Are you navigating the world of durable medical equipment (DME) requests and feeling a bit overwhelmed? You're not alone! Many find the process daunting, but with the right guidance, it can be a breeze. Let's dive into essential tips and templates to simplify your DME request, ensuring you get what you need without the hassleâread on to discover more!

Patient's Personal Information
Durable Medical Equipment (DME) requests require specific patient information for processing. Essential personal information includes the patient's full name, date of birth (typically in MM/DD/YYYY format), and primary diagnosis, which helps justify the need for equipment such as wheelchairs or hospital beds. Insurance details, including policy number and provider information, facilitate coverage verification. Contact information, such as phone number and address, is crucial for communication purposes. Additional notes may encompass medical history relevant to the equipment requested, ensuring a comprehensive view of the patient's needs. Clear documentation of equipment specifications, including model numbers and quantity, streamlines the approval process.
Medical Necessity Statement
Durable medical equipment (DME) plays a crucial role in patient care, especially for individuals requiring continuous support for mobility and health management. Medical professionals often provide a Medical Necessity Statement, detailing why specific items, such as wheelchairs or hospital beds, are essential for patient rehabilitation and comfort. For instance, a powered wheelchair might be prescribed for a patient diagnosed with Multiple Sclerosis, allowing for enhanced mobility and independence. Documented evidence may include physician recommendations, including diagnosis codes like G35 for Multiple Sclerosis, and proof of prior therapy attempts. Such statements aim to justify the equipment's necessity to insurance providers, ensuring patients access vital resources for improved quality of life and recovery outcomes.
Prescribing Physician's Information
Durable medical equipment (DME) requests require detailed information about the prescribing physician to ensure proper authorization and coverage. Essential details include the physician's full name, medical qualification (e.g., Doctor of Medicine, Doctor of Osteopathy), National Provider Identifier (NPI) number, and contact information (phone number and office address). Information about the practice or facility, including tax identification number (TIN), and any relevant specialty certifications (e.g., geriatric medicine, rehabilitation medicine) is crucial for the legitimacy of the request. Additionally, documentation of the patient's medical condition, treatment history, and the specific DME needed (such as wheelchairs, oxygen therapy equipment, or prosthetics) will support the necessity for the prescribed equipment.
Detailed Equipment Description
Durable medical equipment (DME) encompasses a wide range of essential items designed to assist individuals with medical needs. Examples include wheelchairs (both manual and powered), which provide mobility for patients with limited physical capabilities, and hospital beds adjustable to enhance comfort and accessibility for users with prolonged medical conditions. Essential components may include pressure-relief mattresses that prevent bedsores, as well as oxygen concentrators delivering medical-grade oxygen to patients with respiratory illnesses such as chronic obstructive pulmonary disease (COPD). Additionally, nebulizers are critical for effectively administering medication in aerosol form to patients with asthma or other chronic lung diseases. The correct selection of DME is vital for enhancing the quality of life for individuals with mobility challenges or ongoing health issues.
Insurance and Payment Information
Durable medical equipment (DME) requests often require specific insurance types, such as Medicare or Medicaid, to ensure coverage for necessary items like wheelchairs, oxygen tanks, or CPAP machines. Detailed billing codes (HCPCS codes) must be provided to process claims accurately. Insurance deductibles and co-pays can vary significantly, impacting the total out-of-pocket expenses for patients requiring assistance. Prior authorization may be necessary for certain equipment, such as hospital beds or mobility aids, depending on the insurance provider's policies. Documentation of medical necessity from a healthcare provider is typically required to support the claim and demonstrate that the equipment is essential for the patient's well-being. Understanding the local laws and insurance requirements for DME is crucial for both providers and patients to navigate the approval and payment processes efficiently.
