Navigating the world of healthcare can often feel overwhelming, especially when it comes to securing the necessary approvals for treatment. One crucial step in this process is the prior authorization request, which helps ensure that your insurance covers the medical services you need. In this article, we'll guide you through a helpful letter template designed specifically for communicating with your insurer about prior authorization. Ready to take the next step towards getting the care you deserve? Let's dive in!
Patient Information
Prior authorization requests for insurer approval often require detailed patient information to facilitate the approval process. Patient name, age, and medical history must be accurately provided. Identification numbers such as Social Security number and policy number are essential for verification purposes. Specific conditions or diagnoses should be clearly outlined, including any relevant ICD-10 codes that categorize the patient's health issues. It is also important to document ongoing treatments or medications, providing details such as dosages and duration, to demonstrate medical necessity. Additionally, any previous consultations or specialist opinions relevant to the patient's condition must be included to strengthen the case for authorization. This comprehensive approach ensures that insurers have all pertinent information needed for timely decision-making.
Diagnosis and Medical Necessity
Prior authorization requests for medical procedures are essential in ensuring that patients receive necessary care while adhering to insurer guidelines. Specific diagnoses such as severe asthma or advanced diabetes often require medication and treatment such as inhalers or insulin pumps. Medical necessity for these treatments is determined by recent clinical guidelines and guidelines from organizations like the American Diabetes Association for diabetes care management. Additionally, supporting documentation including lab results, physician notes, and treatment history can illustrate the urgency and importance of the requested authorization. Insurers typically review these requests within a set timeframe, often 5 to 14 days, depending on the policy specifics, while expedited requests may be prioritized within 72 hours for urgent cases.
Treatment and Services Requested
Prior authorization requests for medical treatments and services are essential for ensuring coverage by health insurers. Comprehensive documentation is critical to facilitate the approval process, often requiring detailed descriptions of the specific treatment or service, including the medical rationale. Commonly requested treatments might include advanced imaging procedures like MRI (Magnetic Resonance Imaging) which can cost upwards of $2,000, or specialized services such as physical therapy (typically involving multiple sessions and lasting several weeks). Additionally, information about the patient's medical history, relevant diagnoses (e.g., chronic pain due to a specific injury), and any previous treatments attempted should be included to justify necessity. Timely submission of requests can significantly influence the approval timeline, ensuring that patients receive the necessary care without unnecessary delays.
Supporting Documentation
A prior authorization request for medical procedures often requires extensive supporting documentation to ensure the insurer, such as Blue Cross Blue Shield or UnitedHealthcare, has all necessary information for review. Essential components of this documentation include a detailed letter from the physician outlining the diagnosis, the specific procedure or medication requested, and the medical necessity based on evidence-based guidelines. Relevant patient history, such as previous treatments attempted and outcomes, should be attached to provide context. Additionally, clinical notes from visits, results from diagnostic tests (like MRI scans or blood tests), and any applicable treatment plans are crucial. In some cases, peer-reviewed journal articles or clinical guidelines supporting the necessity of the treatment may enhance the request's credibility. All documents must be clearly labeled with patient identifiers and reference numbers to streamline processing by the insurance provider.
Contact Information and Follow-up Procedures
Contacting an insurer for prior authorization requests involves important details, such as specific contact numbers and email addresses. Insurers like Blue Cross Blue Shield or Aetna typically have dedicated customer service lines, often accessed at 1-800-xxx-xxxx for inquiries related to prior authorizations. Follow-up procedures commonly include a defined time frame, usually within 5 to 10 business days, allowing healthcare providers to communicate effectively. Written documentation may also include submission guidelines, such as using designated forms or secure portals like Availity for submission to streamline the process. Understanding these details can significantly enhance the efficiency of obtaining necessary approvals for medical treatments or procedures.
