Are you looking for an effective way to communicate your physical therapy plan to patients? Crafting a comprehensive letter template can make a significant difference in how patients understand their treatment. By providing clear guidance and expectations, you'll enhance their commitment to the recovery process. Dive into this article to discover a practical letter template that you can easily adapt for your needs!
Personal Information
The patient physical therapy plan includes essential personal information, such as the patient's full name, age, and contact details. This data allows healthcare professionals to maintain accurate medical records and establish a personalized treatment approach. The patient's medical history section contains significant details like previous injuries (e.g., fractures or surgeries), chronic conditions (e.g., diabetes or arthritis), and medications currently being taken. Furthermore, the emergency contact information outlines a reliable point of contact, ensuring timely communication in urgent situations. Additionally, insurance information, including provider names and policy numbers, facilitates the billing process, allowing the patient to receive appropriate coverage for physical therapy sessions.
Diagnosis and Assessment
A comprehensive physical therapy plan begins with an accurate diagnosis and thorough assessment of the patient's condition. For instance, a diagnosis such as a torn anterior cruciate ligament (ACL) might necessitate a specific rehabilitation approach tailored to the severity of the injury. The assessment phase includes evaluating range of motion, strength, and functional mobility using standardized tools like the Lysholm Knee Scoring Scale, which provides quantitative data on knee function. Physical therapists may also perform special tests, such as the Lachman test, to confirm ligament integrity. Observations regarding pain levels, typically measured on a scale from 0 to 10, enhance understanding of the patient's challenges. Additionally, the assessment may include an examination of the patient's posture and gait, contributing valuable information that informs tailored interventions and outlines both short-term and long-term goals for effective recovery.
Treatment Goals and Objectives
A comprehensive physical therapy plan must outline treatment goals and objectives to ensure effective recovery for patients experiencing musculoskeletal issues. Short-term goals may include reducing pain levels (targeted reduction by 3-4 points on a 10-point pain scale) and improving range of motion in affected joints (aiming for 10-20 degrees of improvement in flexion or extension). Long-term objectives could focus on regaining functional strength (achieving at least 70% of the patient's pre-injury strength levels) and enhancing endurance (performing daily activities without fatigue, measured through the six-minute walk test). Establishing measurable metrics, such as utilizing a goniometer for joint angles or performance assessments like the Timed Up and Go test, will facilitate tracking progress during sessions, ensuring that the therapeutic interventions are guiding the patient effectively toward recovery.
Treatment Plan Outline
A comprehensive physical therapy treatment plan encompasses an initial assessment, targeted goals, intervention strategies, and follow-up evaluations. The initial assessment involves a thorough examination of the patient's condition, encompassing mobility range, pain levels, and functional limitations, often documented through standardized tools such as the Numeric Pain Rating Scale (0-10) or the Oswestry Disability Index (ODI). Targeted goals are typically SMART (Specific, Measurable, Achievable, Relevant, Time-bound), focusing on specific outcomes such as achieving 80% mobility within six weeks or reducing pain levels by three points on the Numeric Pain Rating Scale. Intervention strategies may include modalities like ultrasound therapy for inflammation reduction, strengthening exercises using resistance bands, and manual therapy techniques to improve joint range of motion in areas such as the lumbar spine or shoulder. Follow-up evaluations, scheduled at intervals (e.g., every two weeks), assess progress towards goals, allowing for modifications in the treatment plan to ensure optimal recovery.
Progress Monitoring and Follow-Up
A physical therapy plan focusing on progress monitoring requires a comprehensive approach to evaluate patient milestones and establish follow-up strategies. Consistent assessments should occur during weekly sessions to track improvements in mobility, strength, and pain levels, utilizing standardized tests such as the Oswestry Disability Index or the Visual Analog Scale (VAS). Detailed notes on range of motion measurements can pinpoint specific joint capabilities, while strength assessments using resistive bands or weights (e.g., five-pound dumbbells) provide clear indicators of physical progression. Follow-up appointments, typically scheduled every four to six weeks, will allow therapists to adjust treatment protocols based on patient feedback and progress. Documentation of each session should reflect therapeutic interventions, patient adherence to home exercise regimens, and adaptations for any reported discomfort. Engaging with patients about their recovery goals fosters motivation and ensures they remain informed about their progress.