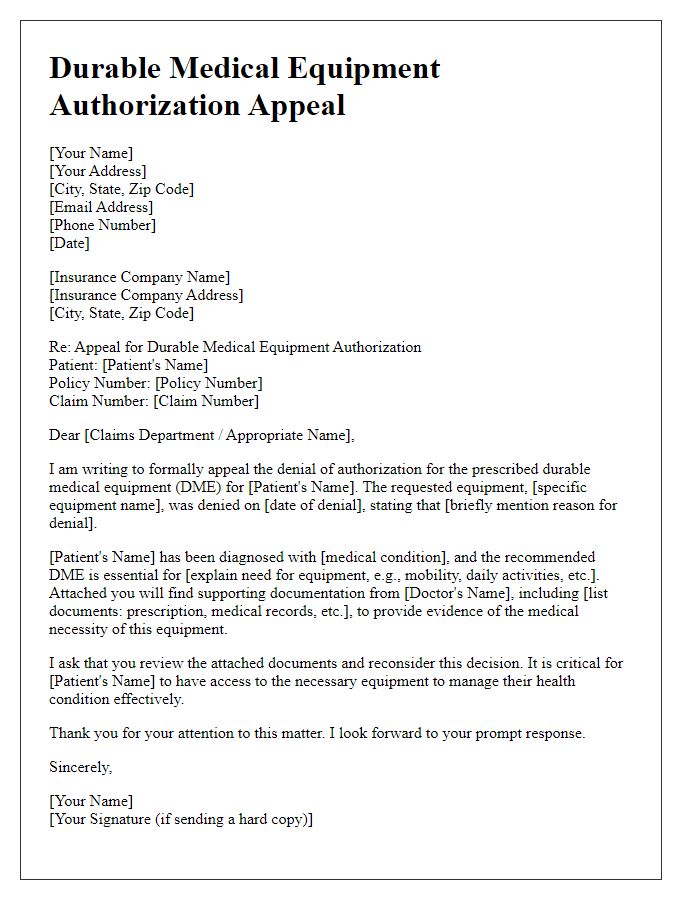
Letter Template For Durable Medical Equipment Request Samples
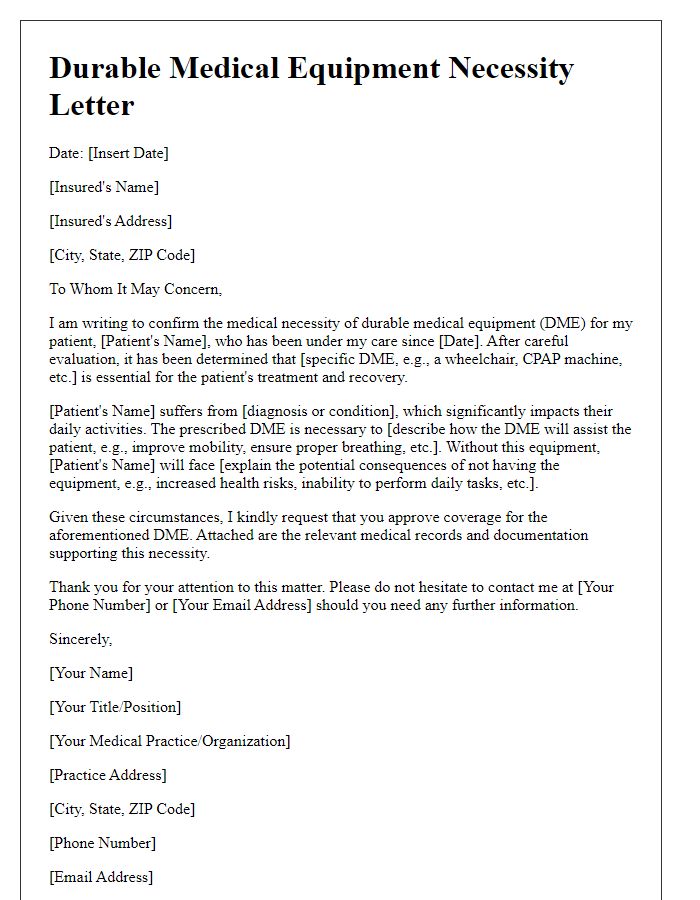
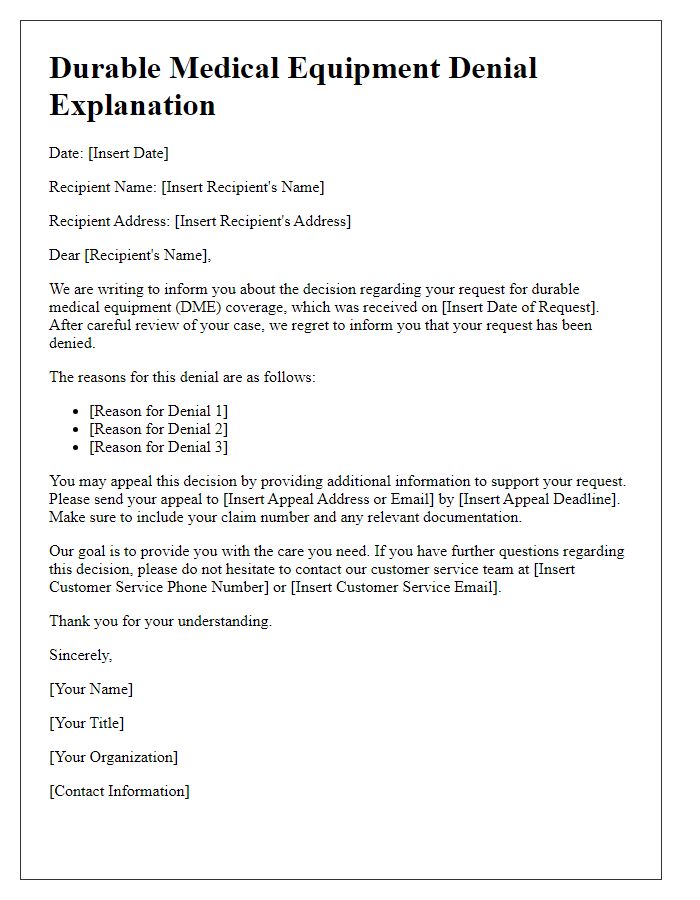
