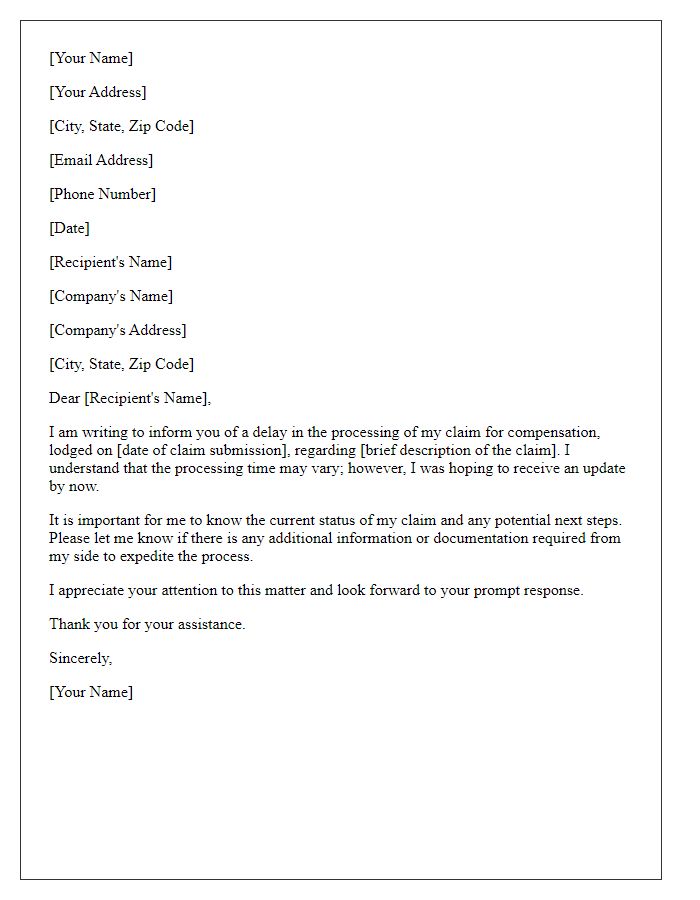
Have you ever found yourself anxiously waiting for a payment that seems to be just out of reach? It can be frustrating to chase after what's rightfully yours, especially when unexpected delays occur. In this article, we'll guide you through the essential steps to effectively communicate a claim payment delay to ensure your concerns are addressed promptly. So, let's dive in and uncover the key strategies to help you resolve this issue swiftly!
Claim Reference Number
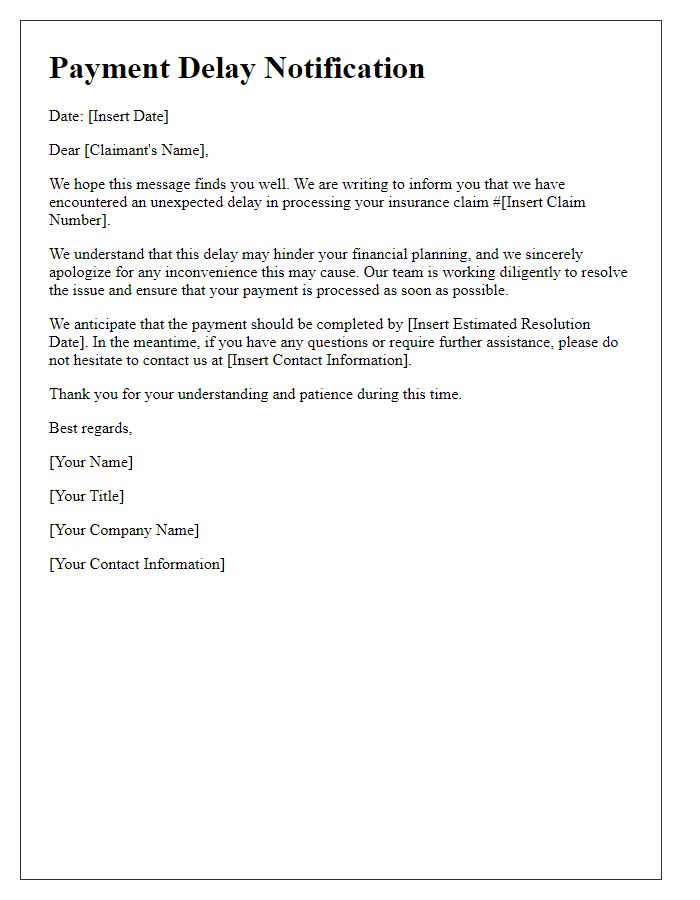
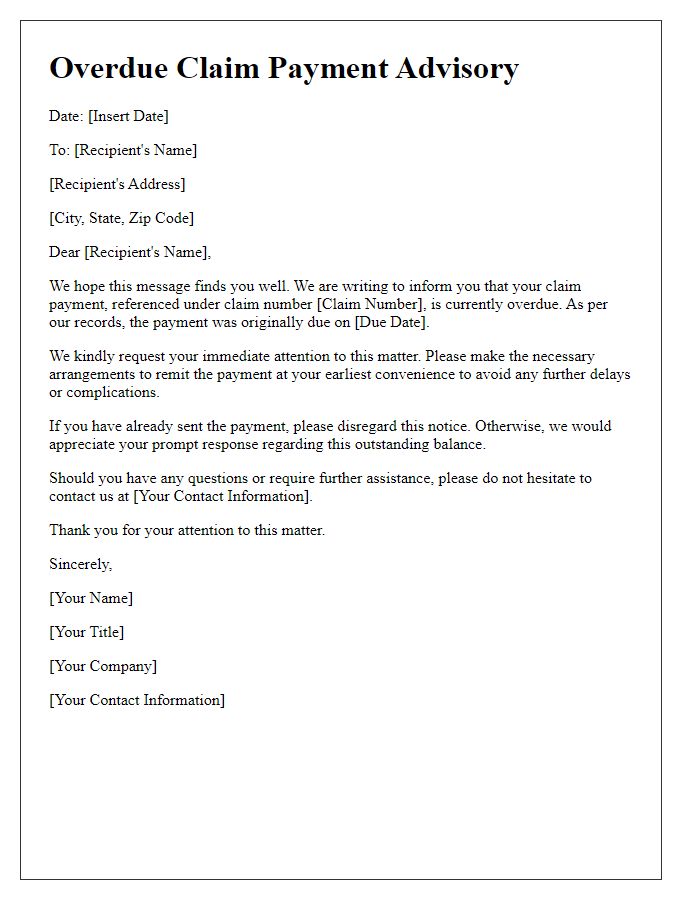
Claim payment delays can cause frustration for policyholders awaiting compensation. The claim reference number serves as a unique identifier for the specific incident, facilitating communication with the insurance provider. Typical delays may stem from additional documentation requests, insurer internal reviews, or the complexity of the claim itself. Policyholders often experience increased anxiety when payments are postponed beyond the expected timeframe, which can range from a few days to several weeks depending on the insurer's processing capabilities. To mitigate these concerns, insurance companies often provide customer service avenues to address inquiries and updates regarding claim statuses.
Policyholder Details
Policyholders encountering delays in claim payments may experience frustration and uncertainty regarding their financial security. Claim processing times can vary significantly based on several factors, including the complexity of the claim, the insurer's internal workload, and regulatory requirements in different jurisdictions. For example, the average processing time for auto insurance claims can range from a few days to several weeks, depending on the severity of the accident and the availability of necessary documentation. Claim adjusters, responsible for reviewing and approving claims, may require additional information or clarification, contributing to potential delays. Effective communication from insurers, including regular updates on the status of claims and anticipated resolution timelines, can alleviate policyholders' concerns and enhance their customer experience.
Description of Delay
