Hey there! If you've recently had an appointment with your primary care physician, you might be wondering what comes next in your journey toward better health. Follow-up consultations are a crucial part of internal medicine, as they provide an opportunity to assess your progress and address any ongoing concerns. In this article, we'll guide you through what to expect during a follow-up visit and how to prepare effectively for your consultation. So, let's dive in and explore how you can make the most of your next appointment!
Patient Identification Information
Patient identification information is crucial for effective internal medicine follow-up consultations. Essential data includes the patient's full name, typically formatted as First Last, along with date of birth to establish identity. Medical record number plays a vital role in tracking the patient's history within the healthcare system. Contact information should include current phone number and address for appointment reminders and necessary communications. Additionally, insurance information is necessary to facilitate billing processes and verify coverage details. Each of these components ensures accurate and efficient patient management in healthcare settings, promoting continuity of care and seamless communication among medical professionals.
Appointment Details and Purpose
A follow-up consultation for internal medicine is essential for assessing chronic health conditions such as Type 2 Diabetes, Hypertension, and Hyperlipidemia. Appointments typically last approximately 30 minutes, allowing the physician to review lab results, update treatment plans, and address patient concerns. Scheduling can often be done at specialized clinics like the Mayo Clinic in Rochester, Minnesota, or through local healthcare providers. Documentation of medication adherence, lifestyle changes, and any new symptoms experienced since the previous visit is critical for effective management. These consultations often occur annually but may be more frequent based on individual health needs and risk factors.
Summary of Medical History
A comprehensive summary of medical history is essential for effective internal medicine follow-up consultations. Key elements include chronic conditions, such as hypertension, diabetes, or hyperlipidemia, with relevant dates of diagnosis and treatment plans. Previous surgical history, including appendectomy or joint replacements, should be documented to provide context. Medication lists must include dosages and adherence levels, particularly for anti-hypertensives or statins. Allergies to medications, like penicillin or sulfa drugs, need highlighting to prevent adverse reactions. Family medical history can reveal hereditary risks, such as a parent's history of heart disease or cancer, contributing vital information for preventive strategies. Recent laboratory results, such as HbA1c levels for diabetes management or lipid panels for cholesterol assessment, should be reviewed to inform ongoing treatment. Social history, including smoking status, alcohol consumption, and exercise habits, is crucial for tailoring lifestyle recommendations. Documenting patient-reported symptoms, such as fatigue or chest pain, offers insight into current health status, ensuring a holistic approach to care.
List of Current Medications
During a follow-up consultation for internal medicine, maintaining an organized list of current medications is crucial for effective patient management. Essential components of this list include prescription medications (e.g., atorvastatin for cholesterol management), over-the-counter drugs (such as ibuprofen for pain relief), supplements (like vitamin D), and any herbal remedies (e.g., ginkgo biloba for cognitive support). The dosage (e.g., 20 mg once daily), frequency (e.g., twice daily), and administration routes (oral or topical) must be specified for clarity. Including relevant details such as the prescribing physician's name, the date medications were initiated, and reasons for their use enhances the context for the healthcare provider during the assessment. Identifying adverse effects or interactions between medications, such as increased bleeding risk with blood thinners and certain supplements, is essential to ensure patient safety and optimize therapy outcomes.
Instructions for Follow-Up Care
Follow-up care after a visit to an internal medicine specialist is crucial for optimal health management. Patients receiving post-consultation instructions should monitor vital signs, including blood pressure readings ideally between 90/60 mmHg and 120/80 mmHg. Adhering to prescribed medication schedules, such as antihypertensive or cholesterol-lowering drugs, should take precedence. Attending scheduled laboratory tests to evaluate liver function (ALT and AST levels) can help track treatment efficacy. Implementing lifestyle changes, including a balanced diet rich in fruits, vegetables, and whole grains, promotes cardiovascular health. Regular exercise, aiming for at least 150 minutes of moderate activity weekly, is also recommended. Follow-up appointments should be scheduled within 4 to 6 weeks to assess progress and adjust treatment plans if necessary. Engaging in open communication with healthcare providers regarding any new symptoms or concerns greatly contributes to effective patient care.