Letter template of durable medical equipment necessity for insurance claims.
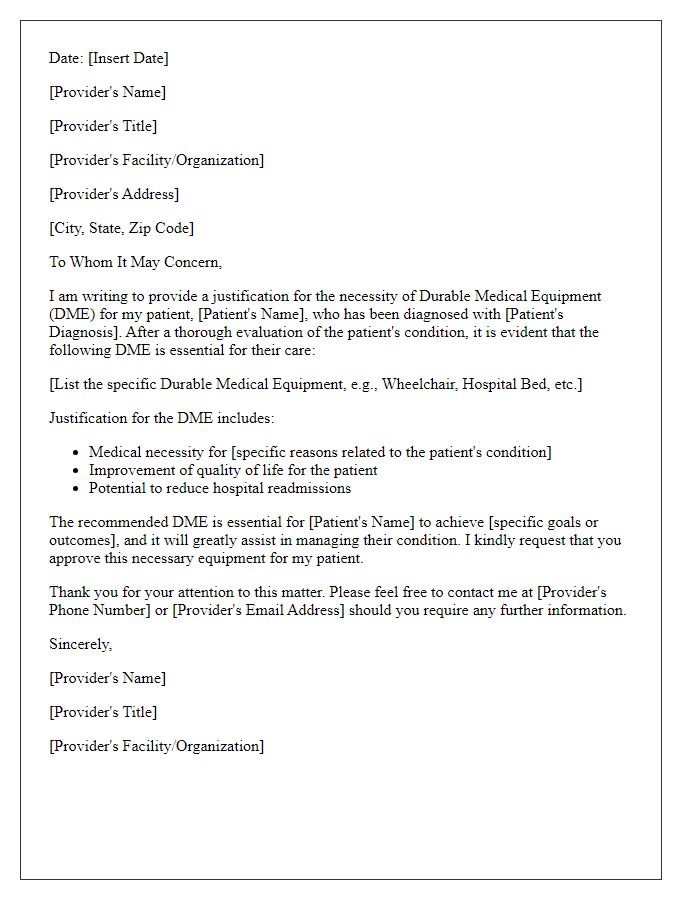
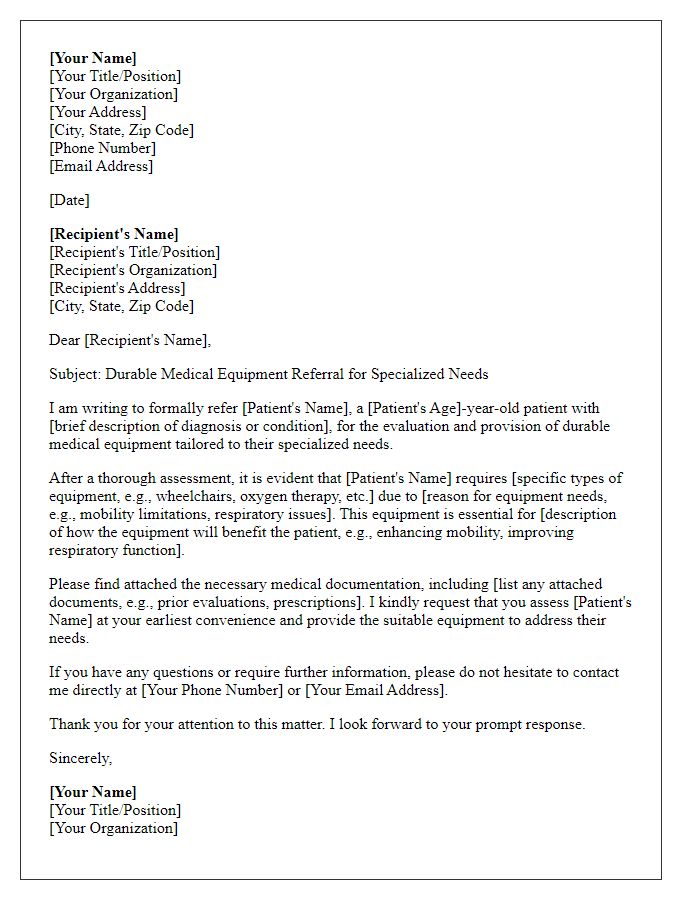
Letter template of durable