Keeping track of your health is an essential part of managing any medical condition, and regular symptom monitoring can make a significant difference in your treatment journey. In this article, we'll explore effective strategies for maintaining an accurate record of your symptoms, which can help you communicate more effectively with your healthcare provider. We'll also discuss the importance of identifying patterns and triggers that influence your well-being. So, if you're looking to enhance your health management skills, join us as we dive deeper into this important topic!
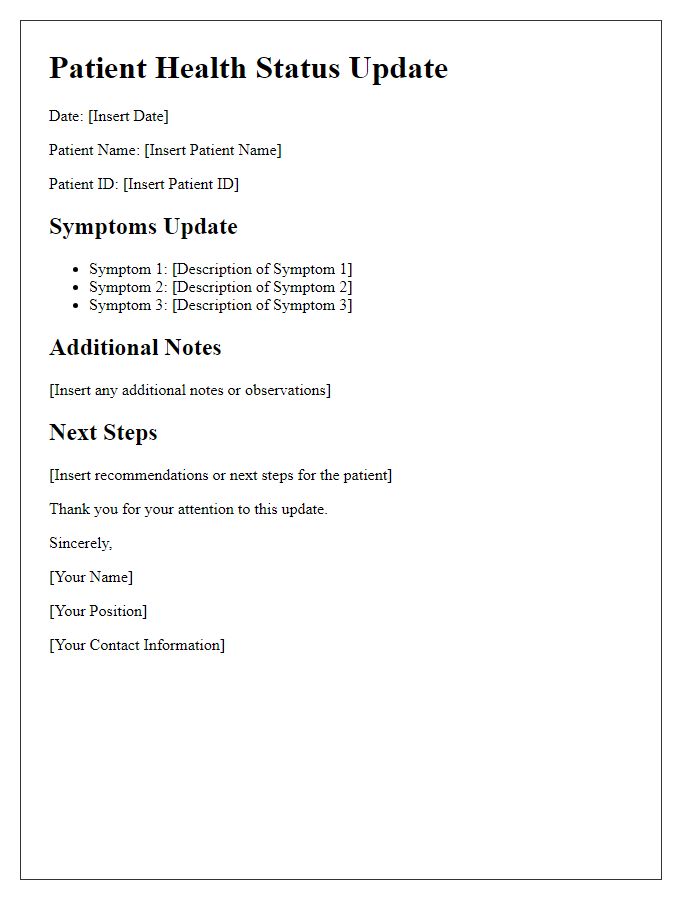
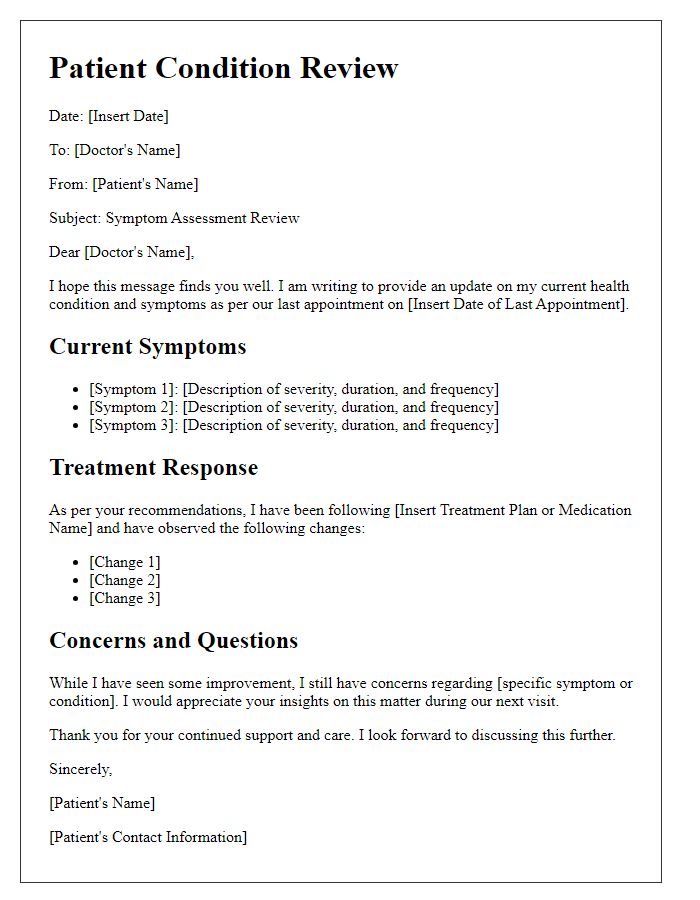
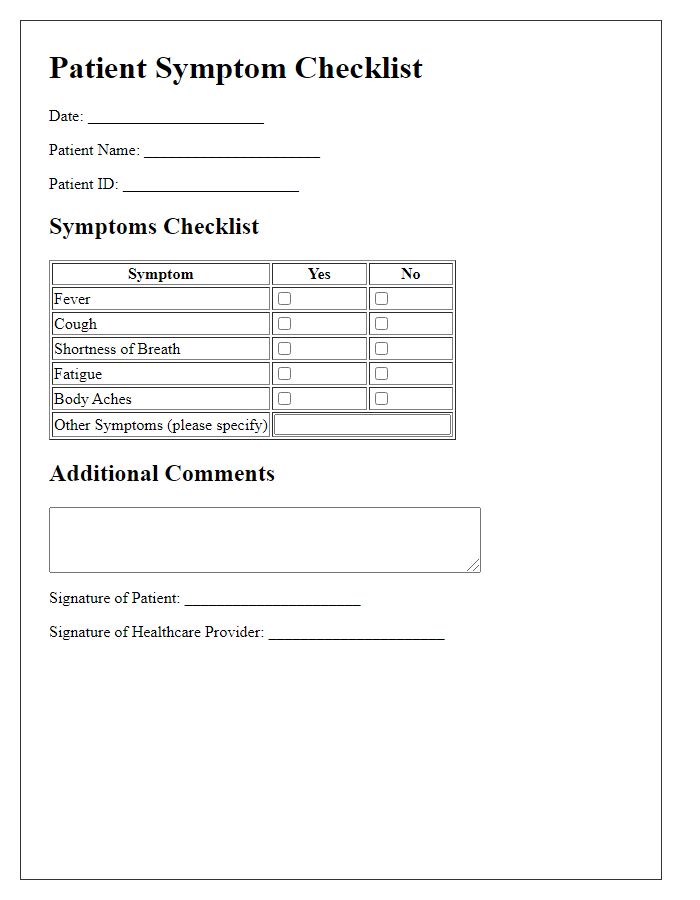
