Are you struggling with chronic pain and feeling overwhelmed by your condition? You're not alone; many individuals face similar challenges and are seeking answers for better management. In this article, we'll explore essential aspects of chronic pain evaluation, from understanding your symptoms to effective communication with healthcare providers. Join us as we dive deeper into this topic and discover ways to enhance your journey toward relief and recovery.
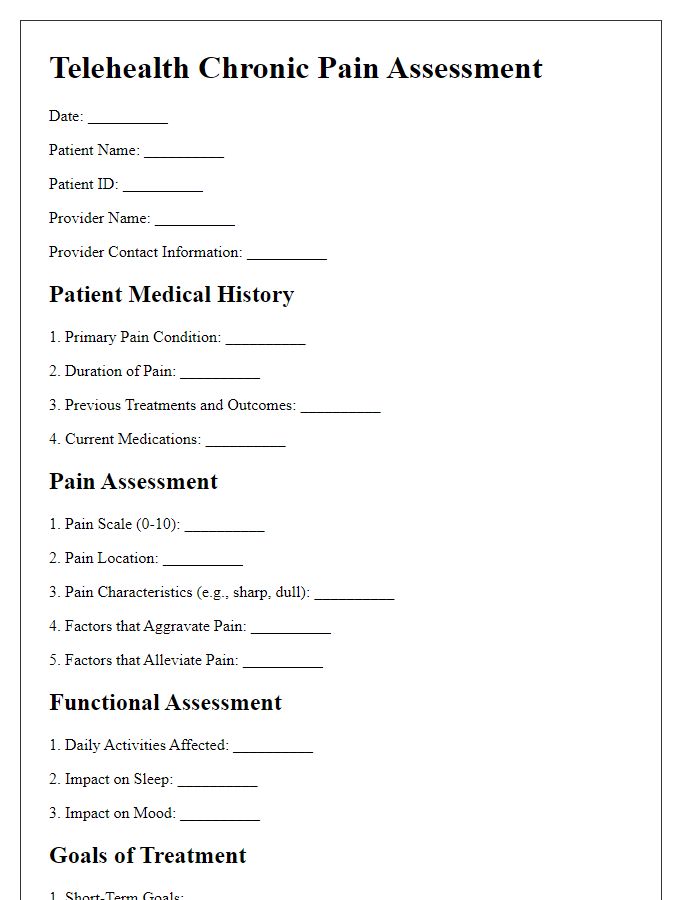
Patient Identification Information
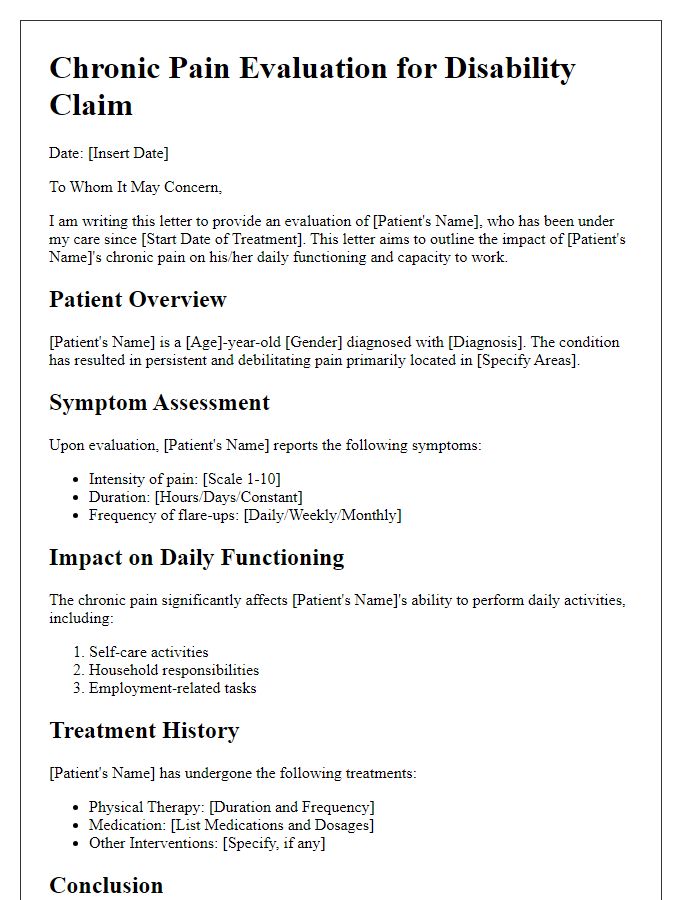
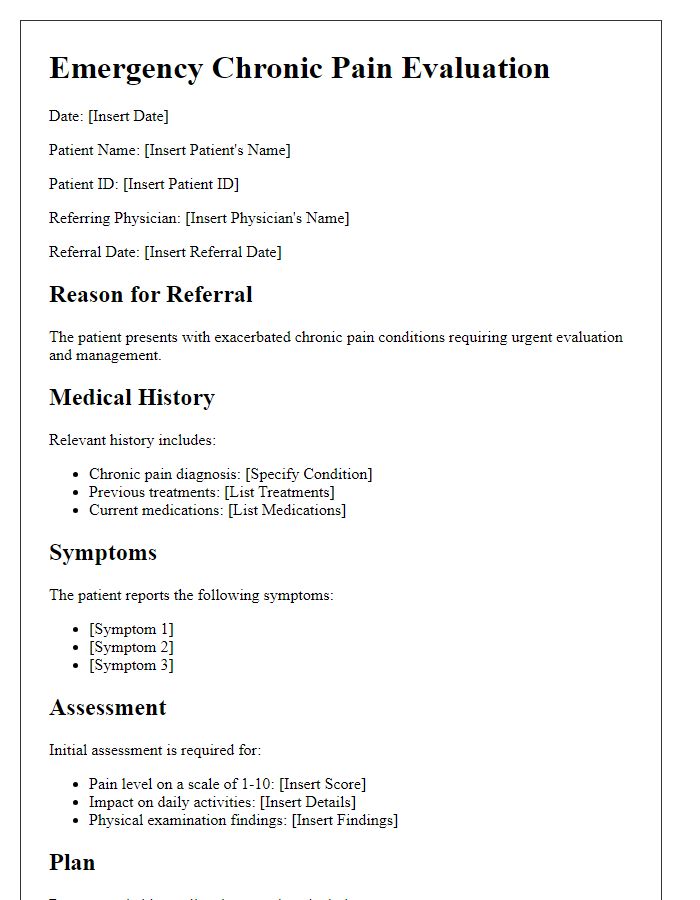
Chronic pain evaluation requires thorough patient identification information to ensure accurate assessment and tailored treatment plans. Essential details include full name, date of birth, and contact information. Medical history should encompass past diagnoses, any previous surgeries (particularly those relevant to pain), and family history of chronic pain conditions, such as fibromyalgia or arthritis. Medication lists are critical, encompassing both prescribed medications and over-the-counter drugs, alongside dosages and frequency of use. Insurance information plays a role in treatment accessibility. Lastly, a detailed pain history documenting onset, duration, intensity (rated on a scale of 1 to 10), and location (specific body parts affected, e.g., lower back or knees) allows healthcare providers to better understand the patient's unique pain experience.
Detailed Pain Description
Chronic pain, often defined as pain persisting beyond three months, can significantly impact daily life and overall well-being. Patients frequently describe their pain with varying intensities on a 0 to 10 scale, where 0 represents no pain and 10 indicates the worst imaginable pain. Common descriptive terms include sharp, dull, throbbing, or burning sensations that can fluctuate in intensity. Locations of pain may vary greatly, often affecting regions such as the lower back, joints, or neck, with specific conditions like fibromyalgia or osteoarthritis contributing to the experience. Additionally, accompanying symptoms such as fatigue, sleep disturbances, and mood changes often co-occur, further complicating the pain experience. Understanding the patterns, triggers, and relief strategies for managing chronic pain is crucial for developing effective treatment plans tailored to individual needs.