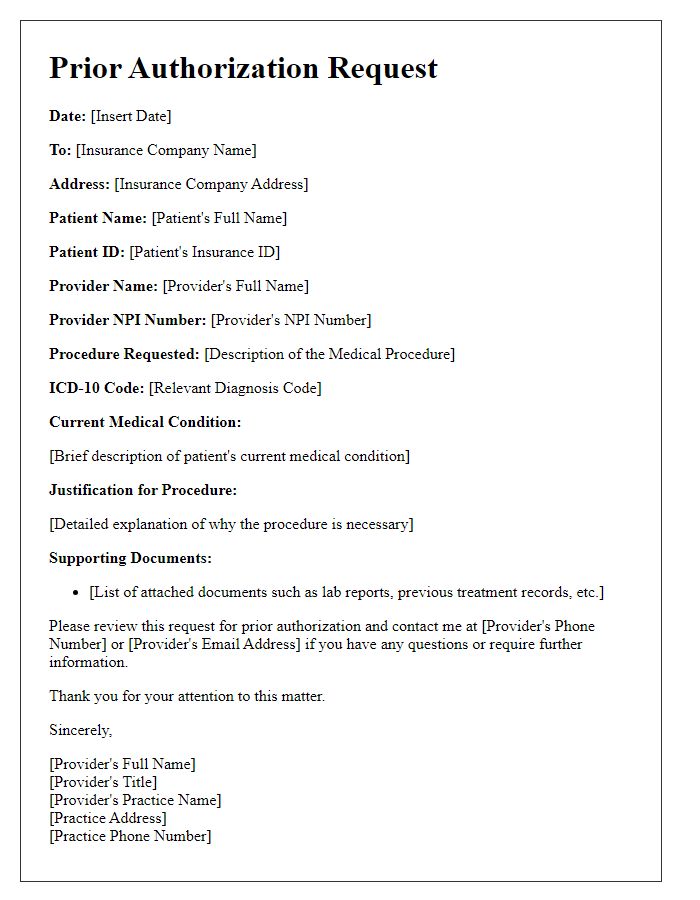
Letter Template For Prior Authorization Request To Insurer Samples
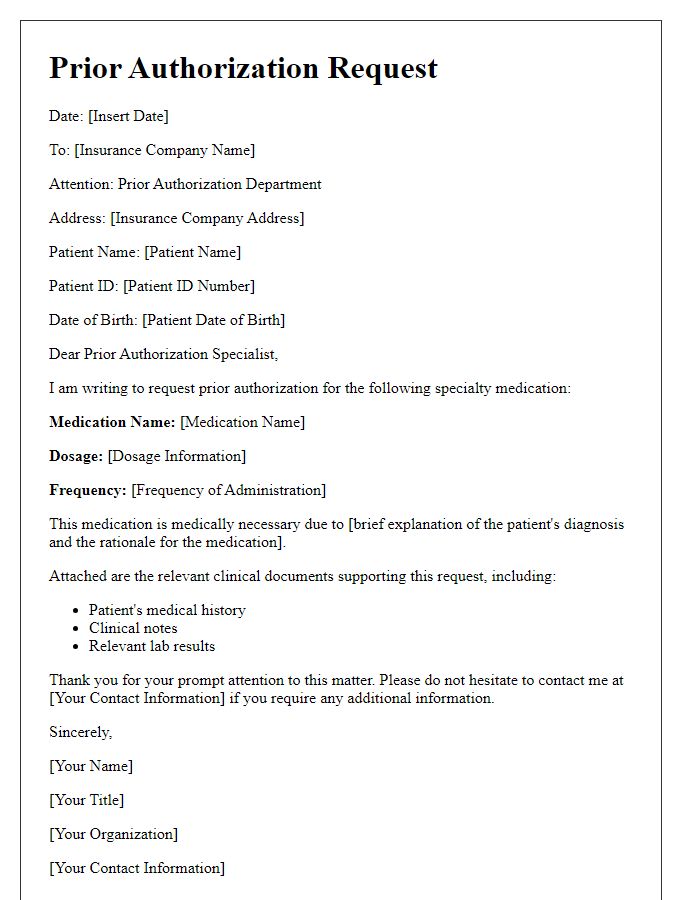
Letter template of prior authorization request for specialty medication.