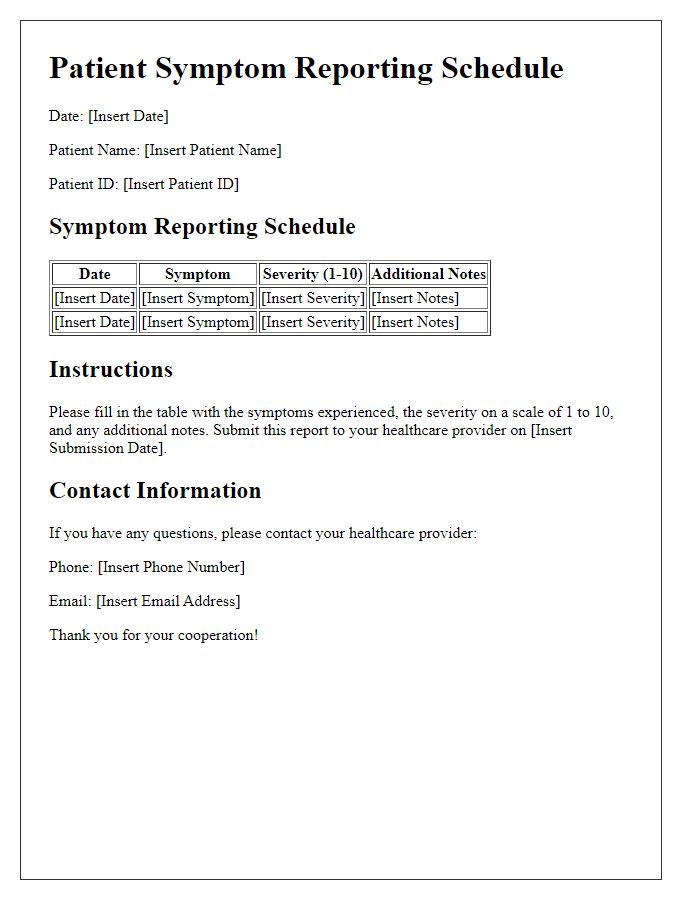
Patient Identification Information
Patient symptom monitoring provides crucial insights into health management. Accurate identification through patient information records, such as name, date of birth, and unique health identification number, ensures personalized treatment. Detailed symptom tracking, including frequency, duration, and intensity, assists healthcare professionals in diagnosing conditions effectively. Consistent updates captured in digital health systems offer an overview of changes, linking symptoms to potential triggers or treatments. This systematic approach improves communication between patients and providers, ultimately enhancing care quality.
