In the complex world of medical malpractice defense, clear communication is paramount. Whether you're defending a practitioner or institution, understanding the nuances can make all the difference in achieving a successful outcome. This article aims to break down essential strategies and considerations to effectively navigate these challenging waters. So, join us as we dive deeper into the intricacies of medical malpractice defense!
Legal and Medical Terminology Precision
Medical malpractice defense requires meticulous attention to legal and medical terminology. In cases involving alleged negligence, the defense must articulate the standard of care expected of healthcare providers such as physicians or nurses, often defined by guidelines established by authoritative bodies like the American Medical Association. Legal definitions of malpractice must include evidenced failure to meet this standard, leading to patient harm, documented through medical records, treatment plans, and expert testimonies. Jurisdictions vary, with statutes of limitations impacting the timeline for filing claims. Understanding causation--demonstrating that the alleged negligence directly resulted in damages, such as physical injury or financial loss--remains a crucial element in formulating a robust defense strategy. Key terms like "foreseeability," "informed consent," and "burden of proof" are essential to navigate this complex legal landscape effectively.
Case Details and Incident Summary
In a medical malpractice defense case, a surgical error can occur during a procedure such as appendectomy, which is aimed at removing the inflamed appendix. The incident may involve an experienced surgeon operating on a 35-year-old patient at St. Mary's Hospital, known for its advanced surgical technologies. During the operation on April 12, 2023, a critical mistake could happen, where the surgeon unintentionally nicks the small intestine, leading to complications. These complications might include infection or bowel obstruction, which require subsequent hospital admissions and further treatments. Medical records show the patient's vital signs remained stable prior to the mishap, indicating no pre-existing conditions that would complicate the procedure. Expert testimonies will be crucial in evaluating whether the surgeon met the standard of care expected in similar medical scenarios, ultimately influencing the case outcome.
Defense Arguments and Evidence Presentation
In medical malpractice cases, defense arguments often focus on establishing adherence to established medical standards and demonstrating that the healthcare provider acted in a reasonable manner under the circumstances. Key evidence may include detailed medical records, expert testimony from board-certified specialists in relevant fields, and documentation of the patient's history and treatment plan. In addition, statistical data may reveal that the incidence of alleged malpractice is within acceptable ranges for similar cases. Furthermore, maintaining comprehensive communications, such as consent forms and follow-up notes, can strengthen the argument that informed consent was obtained during the patient-provider interaction. Notable examples may involve cases adjudicated in jurisdictions like California, where the standard of care is meticulously defined by state medical boards. Defense strategies may also reference landmark rulings that have shaped malpractice law, such as the 1979 case of Helling v. Carey, which addressed informed consent principles. Overall, the focus remains on establishing the healthcare provider's actions as consistent with the medical community's expectations and standards of care, effectively mitigating any claims of negligence or wrongdoing.
Applicable Laws and Regulations
Medical malpractice defense involves navigating complex legal frameworks to protect healthcare professionals from liability. Key laws include the Medical Malpractice Act, which varies by state, establishing standards for proving negligence, such as the applicable standard of care, breach of duty, causation, and damages. In states like California, the statute of limitations for filing a medical malpractice claim is limited to three years from the date of injury or one year from discovery of the injury, with certain exceptions. Regulations set forth by the National Practitioner Data Bank (NPDB) require reporting of malpractice payments and adverse actions against healthcare providers, which can significantly impact a practitioner's reputation. Additionally, tort reform measures in states such as Texas impose caps on non-economic damages, influencing settlement negotiations and trial outcomes. Understanding these laws and regulations is crucial for effectively mounting a defense in medical malpractice cases.
Professional Tone and Confidentiality Compliance
Medical malpractice defense involves intricate legal strategies to address allegations against healthcare professionals. In such cases, the role of the defense attorney is crucial in scrutinizing medical records, which contain patient data, treatment histories, and procedural documentation. Effective defense requires thorough examination of relevant statutes, such as state-specific malpractice laws and tort reform measures, influencing case outcomes. Expert witnesses, often seasoned medical practitioners or specialists (such as surgeons or anesthesiologists), may provide testimony regarding standard of care practices. Confidentiality compliance is vital, ensuring adherence to regulations like HIPAA (Health Insurance Portability and Accountability Act), safeguarding patient information during legal proceedings. A robust defense often hinges on the ability to establish reasonable care and procedural adherence while countering claims of negligence or malpractice in high-stakes environments, such as emergency rooms or surgical units.
