Are you looking to streamline your dermatopathology visit summary? Creating a clear and comprehensive letter can make a world of difference for both patients and healthcare providers. In this article, we'll explore essential elements to include in your summary, ensuring that all necessary information is communicated effectively. Keep reading to discover tips and a handy template that you can personalize for your needs!
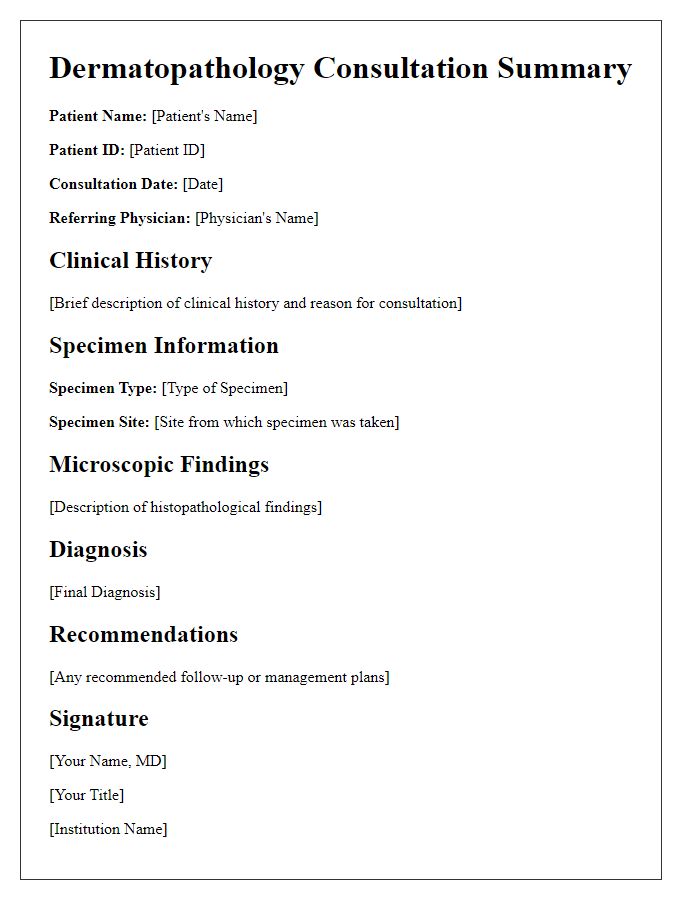
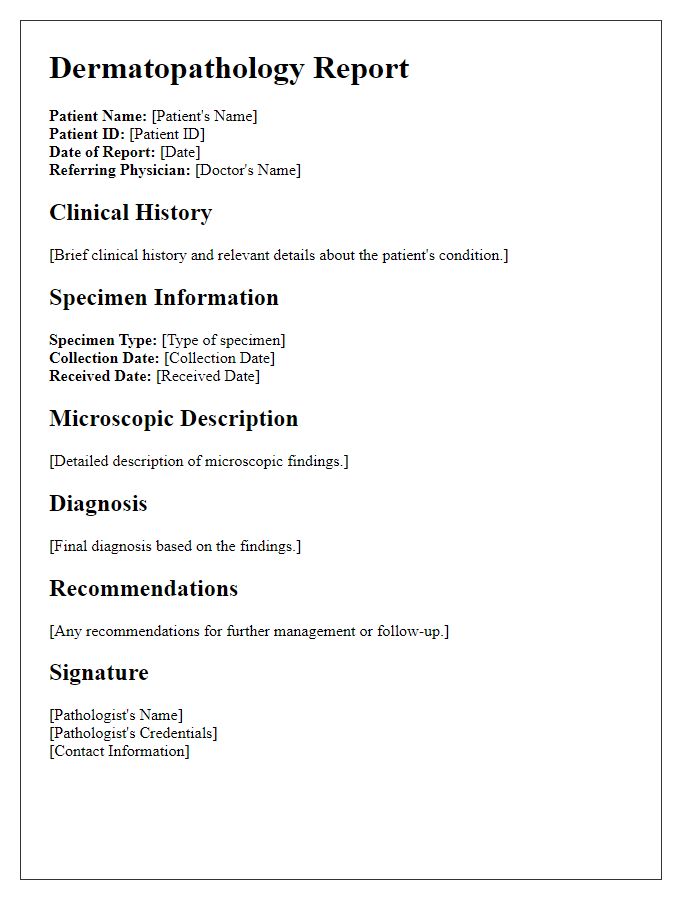
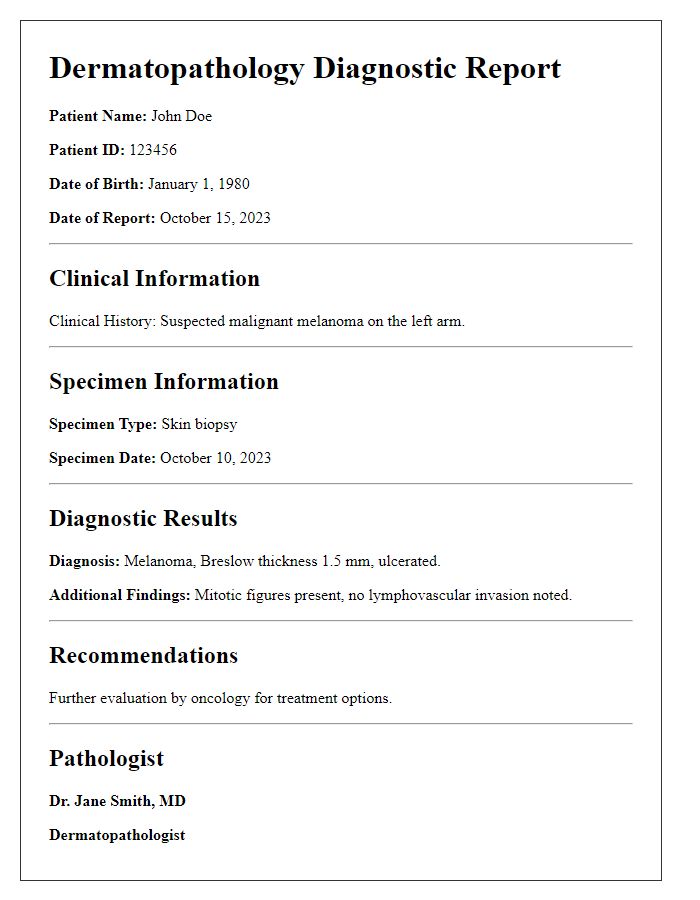
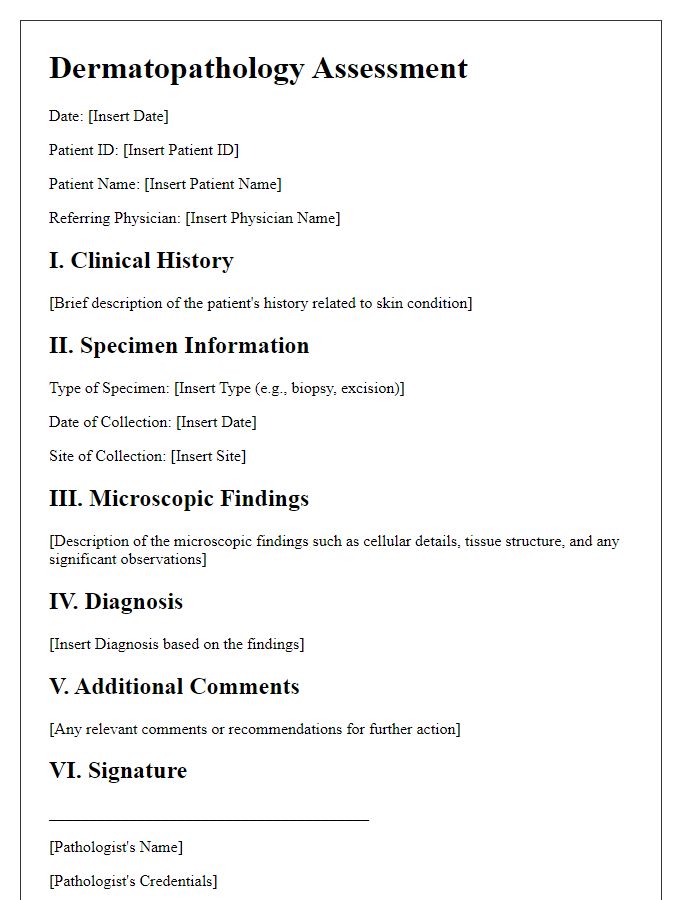
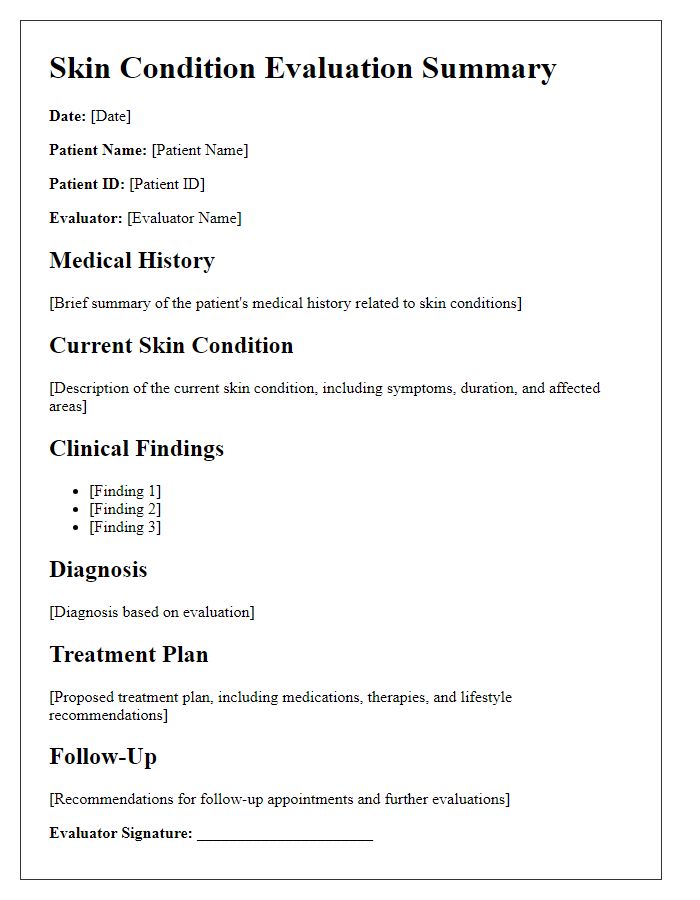
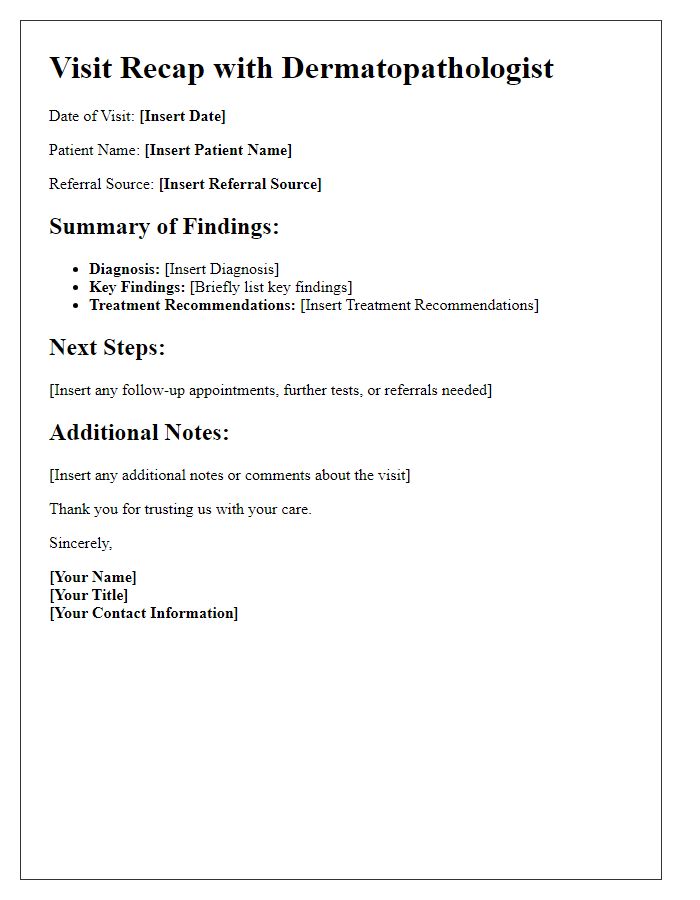
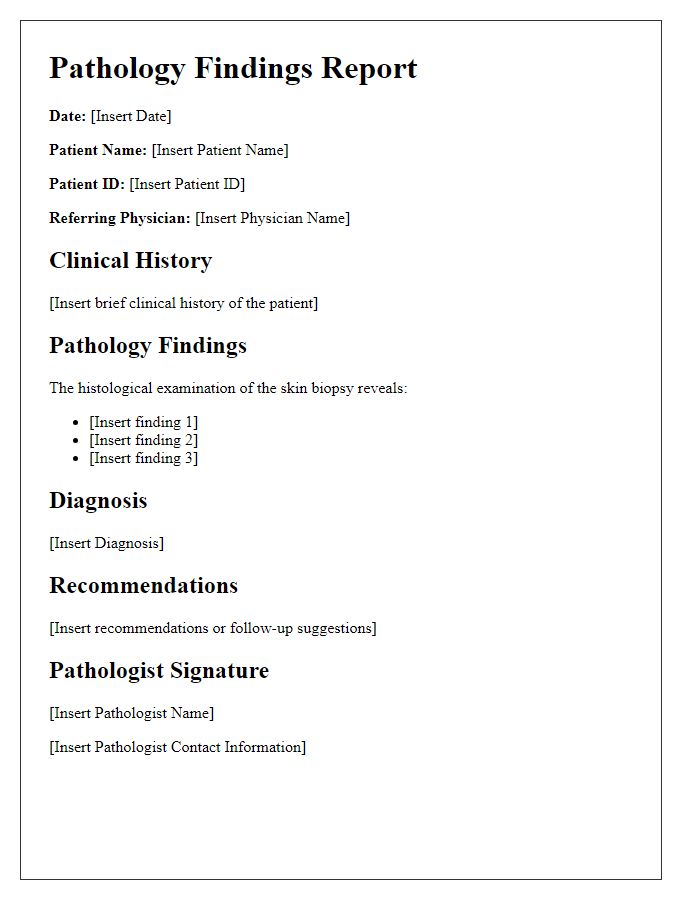
Patient Identification and Demographics
