Are you looking for a way to enhance your asthma management plan? Crafting a personalized letter template can be a game-changer in keeping track of your symptoms and triggers. By updating your asthma management plan, you can ensure your health stays prioritized and your daily activities remain uninterrupted. Join me as we dive deeper into effective strategies for managing asthma with our comprehensive guide!
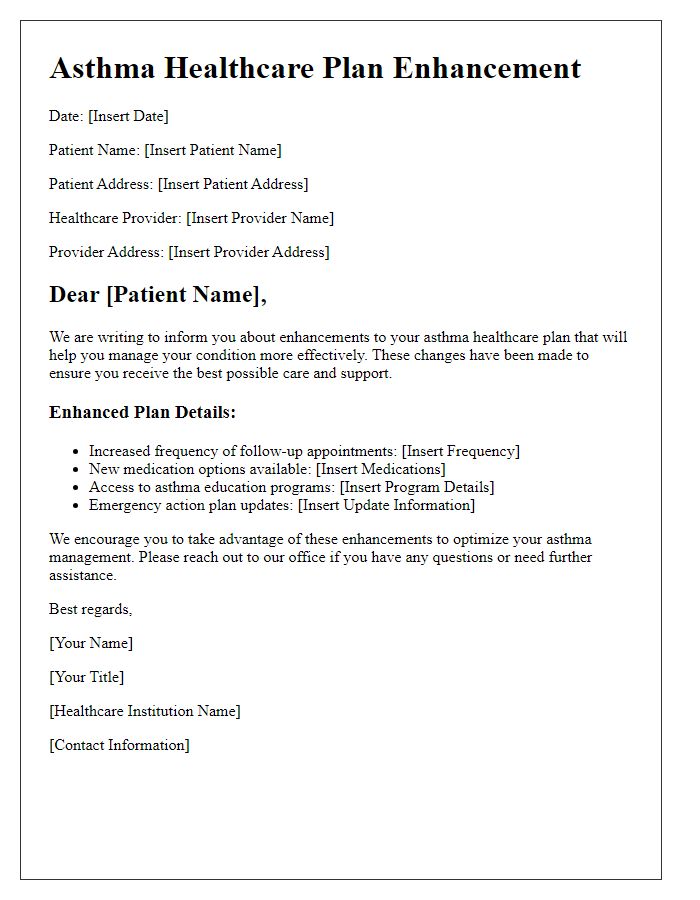
Patient Identification and Details
Asthma management plans are essential for individuals diagnosed with asthma, a chronic inflammatory disease affecting the airways in the lungs. Patient identification involves crucial information, including full name, date of birth (DOB) often recorded in a MM/DD/YYYY format, and unique medical record number (MRN). Details such as emergency contact information, including name and phone number, as well as primary healthcare provider's contact information including name, address, and phone number, are vital for coordinating care. Noteworthy medical history should encompass previous asthma attacks, hospitalizations related to asthma, frequency of inhaler use, and any comorbidities like allergic rhinitis or gastroesophageal reflux disease (GERD) that may impact asthma control. Additionally, documenting current medications, such as corticosteroids or bronchodilators, prescribed dosages, and administration frequency is crucial for personalized treatment adjustments. An updated asthma action plan delineates symptoms, trigger identification, and individualized strategies for managing exacerbations, ensuring comprehensive and effective care for the patient.
Current Asthma Symptoms and Triggers
Current asthma symptoms, including wheezing, shortness of breath, and frequent coughing, often arise and intensify in response to specific triggers. Common triggers include allergens such as pollen (grass, tree, and weed types), dust mites (found in bedding and upholstery), pet dander (skin flakes from cats and dogs), and mold spores (commonly found in damp areas). Environmental factors such as air pollution (from vehicles and industrial activities), tobacco smoke, and extreme weather changes (temperature fluctuations and humidity) can exacerbate these symptoms. Additionally, respiratory infections, particularly viral infections like the common cold, often lead to heightened asthma symptoms. Regular monitoring and identifying these triggers are crucial for effective asthma management and symptom control.