medical equipment justification for healthcare providers.
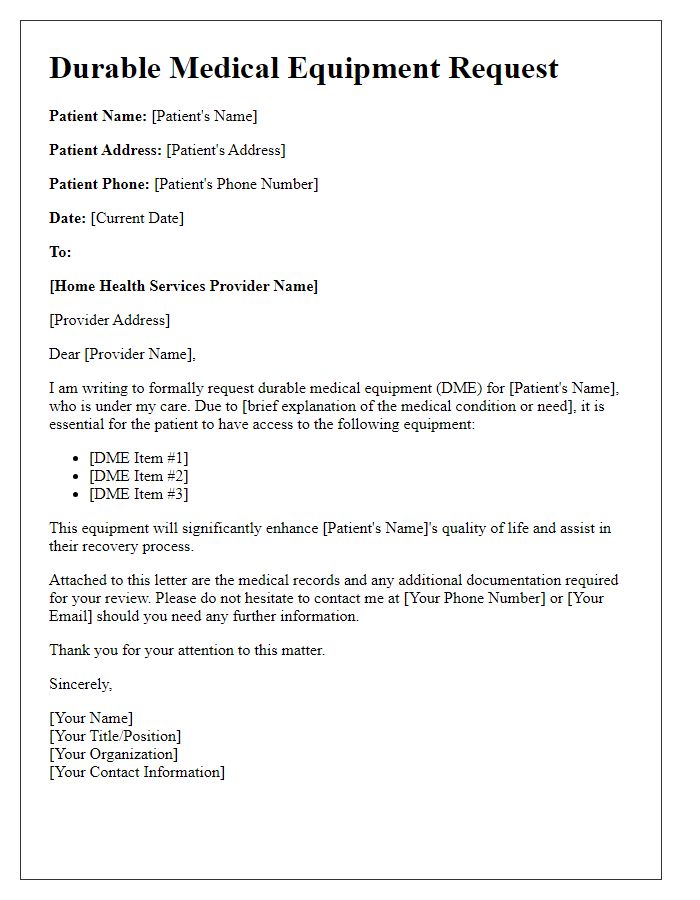
Letter template of durable medical equipment request for home health services.


Comments