When it comes to healthcare, ensuring that patients are informed and comfortable with their treatment plans is essential. A well-crafted letter of consent for treatment modifications not only protects the rights of patients but also fosters trust between them and their medical providers. This document serves as a critical communication tool, outlining the specifics of the proposed changes and obtaining the necessary agreement. Ready to learn more about how to create an effective consent letter? Let's dive in!
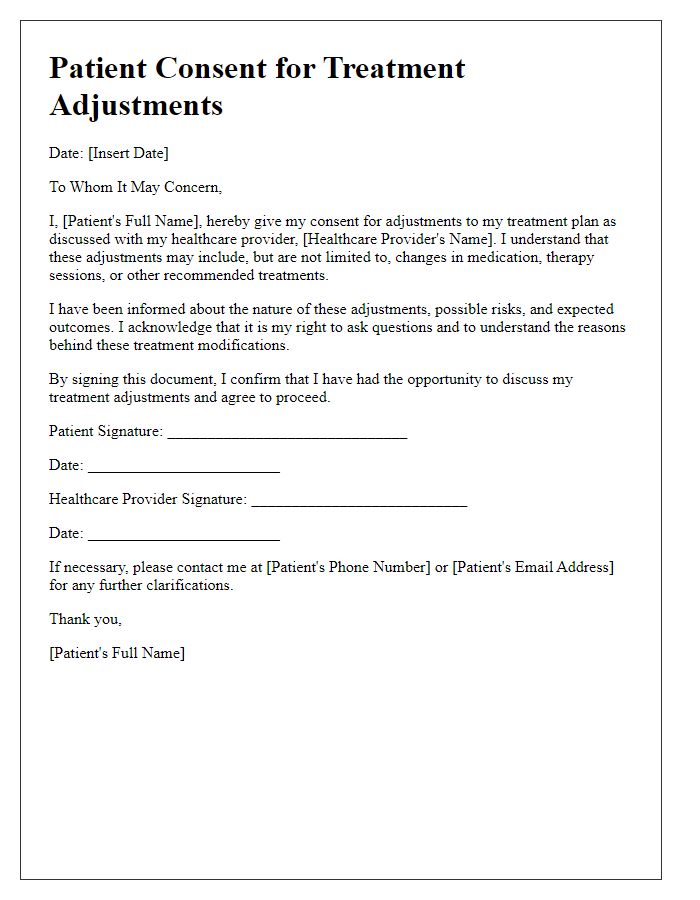
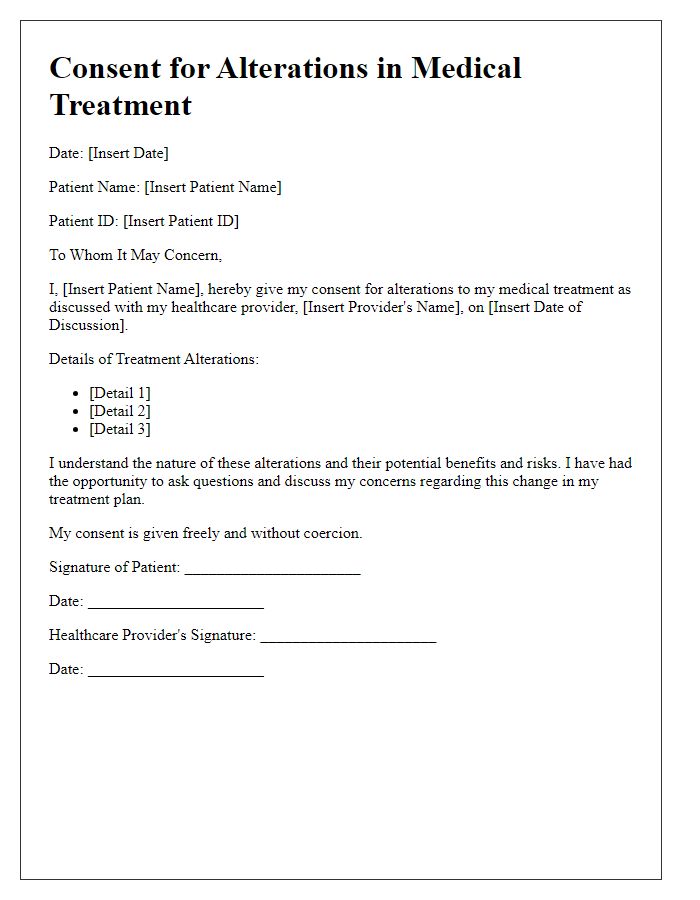