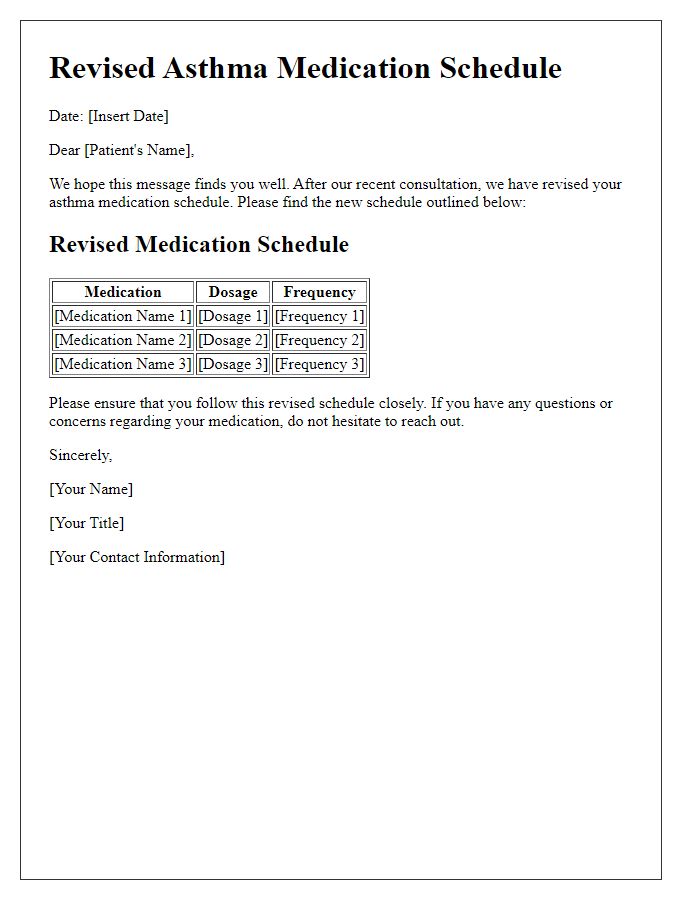
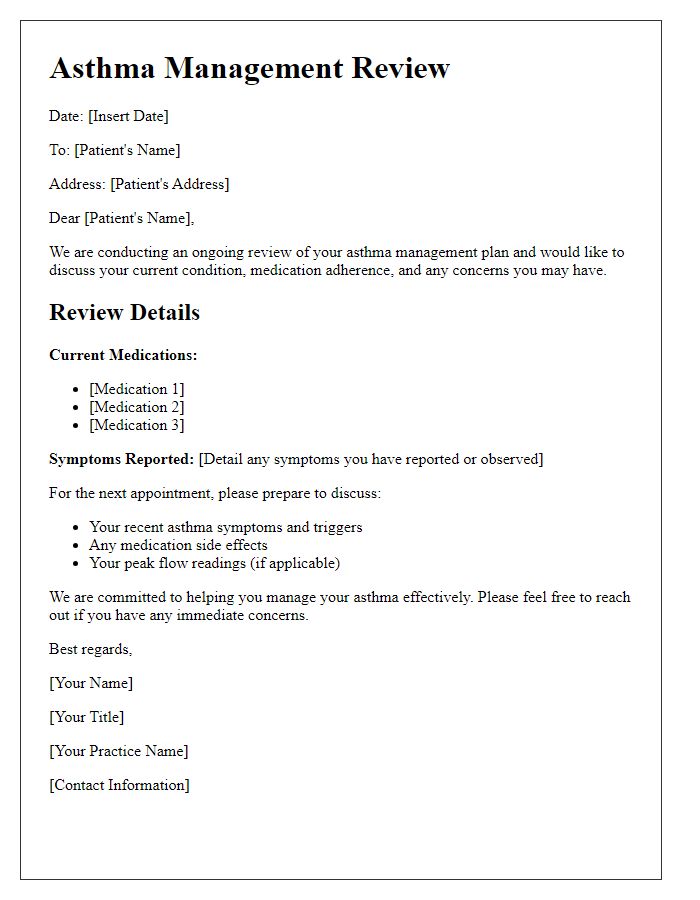
Medication Review and Adjustments
Asthma management plans require regular updates to ensure optimal control of symptoms and medication efficacy. A comprehensive medication review for individuals with asthma includes evaluating bronchodilator effectiveness, such as short-acting beta-agonists (SABAs) like albuterol, prescribed for quick relief of acute symptoms. Long-term controllers, like inhaled corticosteroids (ICS) such as fluticasone, must also be assessed for dosage adjustments based on current severity levels, including frequency of nighttime symptoms and peak expiratory flow rates (PEFR) measured using a peak flow meter at least twice weekly. Additional consideration should be given to the introduction of leukotriene modifiers such as montelukast for individuals experiencing allergic triggers in specific environments, such as pollen-heavy seasons or pet dander exposures. Documentation of changes is vital during follow-up appointments, scheduled every 3 to 6 months, to ensure adherence and address any side effects that may influence treatment compliance and overall health stability.