Medical History and Current Medications
Chronic pain conditions, such as fibromyalgia or osteoarthritis, often require a detailed exploration of medical history for accurate evaluation. Patients may report persistent discomfort lasting over three months, which can impact quality of life. Detailed accounts of prior injuries, surgeries, or conditions are vital for understanding the underlying causes. Additionally, current medications, including analgesics (e.g., acetaminophen or NSAIDs), antidepressants (e.g., amitriptyline), and any adjuvant therapies, help paint a complete picture of the patient's management plan. It is essential to note dosage, frequency, and any side effects experienced, as this information can guide future treatment options and adjustments. The relationship between these factors contributes to developing a tailored approach to alleviate chronic pain effectively.
Impact on Daily Activities
Chronic pain, often stemming from conditions like fibromyalgia or arthritis, significantly impacts daily activities. Individuals experiencing ongoing pain (lasting over three months) report difficulties in performing routine tasks such as personal hygiene and household chores. Physical limitations may lead to decreased mobility, making it challenging to engage in social interactions or exercise. A study conducted by the American Chronic Pain Association in 2022 indicated that 63% of chronic pain sufferers find it hard to maintain employment due to productivity losses and frequent absenteeism. The psychological aspect of chronic pain often includes anxiety and depression, further hindering the quality of life for individuals. The pervasive nature of chronic pain demands comprehensive evaluation and tailored interventions to enhance overall functioning and well-being.