Claim payment delays can severely impact financial stability for individuals and businesses alike. Payment processing systems in various insurance companies, such as XYZ Insurance, may experience inefficiencies (e.g., software bugs or increased claim volume). Delays often extend beyond the standard processing time of 30 days, sometimes reaching over 60 days, causing frustration among policyholders. Internal audits within claims departments can reveal bottlenecks, particularly in complex cases or when additional documentation is required. Additionally, communication breakdowns with third-party providers or assessments can exacerbate the situation, leading to misunderstandings regarding payment timelines. Overall, addressing these delays requires immediate attention to both technological systems and operational workflows to restore trust and guarantee timely payments.
Requested Resolution Timeframe
Claim payment delays can significantly impact individuals and businesses, particularly in the insurance industry. Customers may experience financial strain due to unforeseen circumstances, such as medical emergencies or property damage events. Payment delays can extend to several weeks, sometimes exceeding 30 days in complex claims involving multiple documentation reviews. The claims process may involve adjustment assessments from licensed adjusters or further investigations into fraud, requiring additional time. Transparency and communication from the insurer regarding expected resolution timeframes, ideally communicated through official channels like emails or customer service representatives, are crucial to maintaining trust. Timely notifications regarding the status of claims can alleviate frustration and reduce uncertainty for affected parties.
Contact Information for Follow-up
Delayed claims payment can cause significant financial challenges for individuals and businesses. Timely processing, ideally within 30 days, is crucial for maintaining cash flow. Claim numbers, such as reference IDs, can assist in tracking these payments. Policyholders should maintain accurate documentation, including receipts and correspondence, to facilitate follow-up. Contact information for claims departments should be readily available, typically found on official websites or policy documents, to ensure effective communication. Regular follow-up within a week of submission can help expedite resolution, emphasizing the importance of keeping records of all interactions related to claims.



Comments