Letter Template For Patient Physical Therapy Plan Samples
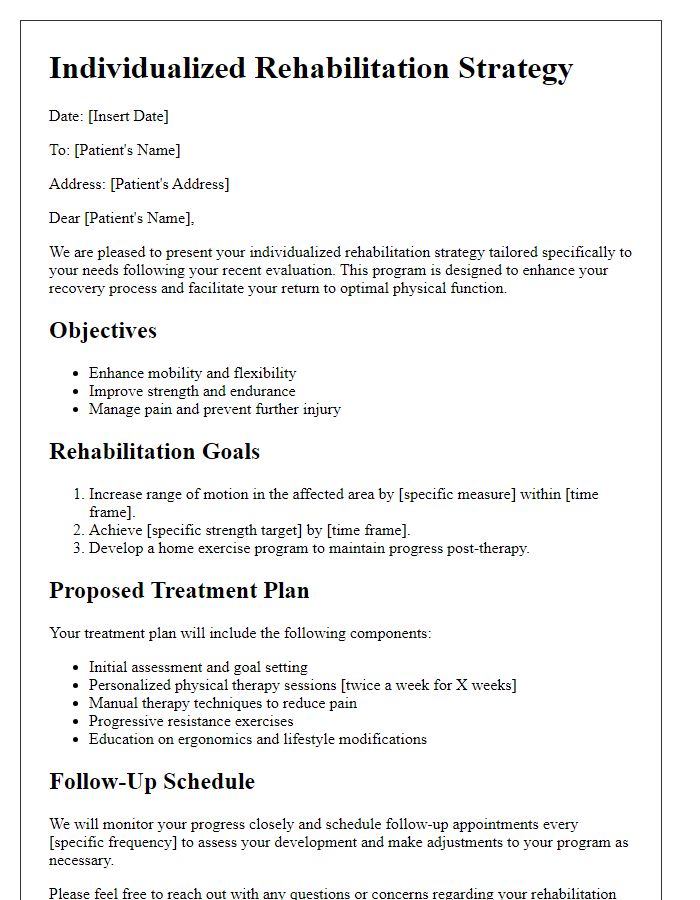
Letter template of individualized rehabilitation strategy for physical therapy.
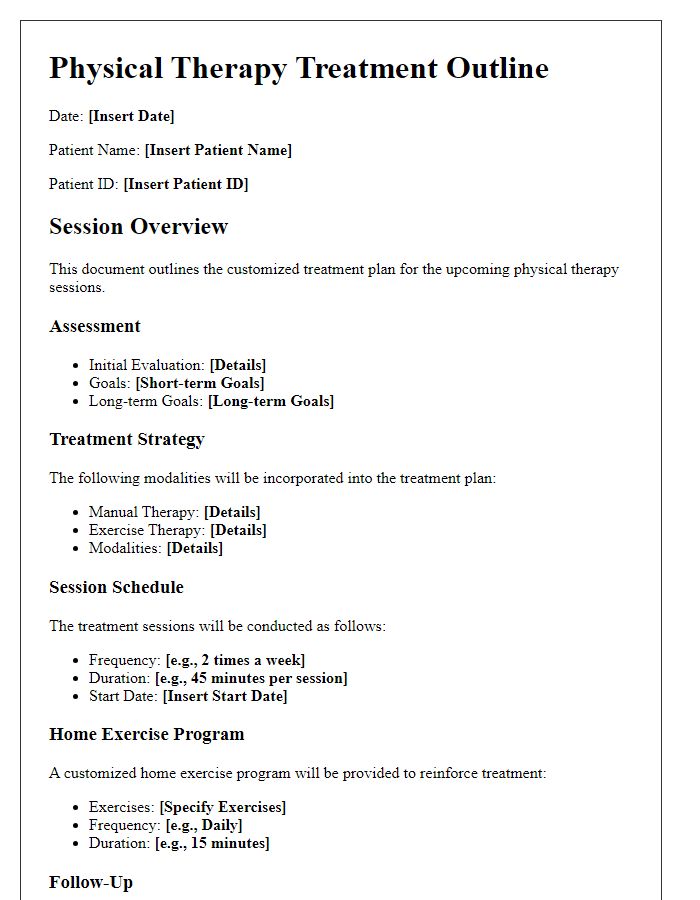
Letter template of customized treatment outline for physical therapy sessions.
