Hey there! If you're navigating the beautiful yet challenging journey of postpartum care, you're not alone. This letter serves as a handy template to guide you through essential practices that promote healing and well-being during this significant transition. With support and resources at your fingertips, you're sure to make the most of this precious timeâread on to discover more!
Individualized Care Approach
Postpartum care guidelines emphasize an individualized care approach to support mothers after childbirth. Each woman's recovery journey is unique, factoring in physical and emotional challenges. Healthcare providers should assess vital signs, including blood pressure and heart rate, to monitor maternal health and identify complications promptly. Mental health screenings, such as the Edinburgh Postnatal Depression Scale, can help detect postpartum depression in approximately 10-15% of new mothers. Additionally, providing education on lactation techniques, addressing common issues like engorgement or sore nipples, can enhance breastfeeding success rates. Follow-up appointments within 6 weeks of delivery allow for personalized assessments and the development of tailored plans, ensuring mothers receive comprehensive support during this critical time. Emotional support networks, including family involvement and peer support groups like La Leche League, provide essential resources encouraging positive adjustments to motherhood.
Communication and Empathy
Effective postpartum care emphasizes the importance of communication and empathy, vital components for new mothers. Medical professionals, including obstetricians and nurses (roles crucial in maternal care), must engage in active listening, allowing mothers to express feelings, concerns, and experiences following childbirth. Empathetic communication cultivates trust, essential in discussions about physical health, mental well-being, and infant care challenges. Offering resources, such as local support groups or mental health services, assists in creating a safety net for emotional support. Regular check-ins during postpartum visits (typically scheduled six weeks post-delivery) ensure mothers feel heard and validated, promoting a healthy recovery environment. Recognizing red flags, such as signs of postpartum depression (affecting approximately 15% of new mothers), can guide timely intervention, further underscoring the role of compassion in enhancing the overall postpartum experience.
Cultural Sensitivity
Cultural sensitivity in post-partum care is vital for supporting new mothers from diverse backgrounds, such as African American, Hispanic, Asian, or Native American communities. Understanding specific cultural practices and beliefs surrounding childbirth and recovery, such as dietary restrictions, family dynamics, and traditional healing methods, enhances the care experience. Healthcare providers should respect practices like the "sit month" in Chinese culture, advocating for rest and nourishment during the recovery phase. Open communication will promote trust, encouraging mothers to discuss preferences, values, and concerns. Incorporating cultural practices into post-partum education can improve maternal mental health outcomes, ensuring mothers feel valued and understood in their care journey.
Support System Integration
Support systems play a crucial role in post-partum care for new mothers, ensuring their physical and emotional well-being. Family members, especially partners and grandparents, should actively participate in caregiving, providing assistance with daily tasks like feeding, diaper changing, and household chores. Local community resources, such as parenting groups and lactation consultants, can offer essential support, fostering connections and sharing valuable information. Mental health professionals should be easily accessible, addressing potential concerns such as postpartum depression, which affects approximately 1 in 7 women within the first year after childbirth. Healthcare providers must promote open communication, encouraging mothers to express their feelings and needs. Practical resources like meal delivery services or babysitting co-ops can alleviate stress, allowing new parents to focus on recovery and bonding with their infant.
Health and Safety Protocols
Postpartum care guidelines are essential for new mothers recovering after childbirth, focusing on health and safety protocols. The critical period typically encompasses the first six weeks postpartum, when physical and emotional changes occur. Regular monitoring of vital signs, including temperature (normal range is 36.1 to 37.2 degrees Celsius), assists in identifying potential complications such as infection. Breastfeeding education emphasizes benefits like improved maternal-infant bonding, while guidance on recognizing latch issues and engorgement provides necessary support. Postpartum depression screening involves tools like the Edinburgh Postnatal Depression Scale, facilitating early intervention. Additionally, pelvic floor exercises bolster recovery, reducing risks associated with conditions like incontinence. Overall, adherence to these protocols promotes maternal health and ensures a smoother transition for new families.