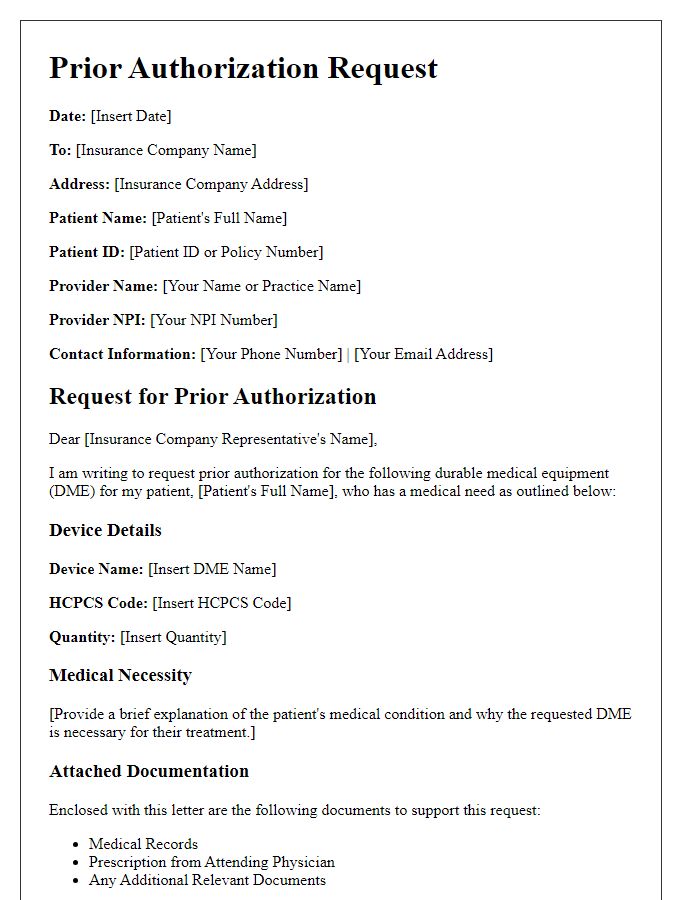
Letter template of prior authorization request for durable medical equipment.
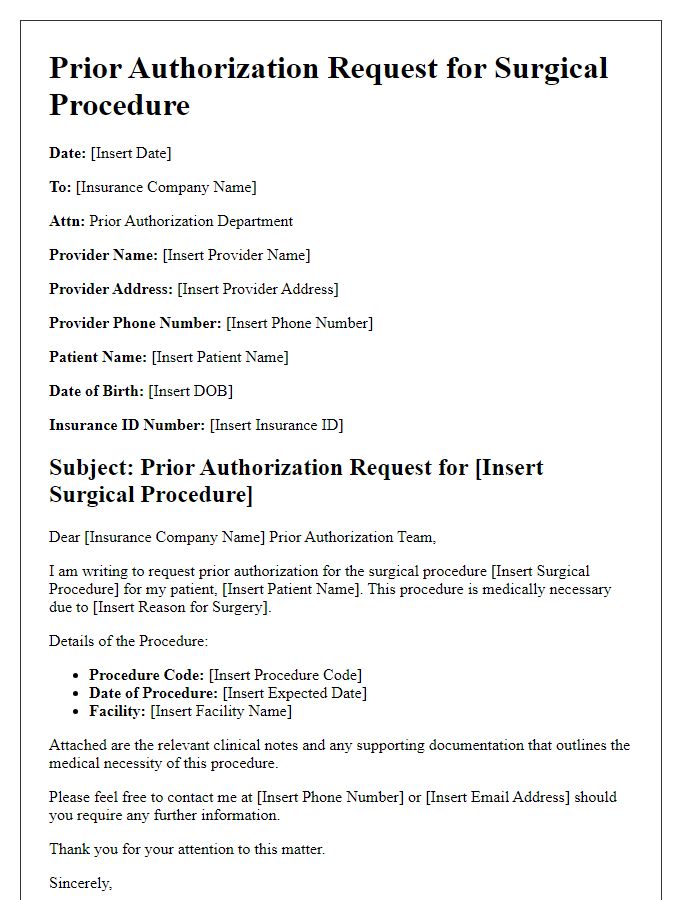
Letter template of prior authorization request for a surgical procedure.