Patient Information
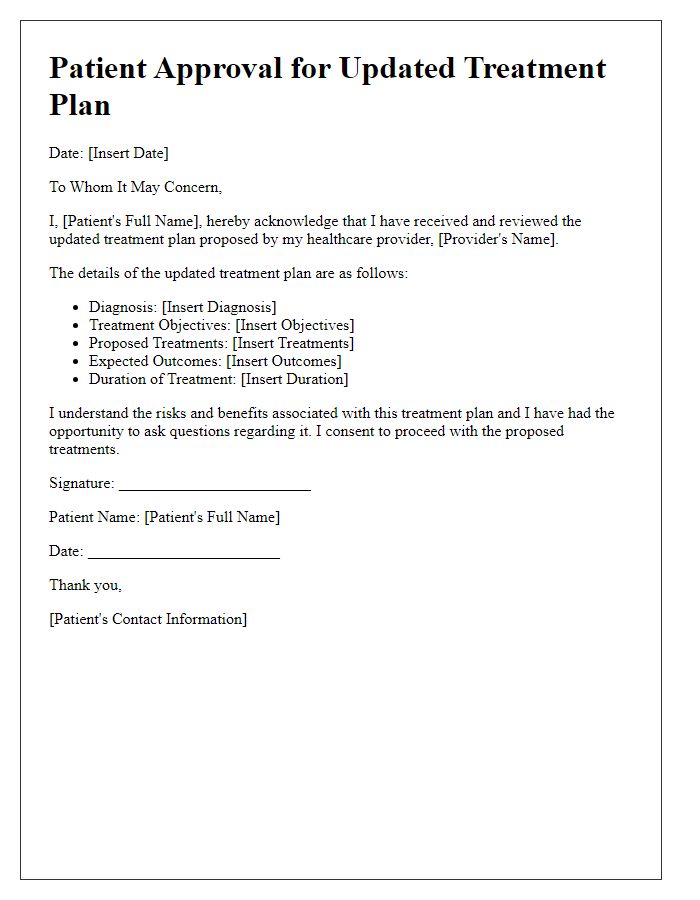
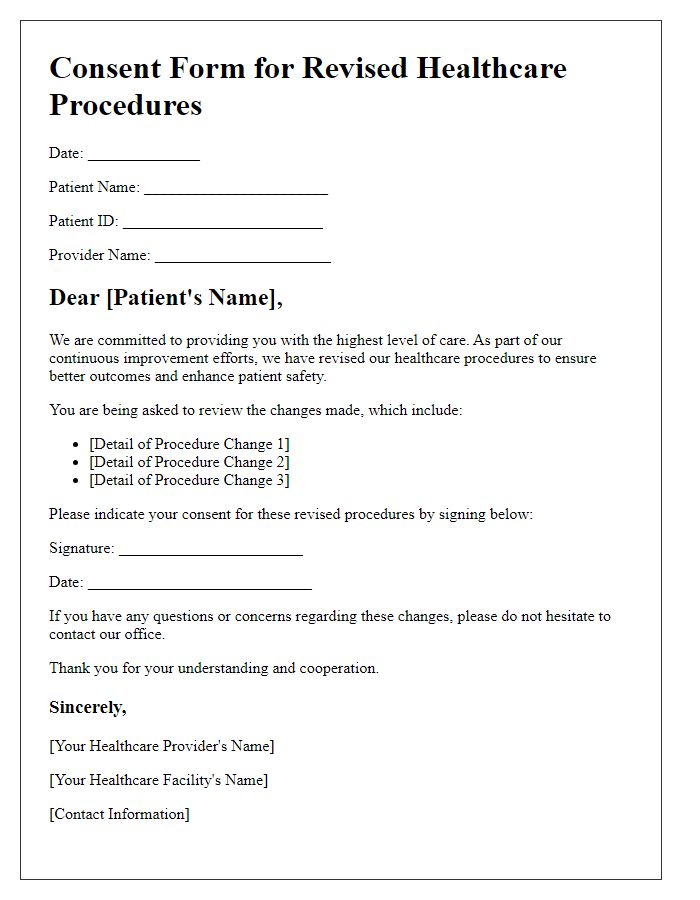
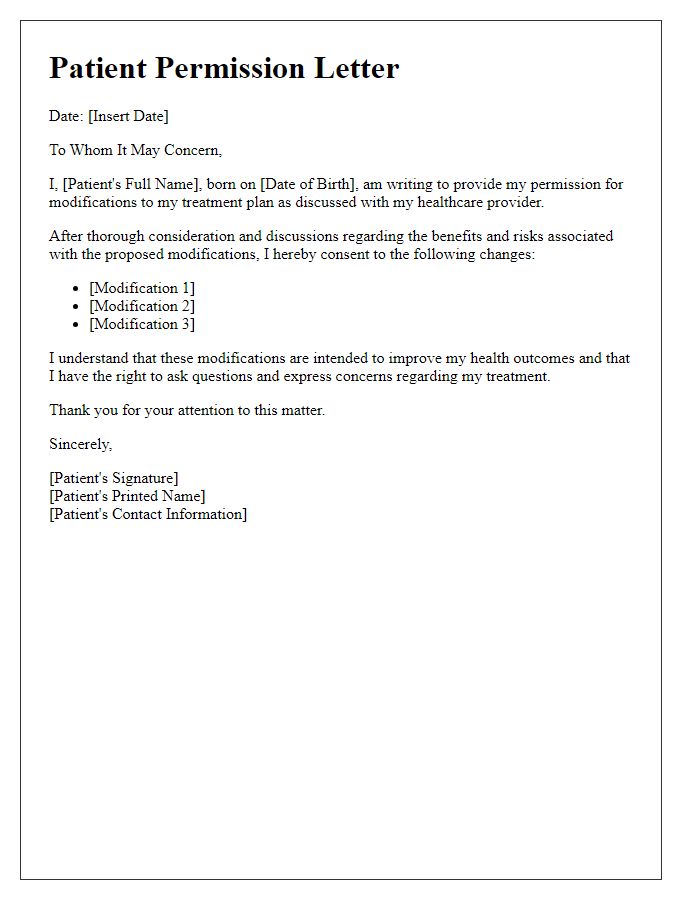
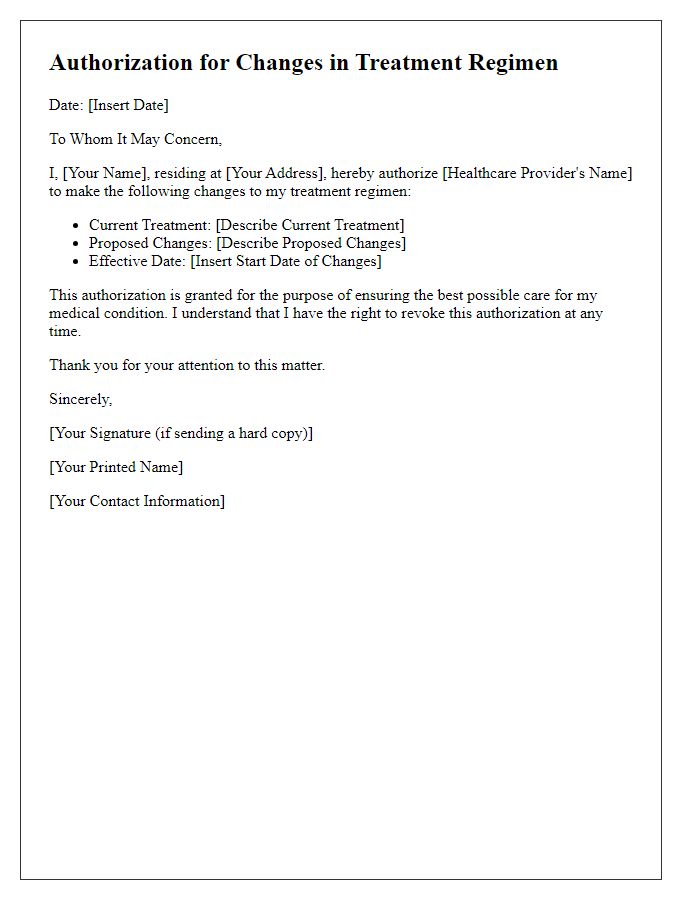
Patient consent for treatment modifications is a crucial document that ensures the patient understands and agrees to changes in their medical care. This consent form typically includes essential patient information such as the patient's full name, date of birth (e.g., January 15, 1980), and medical record number (e.g., MRN 123456789). Furthermore, details about the specific treatment modifications being proposed (e.g., dosage changes, new medication introductions) should be clearly outlined, alongside explanations of the potential benefits and risks involved. Additional notes on the healthcare provider, including their name (e.g., Dr. John Smith) and contact information, are important components, as is the date of consent (e.g., March 1, 2023), to establish a timeline of agreement. Other entities that may be involved, such as a family member or healthcare proxy, should also be noted to ensure that the patient's wishes are respected throughout their treatment journey.