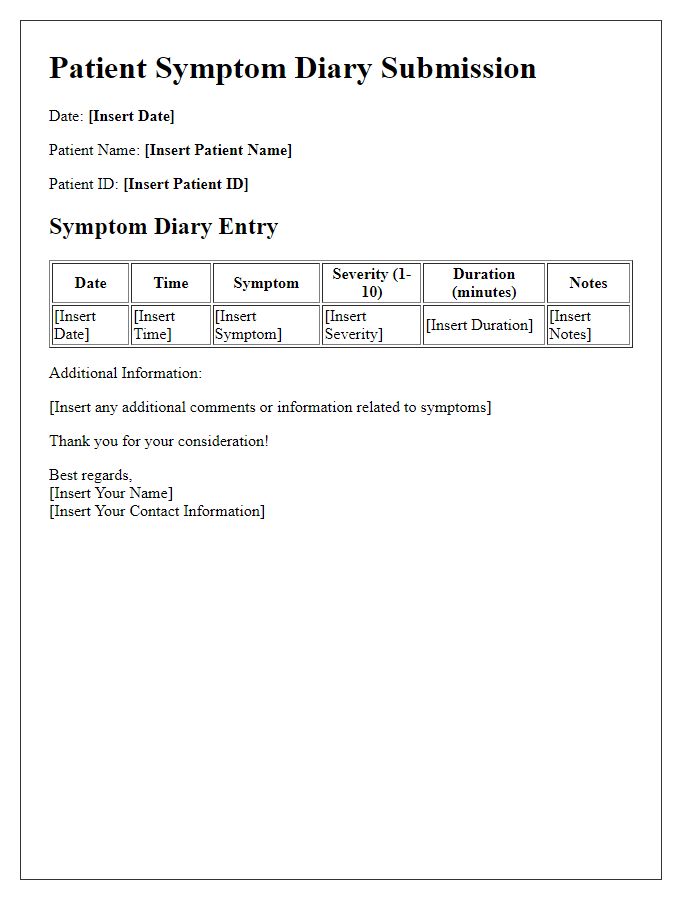
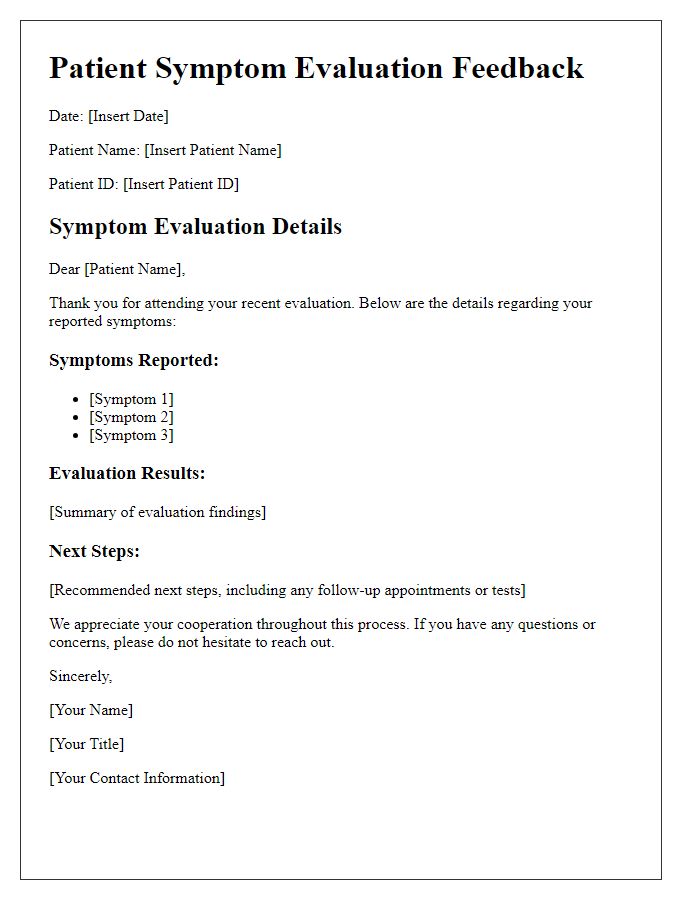
Symptom Description and Duration
Patient symptom monitoring involves detailed observation of specific health indicators, enabling proactive management of conditions. For example, chronic cough lasting over three weeks can indicate respiratory issues such as asthma or chronic bronchitis. Abdominal pain persisting for more than two days might suggest gastrointestinal conditions like appendicitis or gallstones. Fatigue extending beyond a month could signify underlying conditions, including thyroid dysfunction or anemia. Monitoring changes in symptoms, their frequency, and intensity is crucial in clinical decisions. Regular updates facilitate timely interventions, ensuring personalized care tailored to each patient's evolving health status.