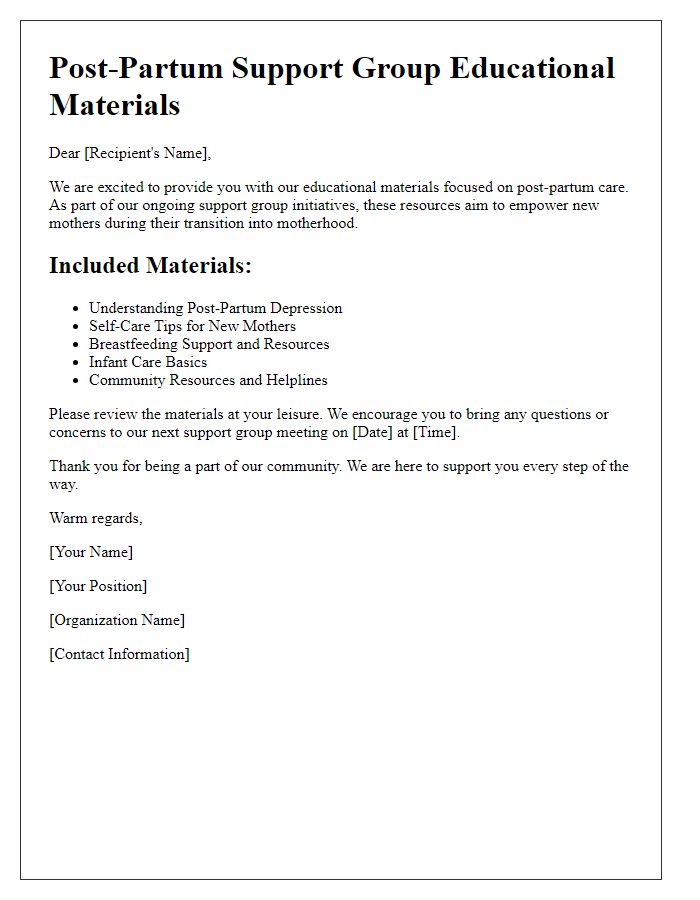
Letter Template For Post-Partum Care Guidelines Samples
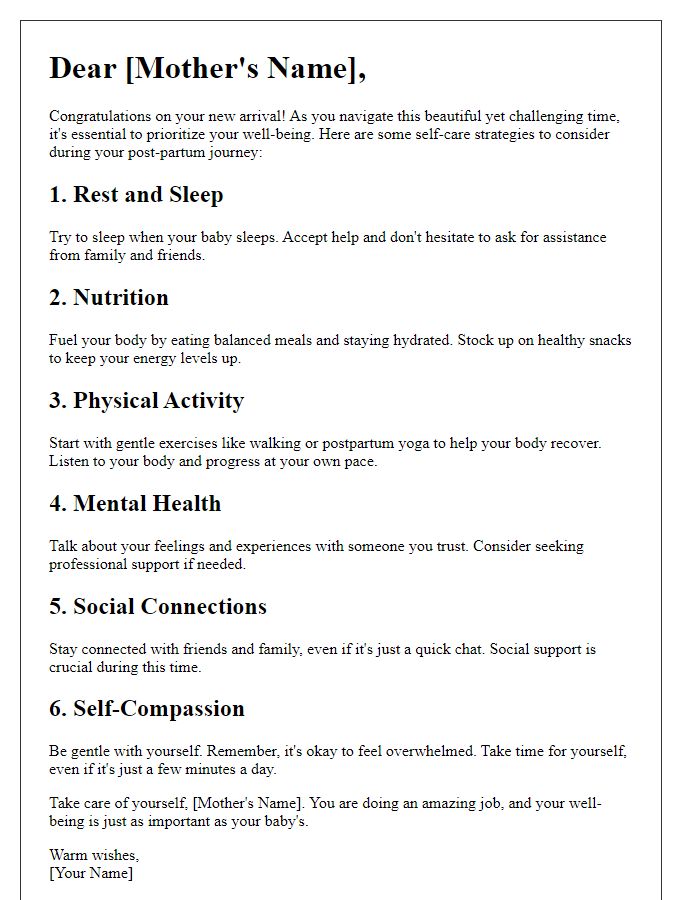
Letter template of post-partum wellness instructions for healthcare providers.
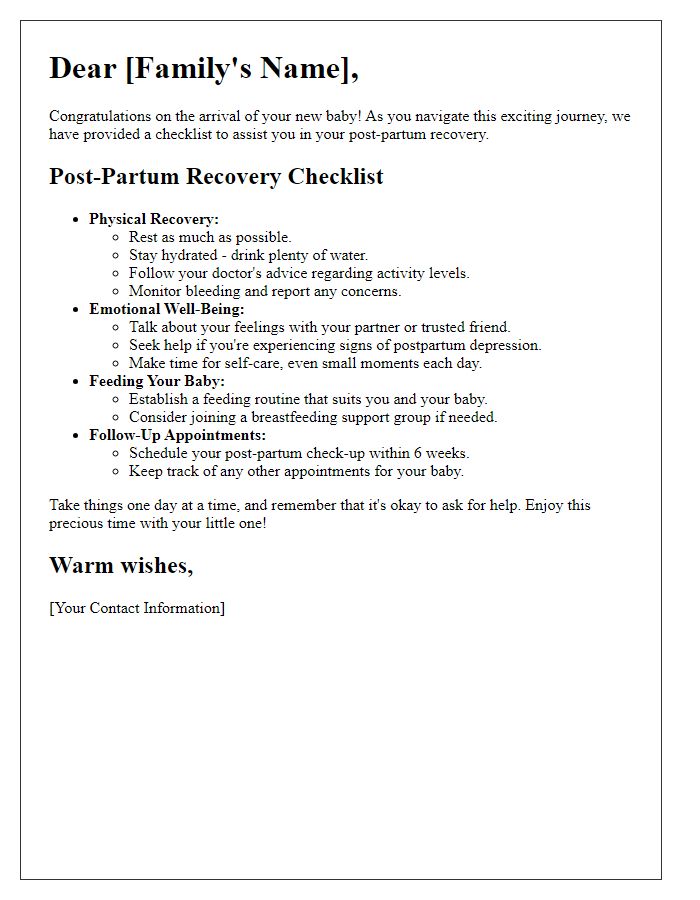
Letter template of post-partum mental health considerations for parents.
Letter template of post-partum nutrition tips for breastfeeding mothers.
Letter template of post-partum physical activity guidelines for new parents.


Comments