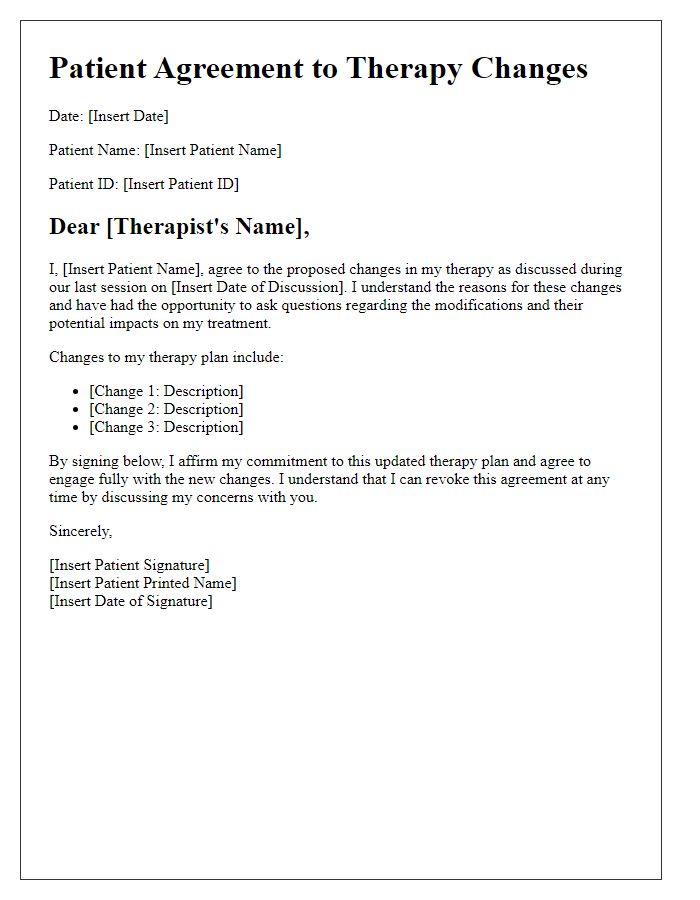
Treatment Modification Details
A patient consent form for treatment modifications details the specific adjustments made to a patient's healthcare regimen, ensuring clarity and understanding of the changes. For instance, dosage alterations may pertain to medications like Metformin for diabetes management, where the physician may recommend reducing the dosage from 500 mg to 250 mg. The modification could be due to blood test results indicating improved glucose levels, measured by HbA1c percentages that have fallen below the target range. Additionally, the consent form should address potential risks associated with these changes, such as the chance of hypoglycemia. Moreover, the patient should be informed about follow-up appointments at the healthcare facility, for example, the diabetes center located in City Hospital, scheduled every three months to monitor adaptation to the altered treatment plan. Clear acknowledgment of understanding these modifications protects both patient and provider.
Risks and Benefits Explanation
Patient consent to treatment modification involves a thorough understanding of associated risks and benefits. When considering surgical procedures such as a laparoscopic cholecystectomy (gallbladder removal), potential risks may include infection, bleeding, and adverse reactions to anesthesia. Benefits often include reduced recovery time, minimal scarring, and less postoperative pain compared to traditional open surgery. Healthcare providers must clearly communicate these factors to patients, ensuring they comprehend the implications of their choices. This process often includes reviewing the patient's medical history, current medications, and any pre-existing conditions that may influence treatment outcomes, ultimately leading to informed and voluntary decision-making regarding their health care.
Voluntary Consent Statement
Informed consent is essential to ensure patients understand the treatment modifications being proposed for their healthcare. A patient voluntarily consents to treatment modifications when they are adequately informed about the potential benefits, risks, and alternatives. This process typically involves discussions with healthcare professionals, including doctors and nurses, at medical facilities such as hospitals or outpatient clinics. Patients must be made aware of specific treatment details, including medications, procedures, and testing involved. For instance, the modification of medication dosages or the introduction of new therapies should be clearly explained. The consent form should include details about the patient's rights, emphasizing their ability to withdraw consent at any time. Moreover, understanding how these modifications may impact the patient's overall health journey is crucial for informed decision-making.
Signature and Date
Informed consent for treatment modifications involves the patient acknowledging their understanding of changes to their medical plan. Key elements include the specific modifications being proposed, potential risks associated with these changes, benefits of the new treatment approach, and alternative options available. The patient's signature and date serve as formal acknowledgment that they have received, read, and understood the information presented regarding their treatment options and the implications of the modifications, ensuring compliance with legal and ethical standards in healthcare settings.


Comments