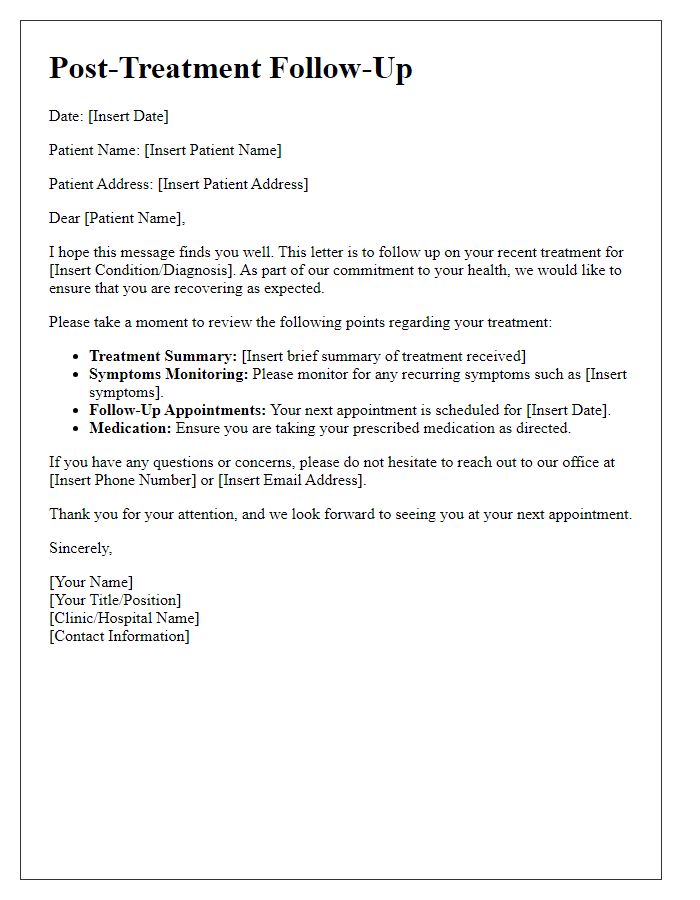
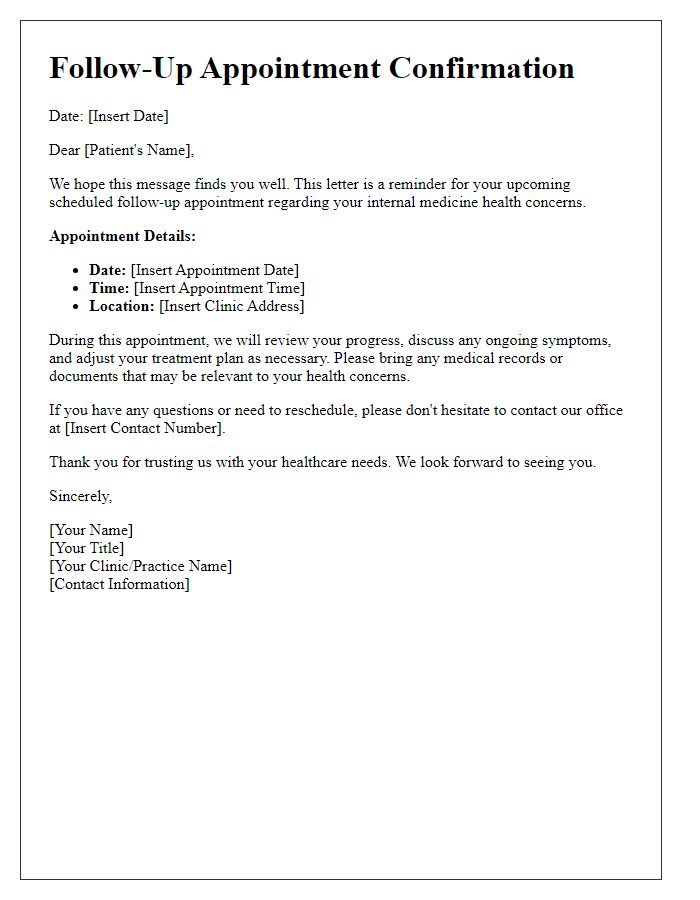
Letter Template For Internal Medicine Follow-Up Consultation Samples
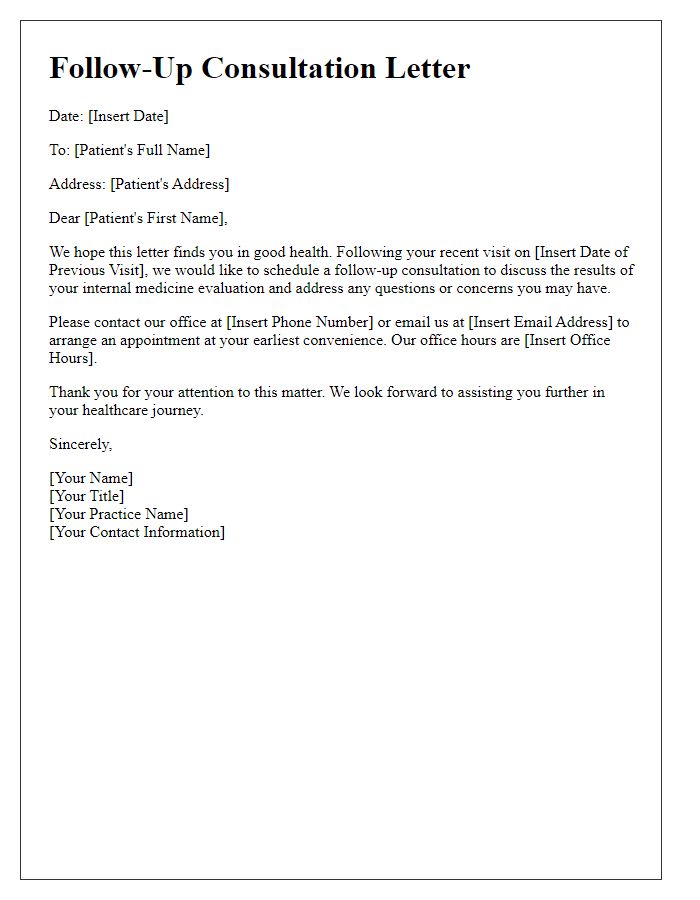
Letter template of follow-up consultation for internal medicine evaluation