Letter Template For Medical Malpractice Defense Samples
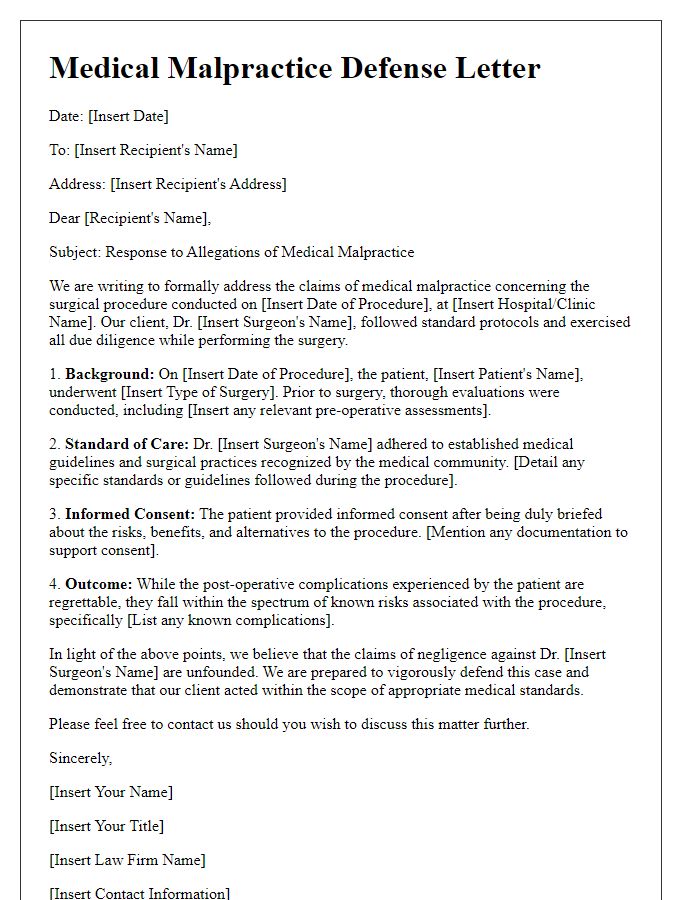
Letter template of medical malpractice defense for a surgical procedure.
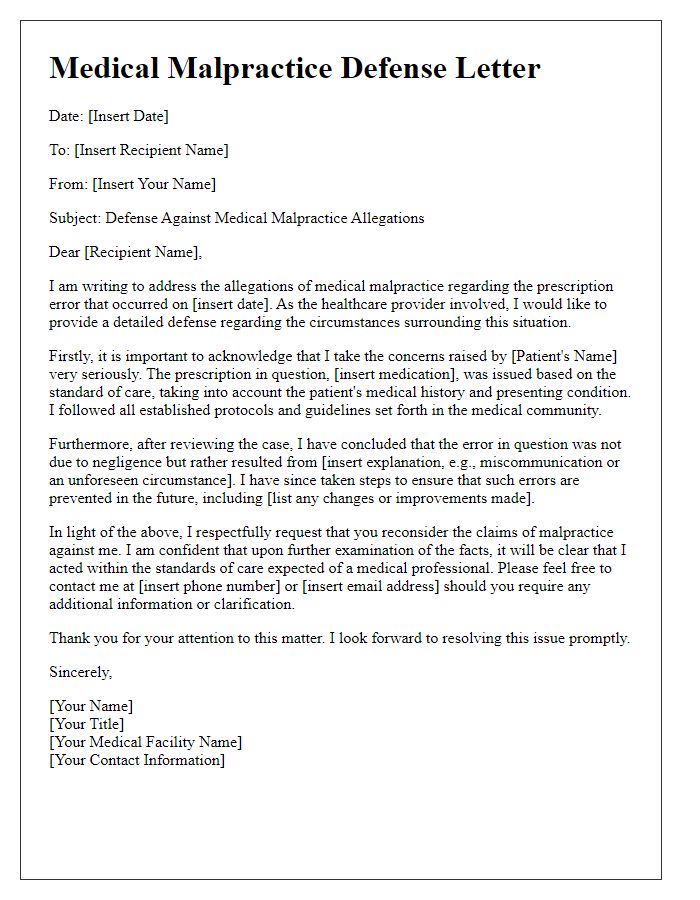
Letter template of medical malpractice defense for a prescription mistake.
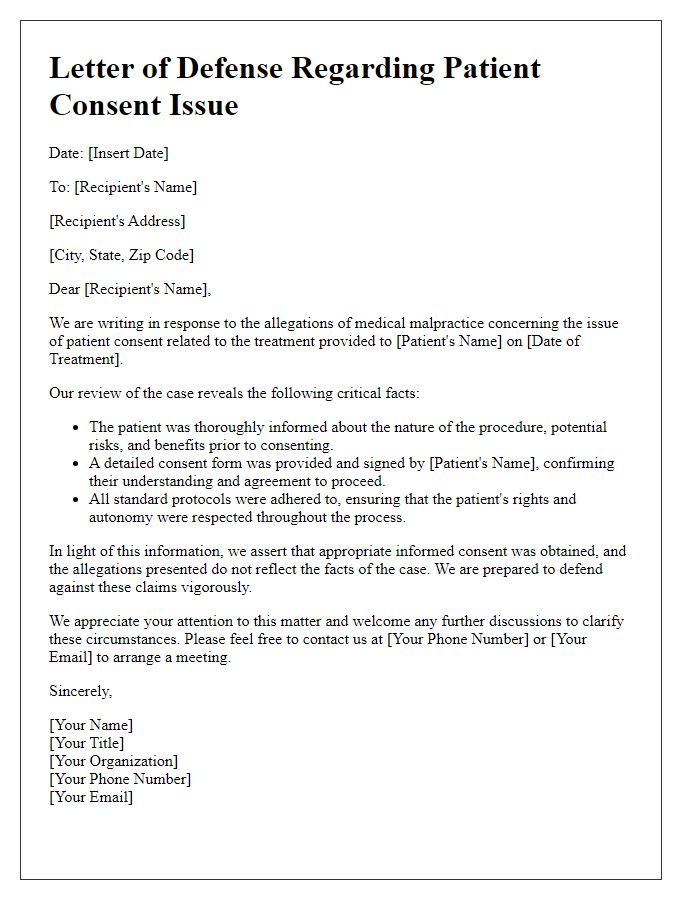
Letter template of medical malpractice defense for a patient consent issue.



Comments