Have you ever wondered what steps need to be taken for an emergency medical evacuation? Navigating the ins and outs of this process can be daunting, especially in a high-pressure situation. Whether it's for a loved one, a colleague, or yourself, understanding what to expect and how to prepare can make all the difference. Join me as we explore the essential details of emergency medical evacuation proceduresâthere's so much more to uncover!
Patient Identification and Medical History
Patient identification is crucial for emergency medical evacuation processes, ensuring accurate transfer of responsibility. Full name, date of birth, and medical record number (MRN) facilitate identification. Medical history must include significant pre-existing conditions, allergies (such as to medications like penicillin), current medications (potential interactions or contraindications), and previous surgeries. Chronic illnesses (e.g., asthma, diabetes) require specific attention, especially if they impact immediate care. Vital signs (blood pressure, heart rate) at the time of evacuation serve as critical indicators for medical personnel. It is essential to communicate any recent diagnoses or treatments, allowing the responding medical team to prepare for appropriate interventions during transport.
Current Medical Situation and Diagnosis
Current medical situations can escalate rapidly, especially in remote locations lacking immediate healthcare facilities. A patient diagnosed with pulmonary embolism, which entails the blockage of arteries in the lungs often due to blood clots from deep vein thrombosis, requires urgent attention. Symptoms like severe chest pain, shortness of breath, and rapid heartbeat can manifest suddenly, necessitating swift medical intervention. In instances where local medical resources, such as specialized medical equipment or skilled personnel, are insufficient, organizing an emergency medical evacuation to a facility equipped to provide advanced care becomes critical. The evacuation process may involve air ambulances fitted with life-sustaining technology, capable of facilitating transport to hospitals renowned for treating life-threatening conditions.
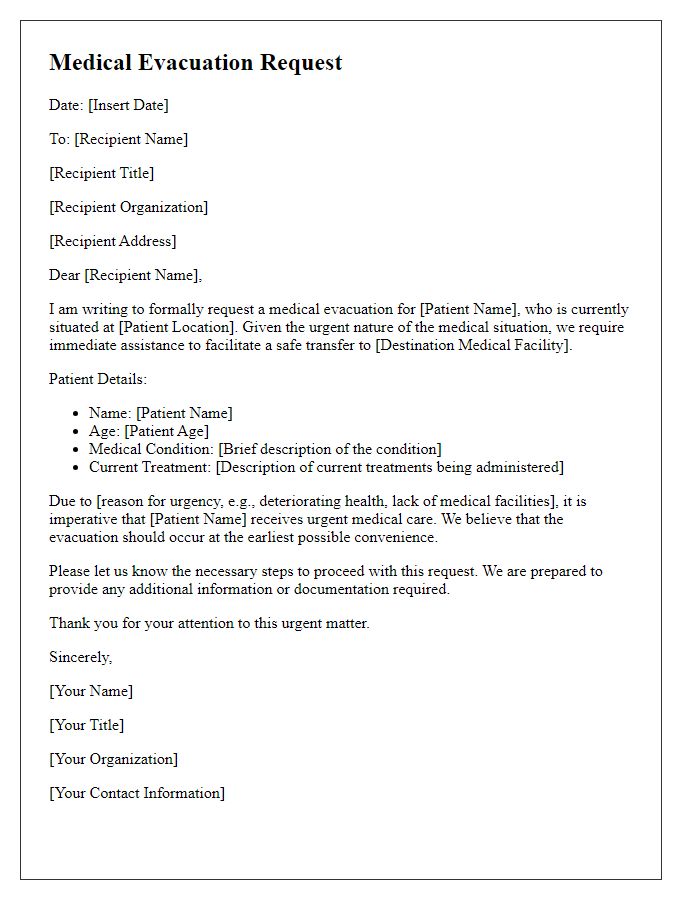
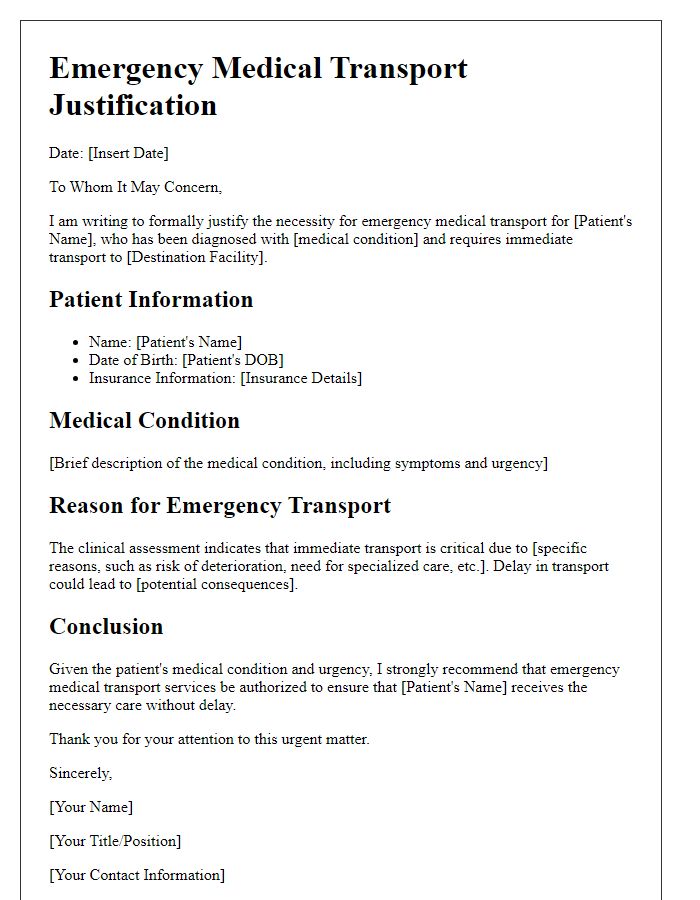
Justification for Evacuation