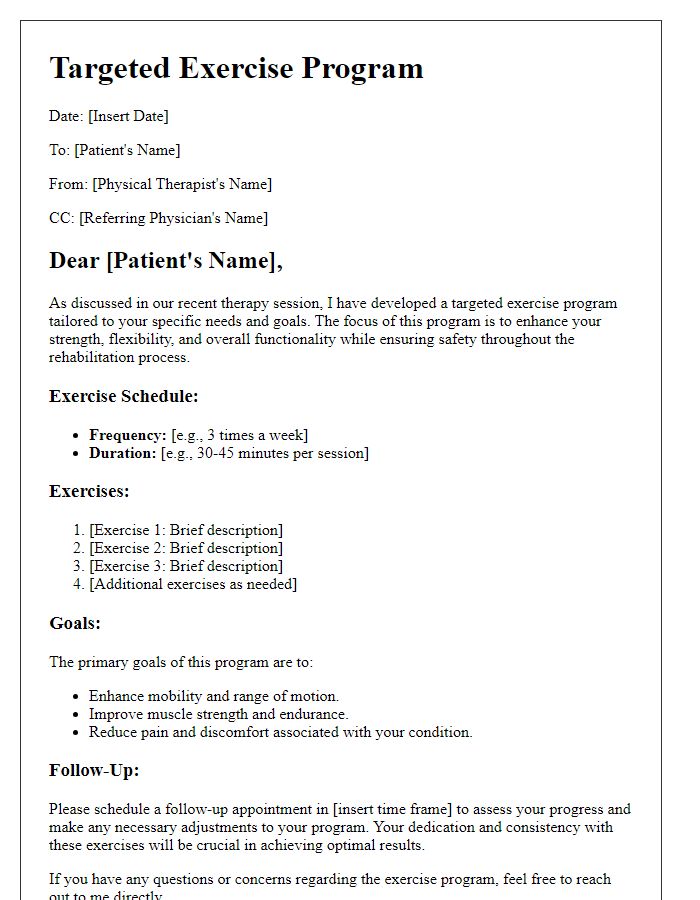
Letter template of targeted exercise program for patient physical therapy.
