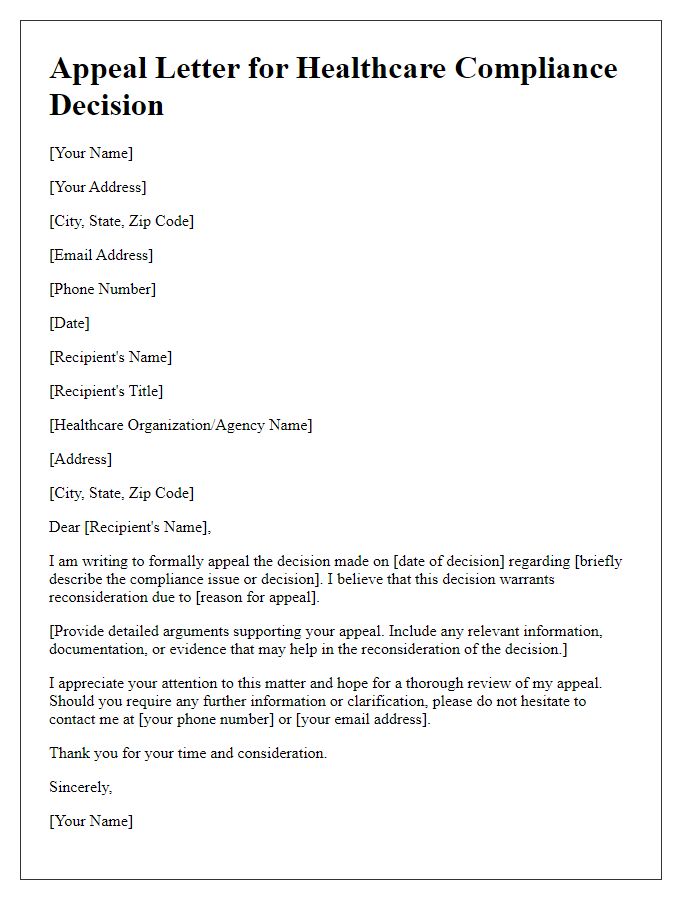
Letter template of request for information on healthcare compliance standards
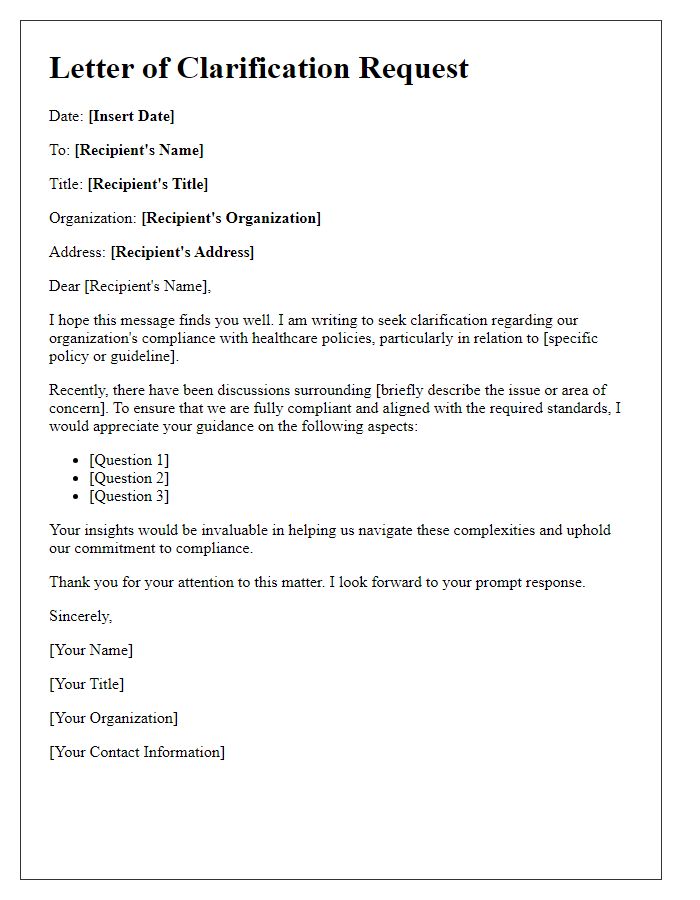
Letter template of clarification needed on healthcare compliance policies