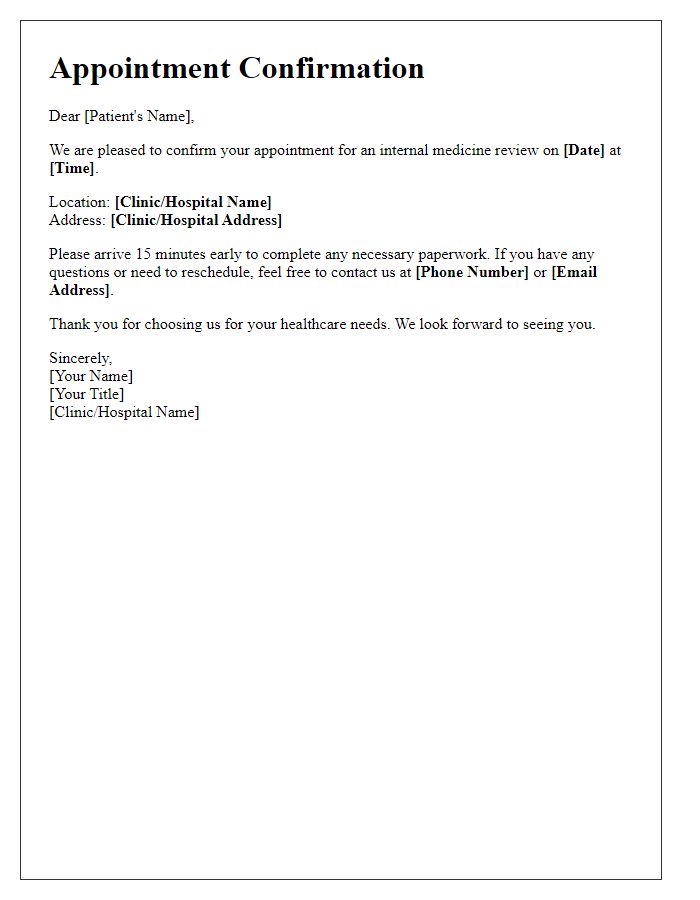
Letter template of follow-up visit for chronic conditions in internal medicine

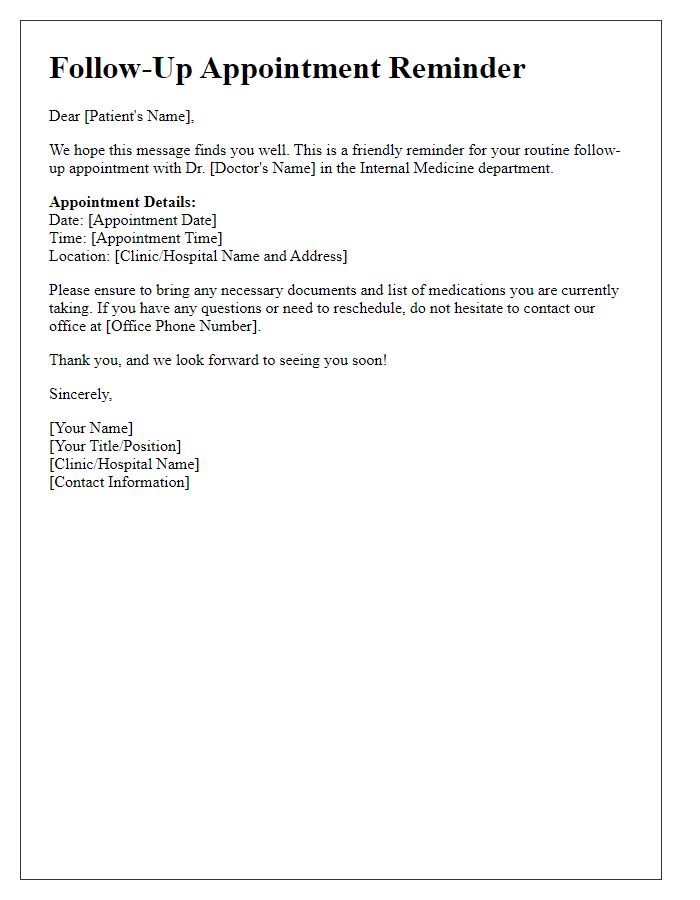
Letter template of routine follow-up appointment for internal medicine patients


Comments