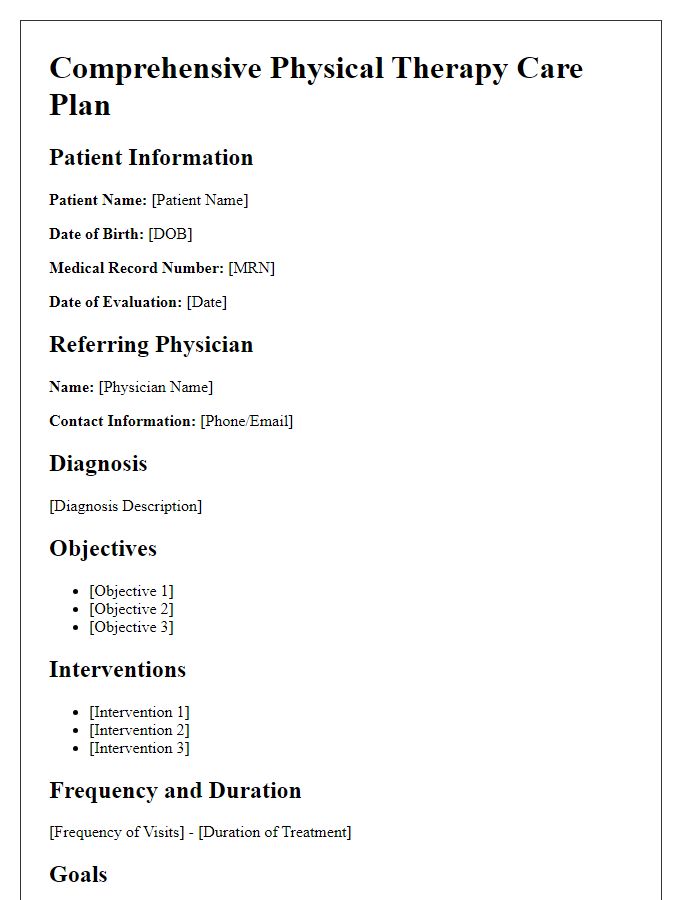
Letter template of comprehensive physical therapy care plan for patients.
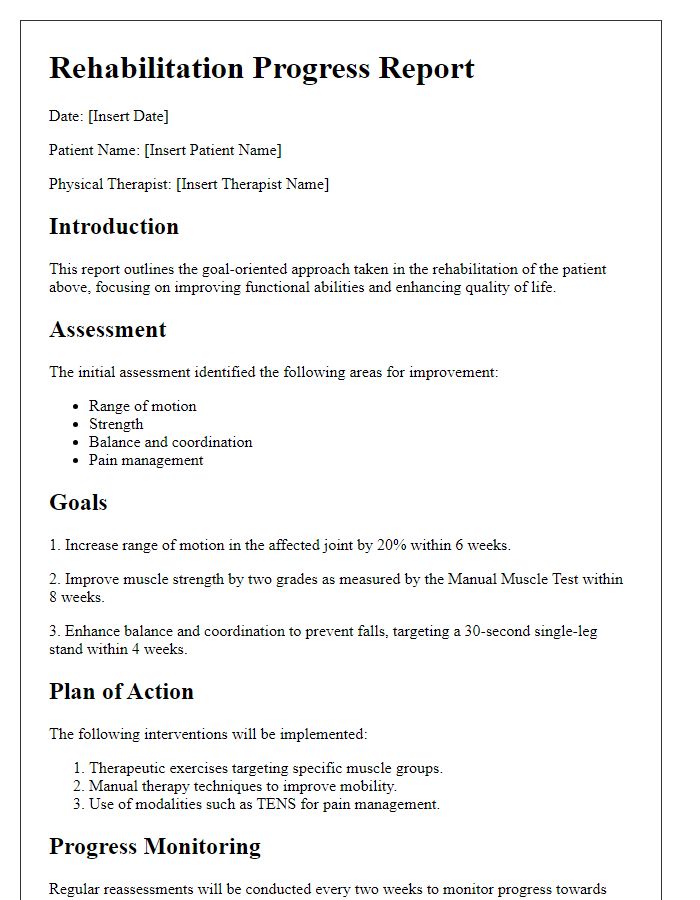
Letter template of goal-oriented physical therapy approach for rehabilitation.