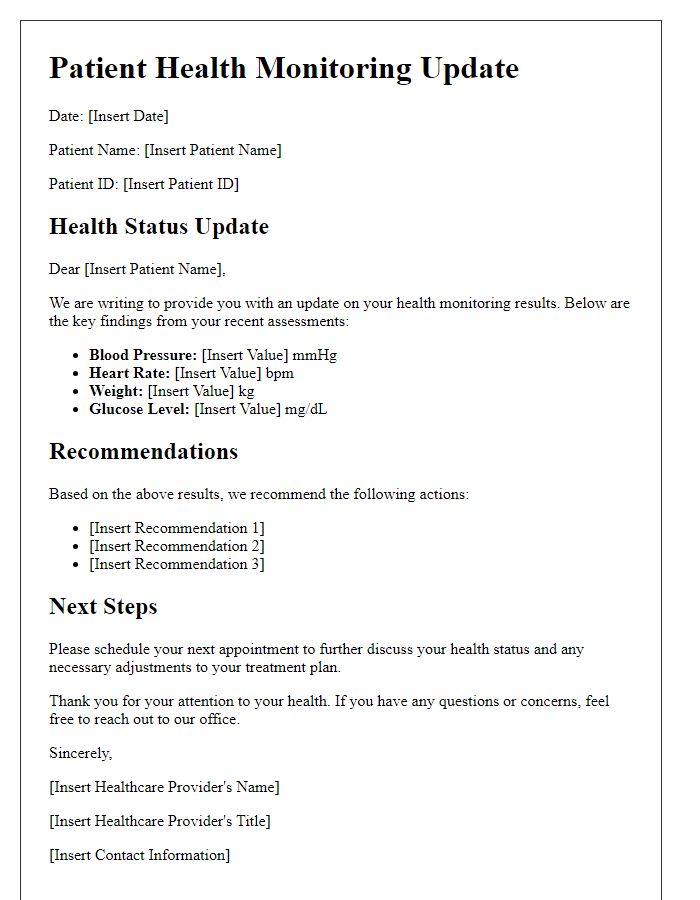
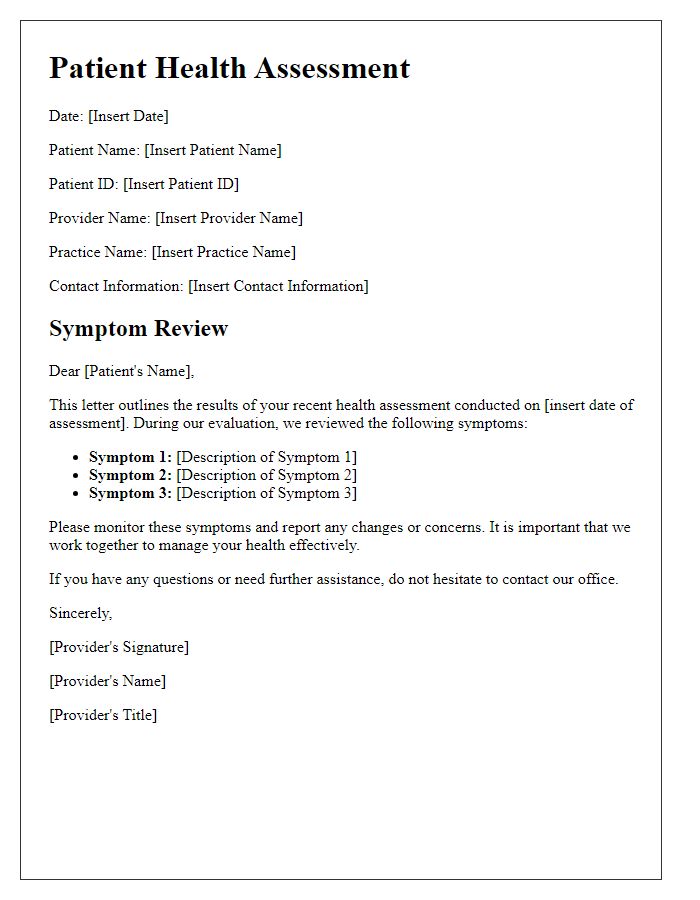
Treatment or Medication Changes
Prolonged use of corticosteroids, specifically Prednisone, often leads to significant changes in symptom management for patients with autoimmune conditions. Elevated dosages, such as 40 mg daily, can result in increased appetite, weight gain, and mood swings, drastically affecting daily life. Monitoring potential side effects, including hyperglycemia (raised blood sugar levels exceeding 130 mg/dL), is crucial to prevent complications such as diabetes. Regular follow-up appointments, typically scheduled every four weeks, should assess these symptoms and adjust pain management protocols, including the possible integration of non-steroidal anti-inflammatory drugs (NSAIDs), to enhance the overall treatment effectiveness. Timely feedback from patients regarding their response to medications, especially when dosage changes occur, is essential for optimizing long-term health outcomes.