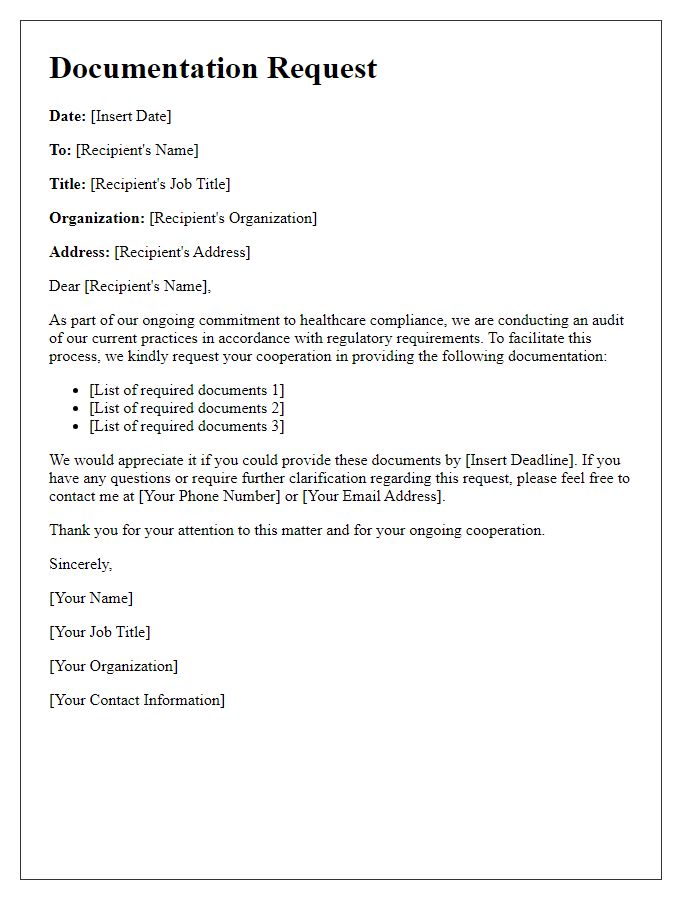
Letter template of documentation request for healthcare compliance audit
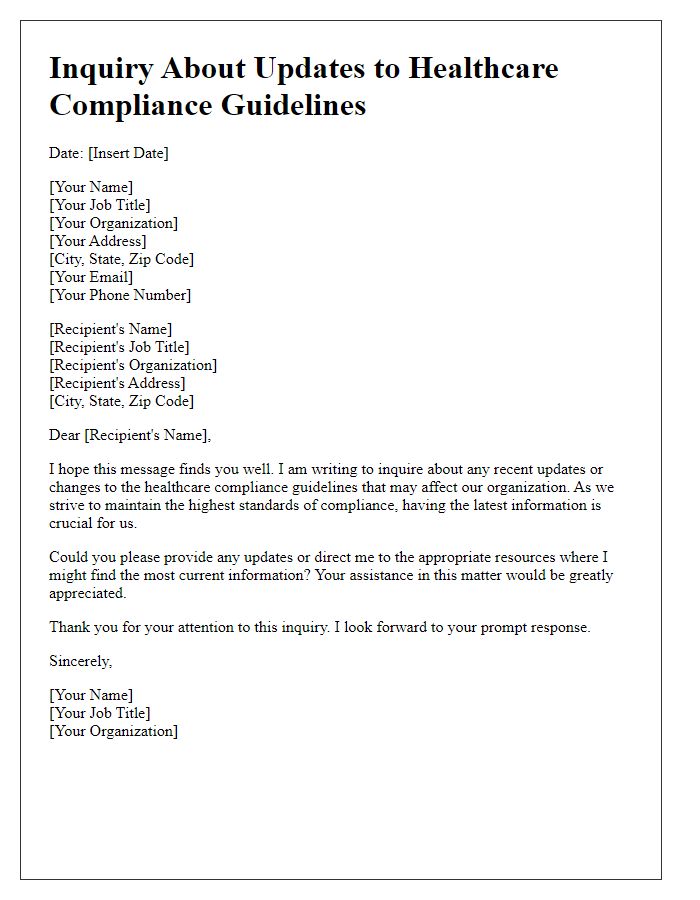
Letter template of inquiry about updates to healthcare compliance guidelines



Comments