When it comes to respiratory health, understanding your condition is crucial for effective management and improvement. This letter serves as a friendly guide to help you assess your respiratory health, offering you insights into the symptoms and factors that may affect your breathing. Whether you're dealing with chronic issues or just looking to stay proactive, this assessment can provide valuable information. So, dive in and discover how you can take charge of your respiratory health by reading further!
Patient Information
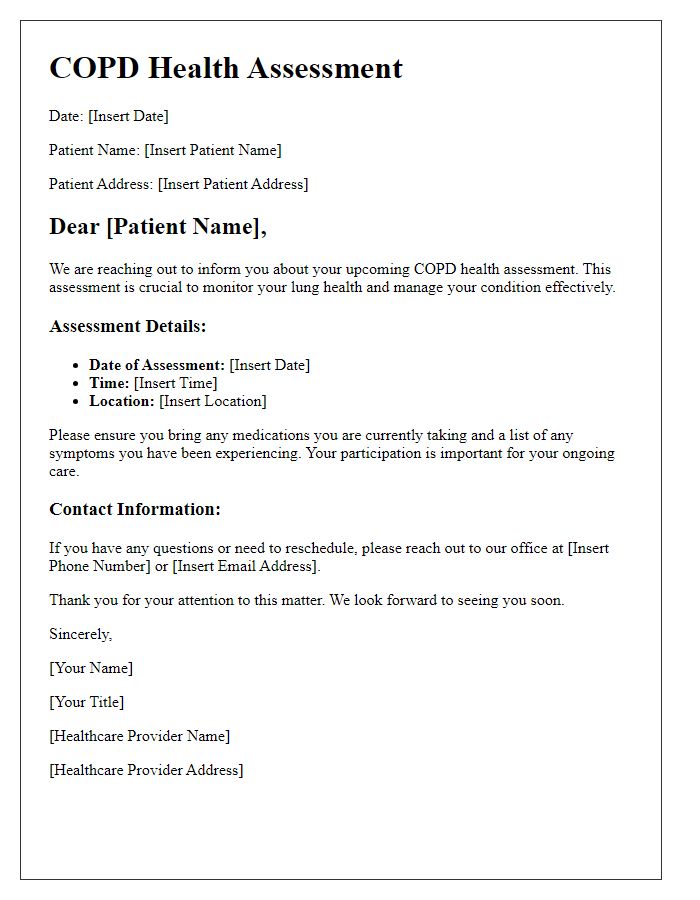
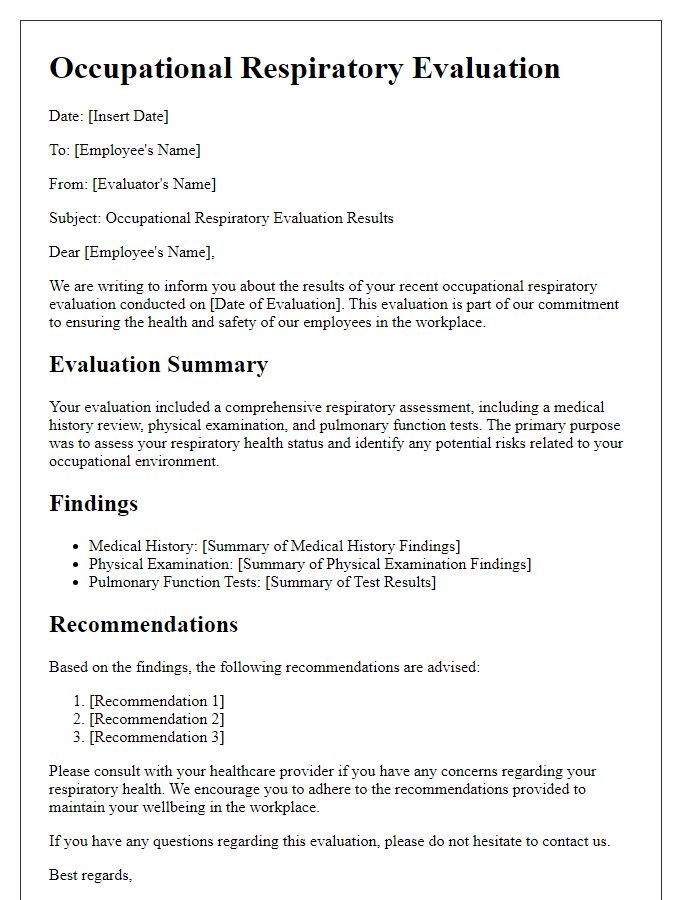
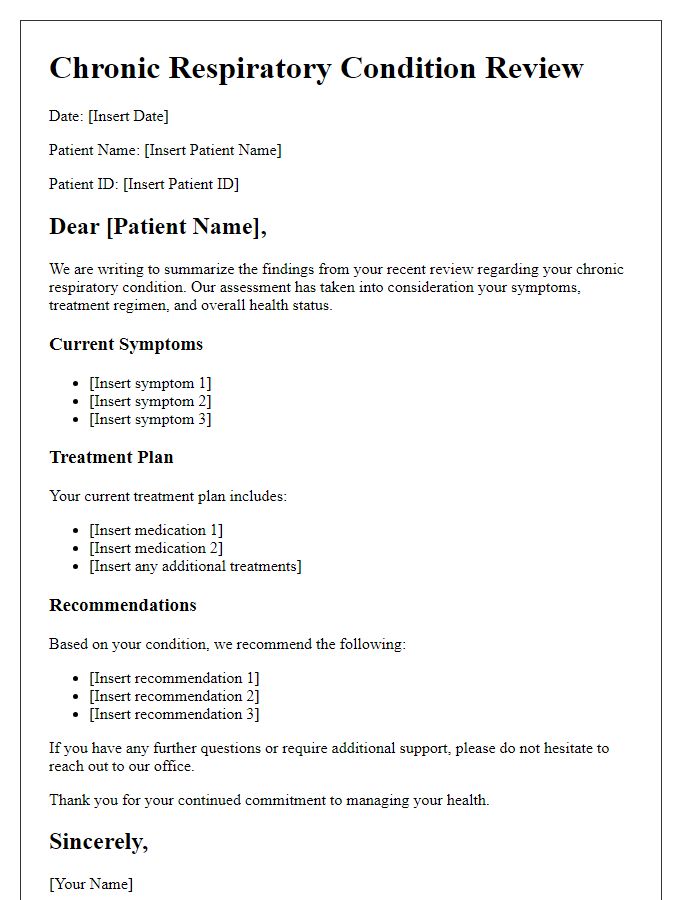
Respiratory health assessments provide crucial insights into pulmonary function and overall wellness. The evaluation typically includes patient demographics, such as age (often measured in years), gender (male or female), and lifestyle factors like smoking status (current, former, or never). Symptoms, including cough frequency (number of times per day), shortness of breath (graded on a scale from mild to severe), and wheezing episodes, should be documented in detail. Medical history should encompass previous respiratory conditions, such as asthma (a chronic inflammatory disease affecting the airways), chronic obstructive pulmonary disease (COPD, characterized by persistent respiratory symptoms), and any hospitalizations related to respiratory issues. Environmental exposures should also be noted, encompassing allergens (like pollen and dust mites), occupational hazards (such as chemicals or fumes), and geographical factors (like urban pollution levels). Accurate and thorough patient information enhances the effectiveness of the respiratory health assessment, ultimately guiding treatment plans.
Purpose of Assessment
Respiratory health assessments aim to evaluate lung function and identify underlying conditions affecting breathing, such as Chronic Obstructive Pulmonary Disease (COPD) or asthma. These assessments typically involve measurements of lung capacity through spirometry tests, which quantifies parameters like Forced Expiratory Volume (FEV1) and Forced Vital Capacity (FVC). Understanding respiratory health is crucial for populations exposed to environmental pollutants, particularly in urban areas like Los Angeles, which suffers from significant air quality issues. Additionally, such assessments can help healthcare providers develop tailored treatment plans and interventions to improve patients' quality of life, especially among vulnerable groups, including the elderly and those with pre-existing health conditions.