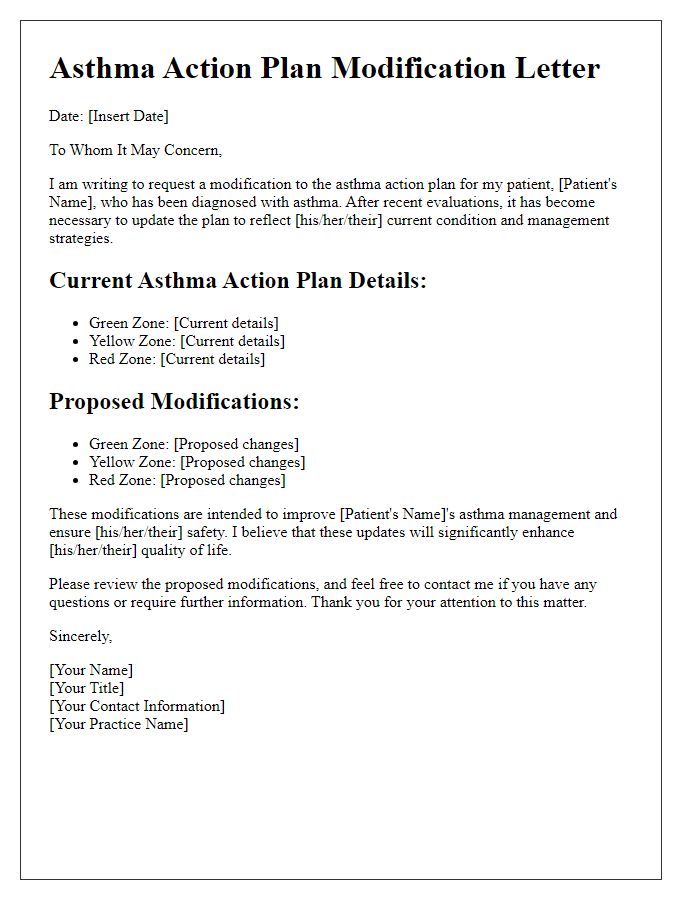
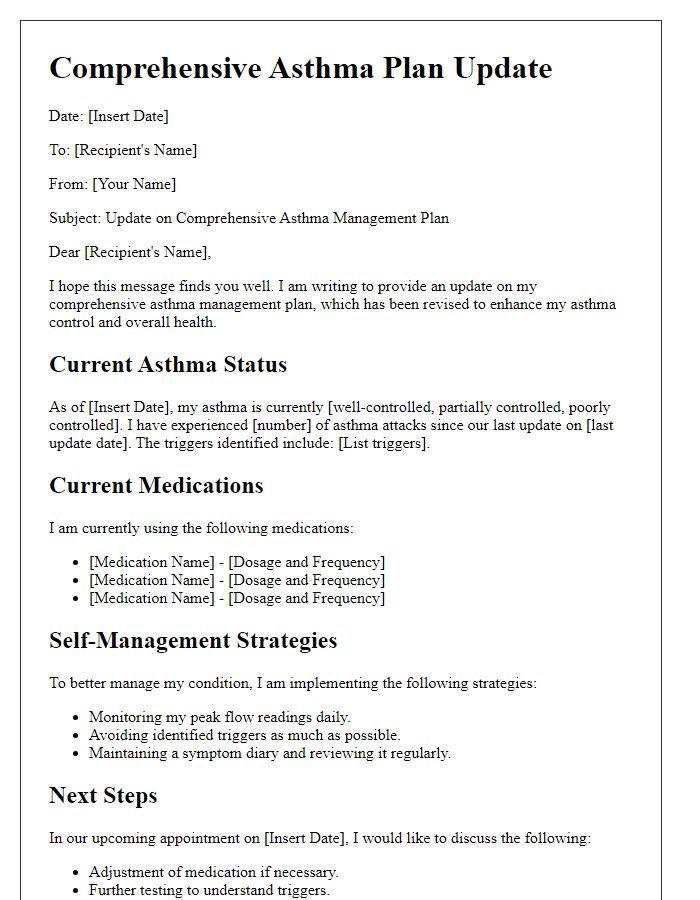
Action Plan for Asthma Exacerbations
Asthma management plans outline critical steps for handling exacerbations effectively, particularly in pediatric patients diagnosed with asthma. Patient-specific details, such as triggers identified through monitored events (e.g., pollen levels exceeding 50 grains per cubic meter or cold air exposure), can be integral to maintaining optimal respiratory health. Medication adherence is highlighted, with rescue inhalers like albuterol prescribed at dosages of 90-180 micrograms, providing essential relief during episodes. Regular consultations with healthcare providers in facilities like local pediatric asthma clinics can facilitate timely adaptations of the action plan. Additionally, employing a peak flow meter can track lung function, with readings under predicted values signaling necessary interventions, including potentially adjusting long-term control medications. Emergency services contact numbers must remain readily available, ensuring swift actions can be taken for severe exacerbations, thus promoting safety and wellness in everyday life for those affected.
Scheduled Follow-up and Monitoring
An effective asthma management plan update is essential for individuals affected by asthma, a chronic respiratory condition characterized by airway inflammation and constriction. Scheduled follow-ups, typically occurring every six months or as advised, facilitate comprehensive assessments of asthma control, medication efficacy, and symptom frequency. Monitoring tools, such as peak flow meters, assist patients in tracking lung function, specifically measuring the maximum speed of expiration in liters per minute, crucial for identifying worsening symptoms. Education on recognizing triggers--common allergens like pollen, dust mites, or smoke--is vital for prevention strategies. Adjusting medications, including inhaled corticosteroids or bronchodilators, based on physician recommendations ensures optimal asthma management. Regular updates to the action plan, tailored for individual needs, enhance readiness during asthma attacks, ultimately improving quality of life for those managing this condition.


Comments