Observation Notes and Patterns
Monitoring patient symptoms over time can reveal significant patterns that inform effective treatment plans. For instance, a patient diagnosed with chronic migraine might report episodes occurring primarily on weekends, suggesting potential triggers related to changes in stress levels or sleep patterns. Documenting specifics such as frequency (up to five times a month), duration (lasting 24 hours), and associated symptoms (nausea, light sensitivity) enhances understanding. Moreover, noting external factors like weather changes (barometric pressure fluctuations) or dietary intake (increased caffeine consumption) can provide additional insight. Regular observation can facilitate timely interventions, enabling healthcare providers to devise personalized management strategies that address the unique needs of each patient.
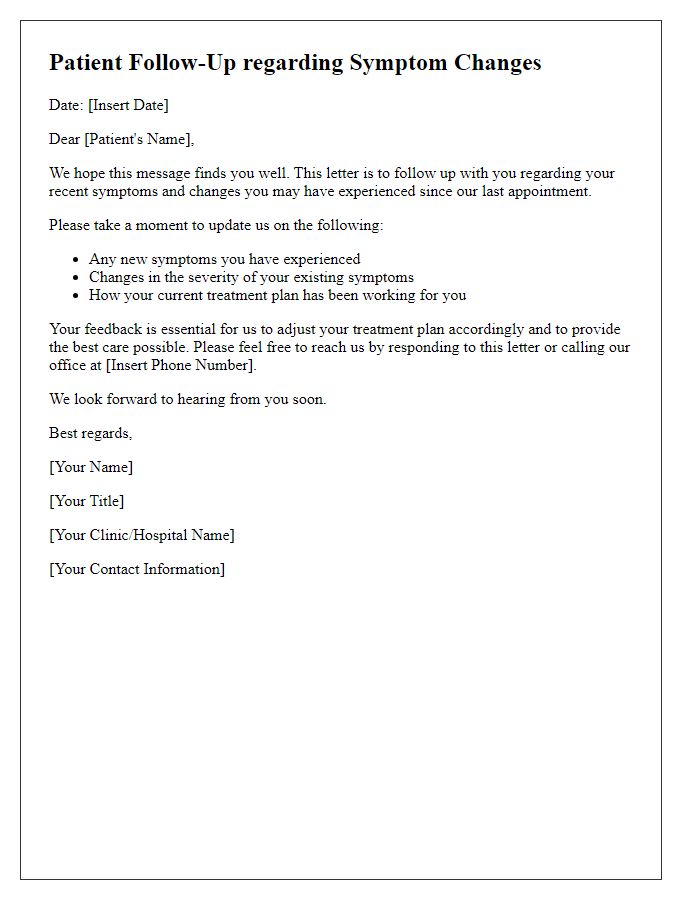
Next Steps and Follow-Up Plan
Patient symptom monitoring updates require careful documentation. Clinicians should record specific changes in symptoms, such as increased pain levels from 4 to 7 on a scale of 10, or shifts in mood reflecting anxiety triggered by recent life events. The follow-up plan may include scheduled appointments, either virtual or in-person, possibly at a facility like General Hospital, targeting specific symptoms such as insomnia. Recommendations could outline prescription adjustments for medications like antidepressants and additional referrals to specialists such as psychiatrists or physical therapists. Monitoring tools, including daily symptom diaries or mobile health applications, can assist in tracking progress and the effectiveness of interventions. Establishing clear communication channels, like secure messaging platforms, ensures timely updates and a proactive approach in managing the patient's health.



Comments