Medical History
Respiratory health assessments are crucial for understanding patient conditions related to the lungs and airways. Comprehensive medical history includes key details such as asthma diagnosis, chronic obstructive pulmonary disease (COPD) experiences, and past respiratory infections, like pneumonia. Documentation of exposure to environmental factors, such as smoking history with pack-years quantified, occupational hazards in industries like construction or manufacturing, and living conditions in locations with high air pollution, provides context. Family history of respiratory diseases, including hereditary conditions like cystic fibrosis or alpha-1 antitrypsin deficiency, plays a vital role. Notable symptoms, such as chronic cough or shortness of breath, are assessed alongside current medications, including bronchodilators or corticosteroids, to evaluate treatment effectiveness. These detailed notes guide healthcare professionals in diagnosing, treating, and monitoring respiratory health accurately.
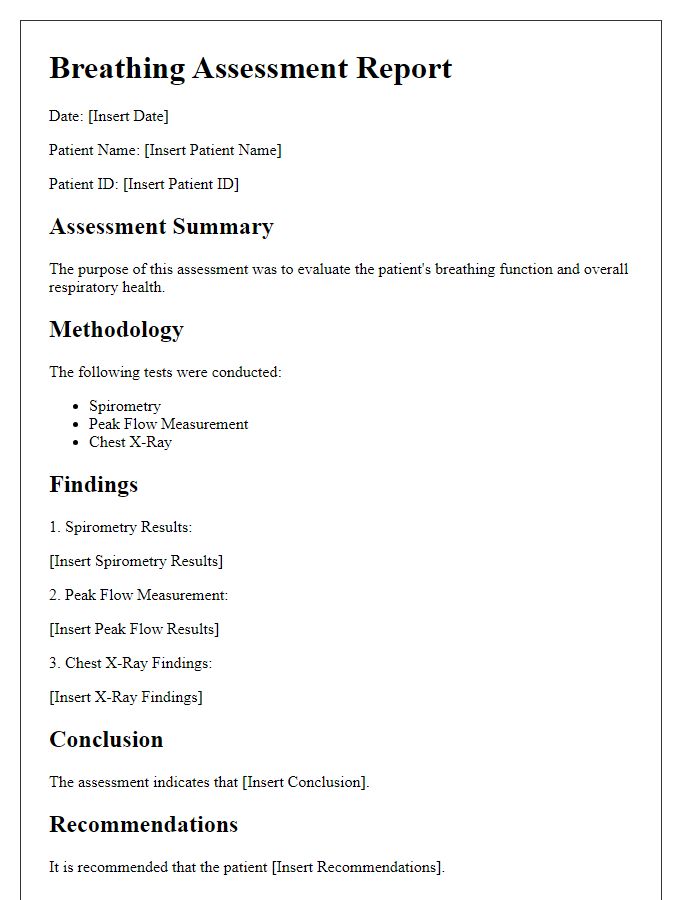
Assessment Procedures
Respiratory health assessments involve a comprehensive evaluation of lung function and overall respiratory status. This includes spirometry testing, which measures airflow and volumes of air inhaled and exhaled, essential for diagnosing conditions like asthma or chronic obstructive pulmonary disease (COPD). A peak flow meter may be used, providing real-time data on the patient's maximum speed of expiration, crucial for monitoring asthma control. Observations of auscultation, where a healthcare professional listens to lung sounds using a stethoscope, can reveal abnormalities indicating infections, fluid buildup, or bronchoconstriction. Additionally, a detailed patient history regarding exposure to environmental irritants, allergens, and smoking habits will be documented, ensuring tailored management plans are developed. Chest X-rays or CT scans may be incorporated into assessment protocols if structural problems are suspected.
Follow-up Instructions
Follow-up instructions for respiratory health assessments are crucial for ensuring patient progress and well-being. Patients with chronic respiratory conditions, such as asthma or chronic obstructive pulmonary disease (COPD), should monitor symptoms daily, recording peak flow meter readings to track lung function. Scheduling follow-up appointments every three months is recommended for ongoing evaluation and adjustment of treatment plans. Patients must adhere to prescribed medications, including inhalers and nebulizers, to manage symptoms effectively. In the event of sudden worsening of breathing difficulties or increased reliance on rescue inhalers, patients should seek immediate medical attention. Lifestyle adjustments, such as avoiding smoke exposure and practicing breathing exercises, are also vital for improving overall lung health. Regular consultations with healthcare providers ensure timely interventions and optimal management of respiratory conditions.


Comments