Managing your glucose levels is crucial for your overall health, and having a solid monitoring plan can make all the difference. In this article, we'll explore the essential components of an effective glucose monitoring strategy, tailored just for you. From setting realistic goals to recognizing the best times to check your levels, we've got you covered with practical tips. So, grab a cup of tea and dive in as we unravel the details of creating your personalized glucose monitoring plan!
Personalized glucose target ranges
Personalized glucose monitoring plans for diabetic patients are essential for effective management of blood sugar levels. These plans typically include individualized glucose target ranges that vary based on factors like age, weight, and activity level. For instance, the American Diabetes Association recommends fasting blood glucose levels between 80-130 mg/dL for adults under 65 years old, and between 90-150 mg/dL for older adults, highlighting the importance of tailored goals. Key metrics such as postprandial (after meal) glucose should ideally be under 180 mg/dL at one to two hours after eating. Continuous glucose monitoring (CGM) systems, like the Dexcom G6, provide real-time data and enable patients to adjust their daily routines accordingly. Regular consultations with healthcare providers ensure that the glucose targets are reassessed as needed, considering changes in lifestyle or health conditions.
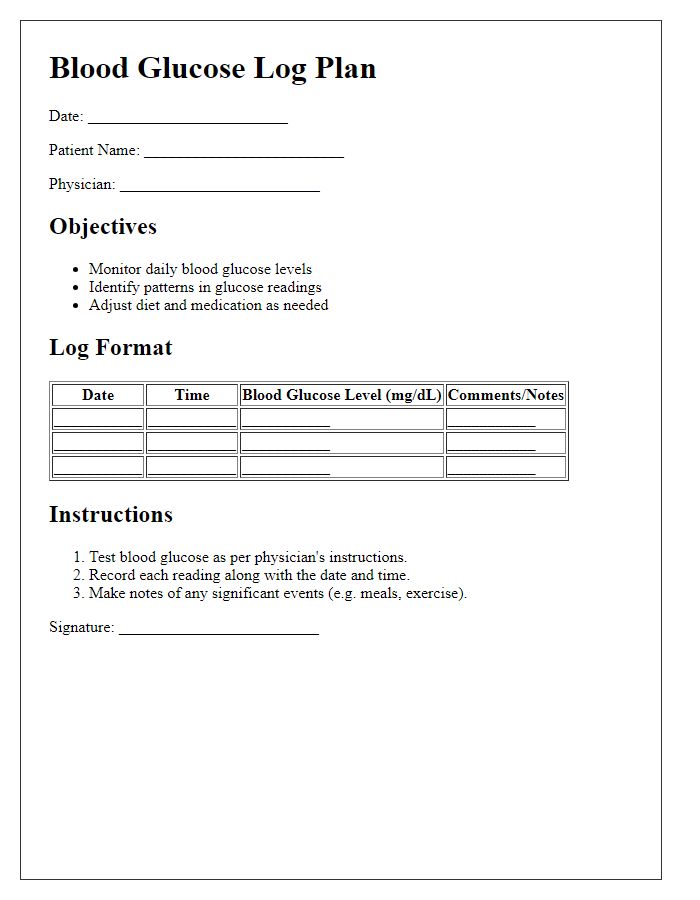
Frequency of blood glucose testing
Regular blood glucose testing is crucial for effective diabetes management, typically recommended multiple times daily for optimal control. Patients should conduct tests before meals, two hours post-meal, and at bedtime to monitor fluctuations in glucose levels. The American Diabetes Association suggests maintaining a target range of 70 to 130 mg/dL before meals and less than 180 mg/dL after meals. Continuous monitoring devices, such as the Dexcom G6, offer a comprehensive overview, allowing for trend analysis over time. Patients must log their results, noting any symptoms or dietary adjustments, to discuss with healthcare providers during follow-up visits. Timely adjustments in medication or lifestyle based on these readings can significantly enhance overall health outcomes.
Dietary and exercise recommendations
A comprehensive glucose monitoring plan emphasizes the importance of dietary choices and physical activity for managing diabetes effectively. For optimal glucose control, individuals should aim for a balanced diet rich in whole foods, including fresh vegetables, fruits, whole grains, and lean proteins, while limiting processed foods high in sugars and unhealthy fats. The American Diabetes Association recommends consistent meal timing and portion control, typically involving three main meals and two snacks, with an emphasis on fiber intake to stabilize blood sugar levels. Daily exercise is critical, with at least 150 minutes of moderate-intensity aerobic activity per week, such as brisk walking or cycling, to enhance insulin sensitivity and aid weight management. Incorporation of resistance training twice a week supports muscle health, which plays a role in glucose metabolism. Regular monitoring of blood glucose levels is essential to evaluate the effectiveness of dietary and exercise modifications, enabling timely adjustments to the management plan.
Insulin and medication adjustments
A comprehensive patient glucose monitoring plan requires careful tracking of insulin levels and medication adjustments for optimal diabetes management. Regular blood glucose testing, ideally four to six times daily, allows for insight into daily fluctuations in glucose levels. Patients may need to administer rapid-acting insulin, such as Lispro or Aspart, before meals to counteract carbohydrate intake. Monitoring should also incorporate long-acting insulin, like Glargine or Detemir, taken once or twice daily to maintain baseline glucose levels. Adjustments in dosages might be warranted based on meal sizes, activity levels, and stress factors affecting glucose metabolism. Documenting all readings in a glucose diary aids in identifying patterns and potential areas for intervention, enhancing overall health outcomes. Regular consultations with healthcare providers are essential for timely medication adjustments based on monitoring data.