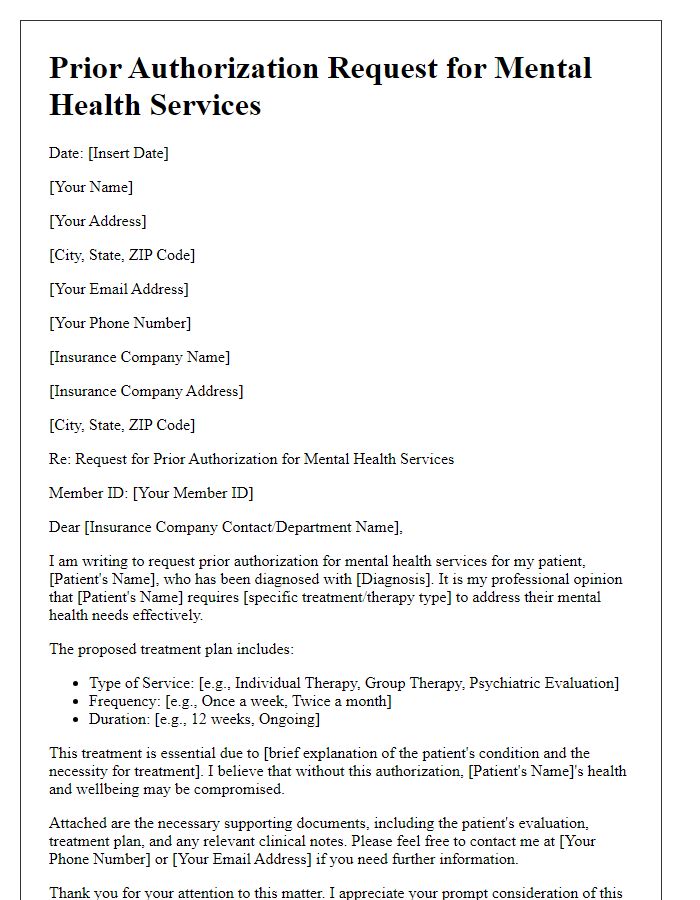
Letter template of prior authorization request for mental health services.
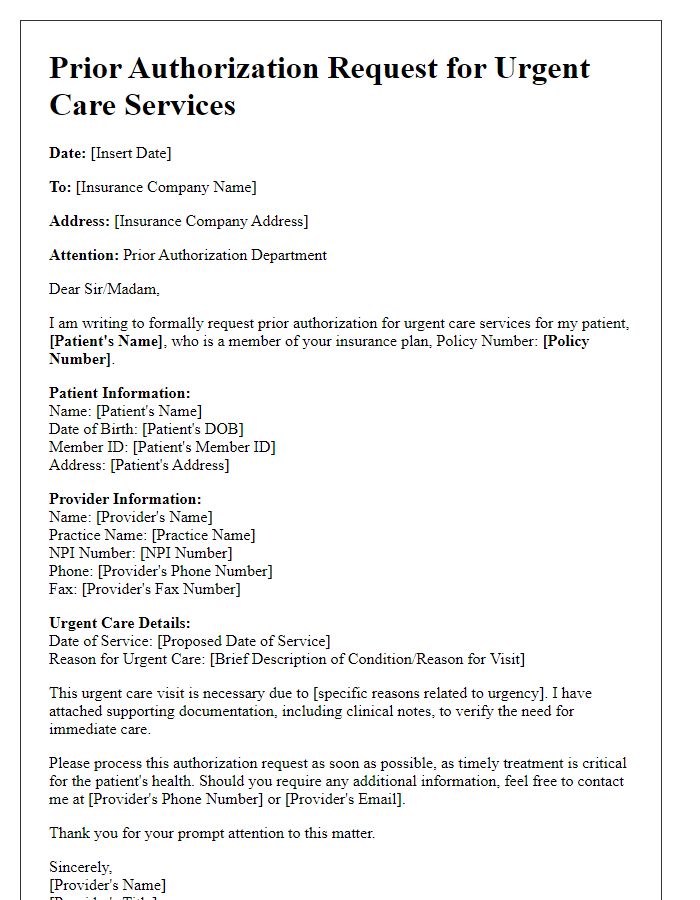
Letter template of prior authorization request for urgent care services.

Comments