Treatment and Management Recommendations
Chronic pain conditions require comprehensive assessment and tailored treatment plans for effective management. Clinicians often utilize standardized pain scales (e.g., Numeric Rating Scale from 0 to 10) to quantify patient pain levels. Multidisciplinary approaches may include physical therapy sessions (typically spanning 6 to 12 weeks) focusing on exercises to improve mobility and strength. Pharmacological interventions might involve nonsteroidal anti-inflammatory drugs (NSAIDs) like Ibuprofen or acetaminophen, emphasizing dosages according to the patient's medical history. Psychological support, such as cognitive behavioral therapy (CBT), plays a crucial role in addressing the emotional components of chronic pain. Additionally, lifestyle modifications involving regular physical activity and dietary changes can contribute significantly to pain management strategies. Regular follow-up appointments every 3 to 6 months are essential to reassess treatment efficacy and make necessary adjustments.
Letter Template For Patient Chronic Pain Evaluation Samples
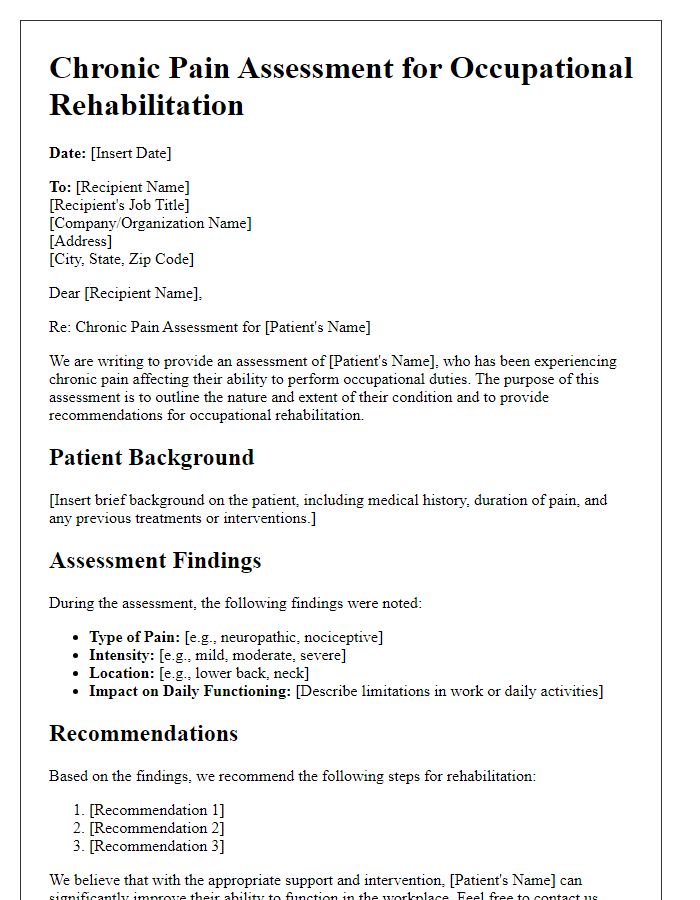
Letter template of chronic pain assessment for occupational rehabilitation.
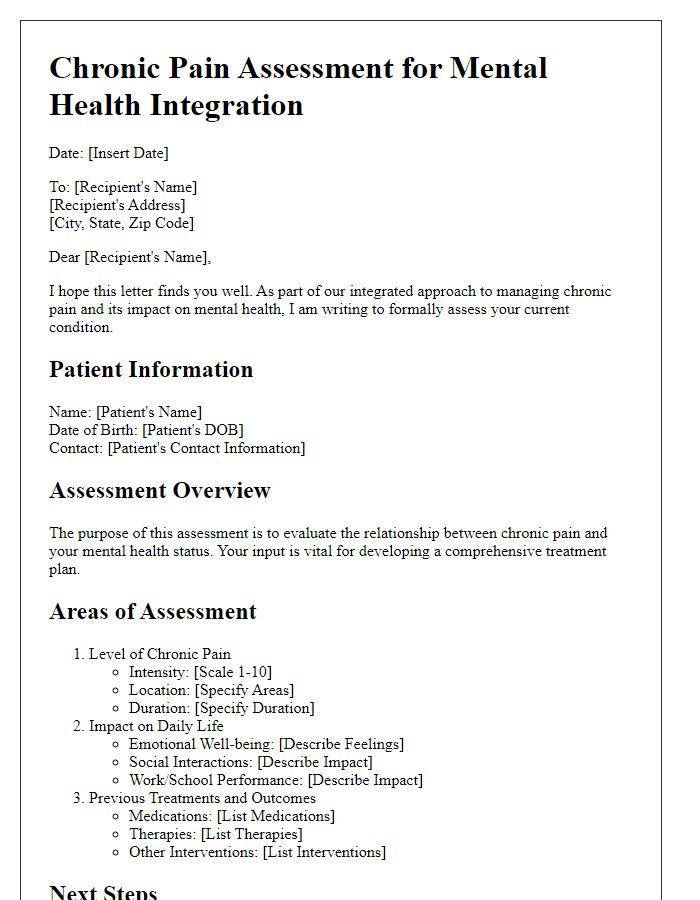
Letter template of chronic pain assessment for mental health integration.



Comments