Follow-up and communication schedule
Developing a patient glucose monitoring plan involves establishing a systematic follow-up and communication schedule. Regular monitoring, typically recommended at least three times a week, allows healthcare providers to track blood glucose levels effectively. For example, patients may be instructed to measure their fasting glucose levels daily in the morning (between 7 AM and 9 AM) and additional readings post-meals (one to two hours after eating). Monthly follow-ups with healthcare professionals, including dietitians and endocrinologists, enable assessment and adjustment of dietary plans and medication dosages. Digital communication tools like glucose tracking apps can facilitate real-time sharing of data, enhancing patient engagement. Incorporating specific dates for check-ins, such as every first Monday of the month, ensures continuity in care and motivates adherence to the monitoring plan.
Letter Template For Patient Glucose Monitoring Plan Samples
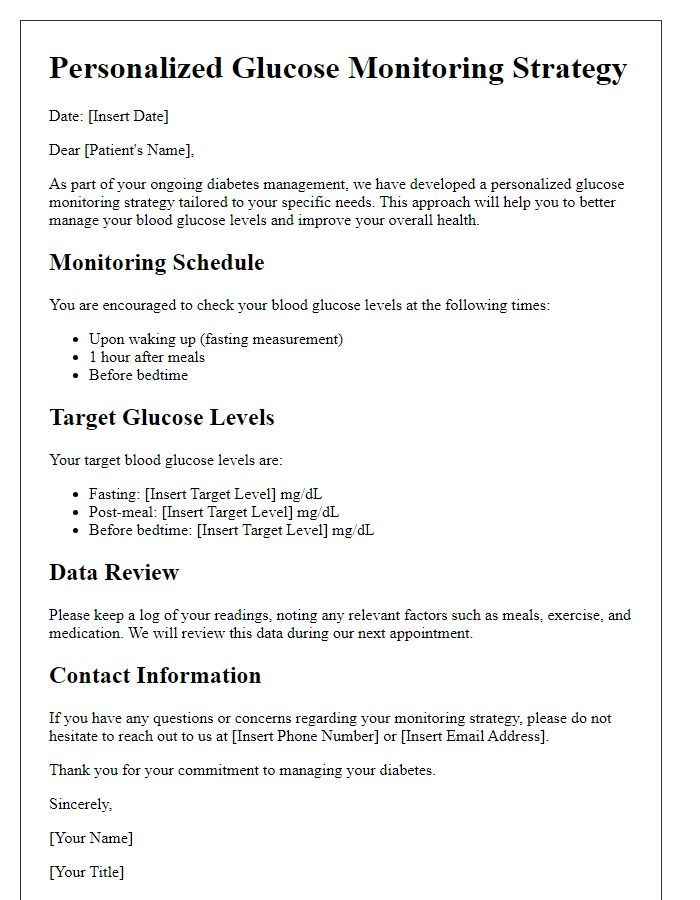
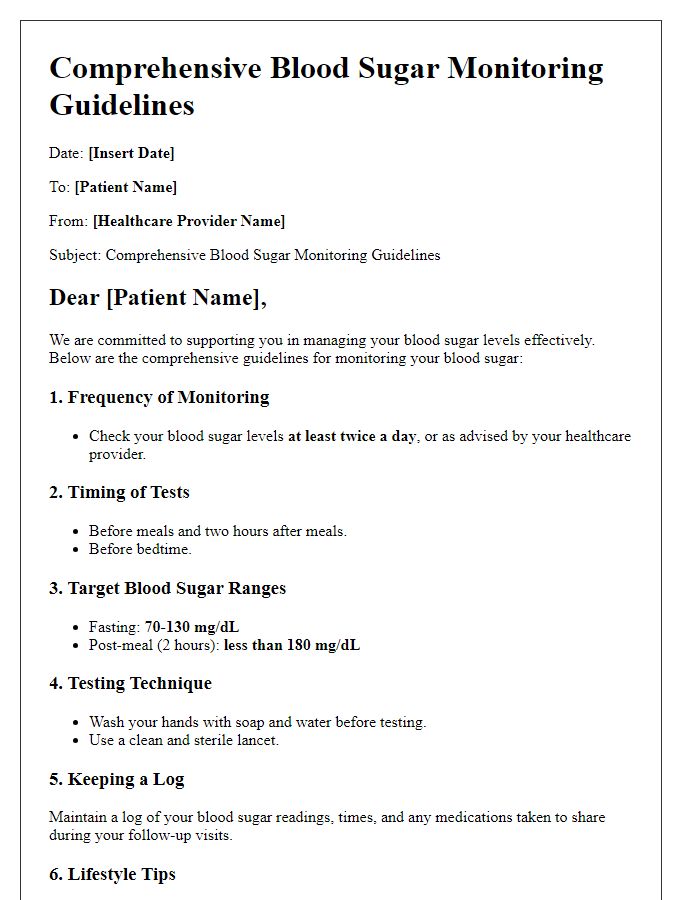
Letter template of personalized glucose monitoring strategy for patients


Comments