Emergency medical evacuation (medevac) occurs when immediate transport is necessary to ensure patient safety and optimize medical outcomes. Conditions such as severe trauma, life-threatening illnesses, or acute respiratory distress can necessitate this urgent response. Transporting a patient from remote locations, such as natural disaster sites or conflict zones, often involves aircraft like helicopters or fixed-wing planes, facilitating rapid access to advanced medical facilities. Distance plays a crucial role; for instance, a patient in a remote region located over 100 miles from the nearest hospital may require urgent medevac procedures. Timeliness, typically within the critical care window of two hours, greatly influences survival rates and recovery potential, justifying the need for decisive action in emergency medical situations.
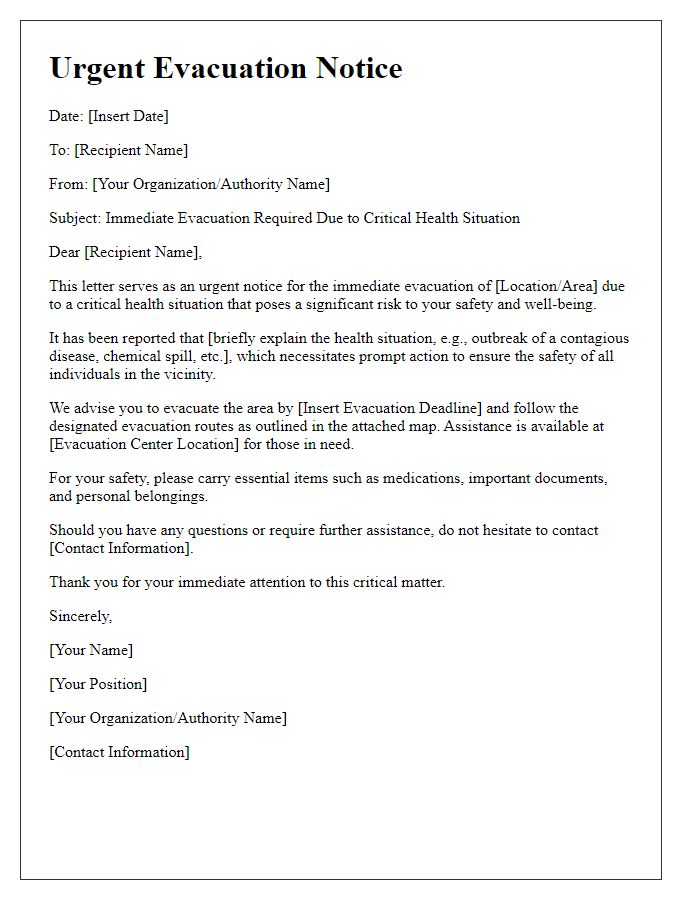
Evacuation Logistics and Arrangements
Emergency medical evacuation (medevac) logistics involve precise planning and coordination to ensure patient safety and timely transport. Air ambulances, equipped with advanced medical equipment, are essential for quickly transporting critically ill patients from remote locations, such as disaster sites or offshore oil rigs, to medical facilities. Ground ambulances serve as a crucial link for initial transport to helipads or airports. Medical professionals, including paramedics and flight nurses, accompany patients throughout the journey, providing continuous care. Communication with hospitals, like those in urban centers such as Chicago or New York, is vital for seamless transfer. Weather conditions, air traffic, and location accessibility significantly influence the evacuation schedule, requiring flexible and adaptive response strategies to ensure the best possible patient outcomes.
Contact Information for Medical Personnel and Family
In emergency medical evacuation situations, timely communication is critical for coordinating effective medical response. Contact information for medical personnel should include names, qualifications, and specialty areas, such as emergency physicians or paramedics. Additionally, family contact details should comprise their full names, relationships to the patient, and primary phone numbers for immediate communication. This information is essential for notifying family members about the patient's condition and location, as well as facilitating coordination with healthcare providers at the receiving medical facilities. Proper documentation of these contacts can significantly enhance the efficiency and effectiveness of emergency medical operations, ensuring that all parties involved are informed and prepared for any necessary actions.



Comments