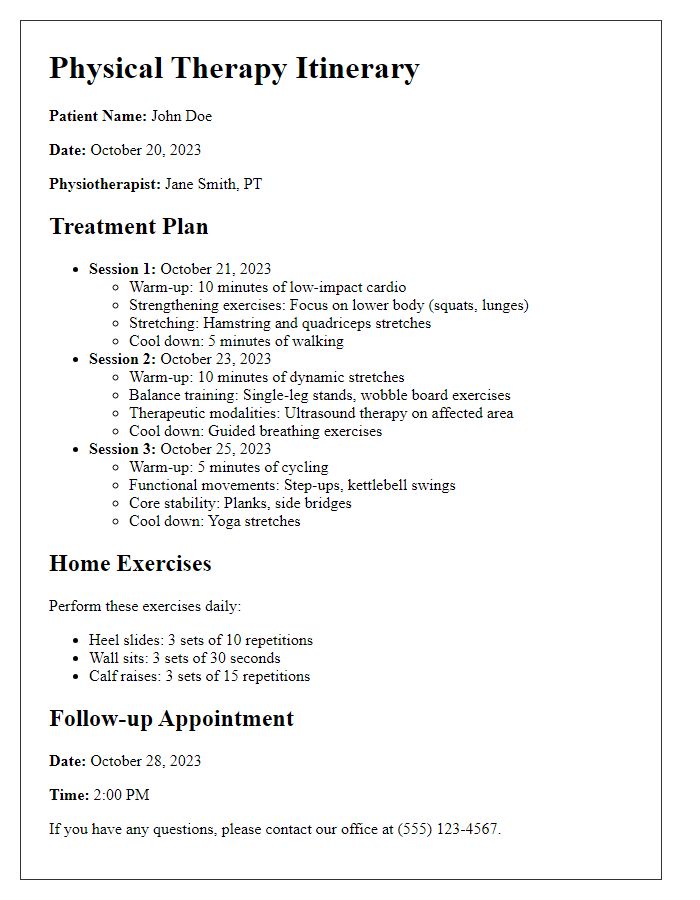
Letter template of detailed patient-specific physical therapy itinerary.
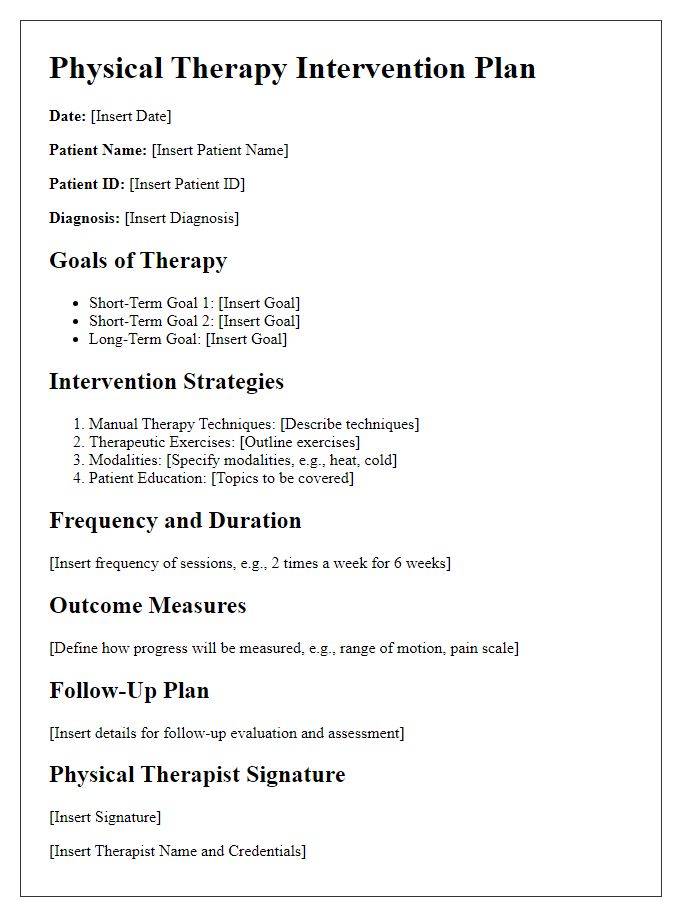
Letter template of structured physical therapy intervention plan for recovery.


Comments