Patient identification in dermatopathology includes essential details such as the patient's full name, date of birth for age verification (e.g., June 15, 1985), gender (male or female), and unique identification number assigned by the healthcare facility. Demographics might encompass the patient's address, contact information (including phone number), and insurance provider details. Furthermore, record associated medical history, including previous dermatological issues (like skin cancer) and any pertinent family history (for example, melanoma in a sibling). This information is crucial for accurate diagnosis and tailored treatment plans during follow-up consultations by dermatologists and pathologists.
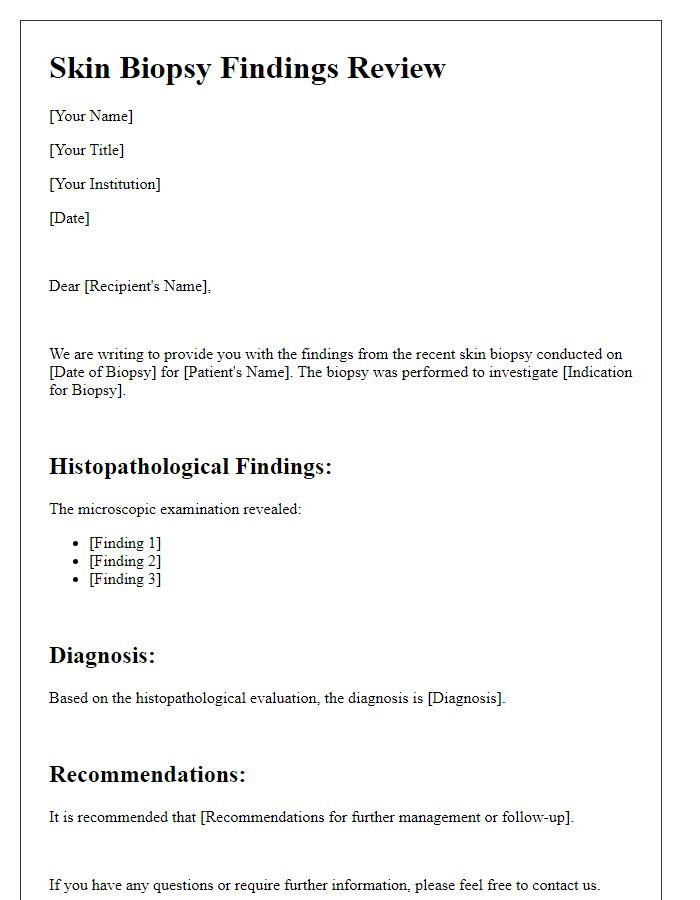
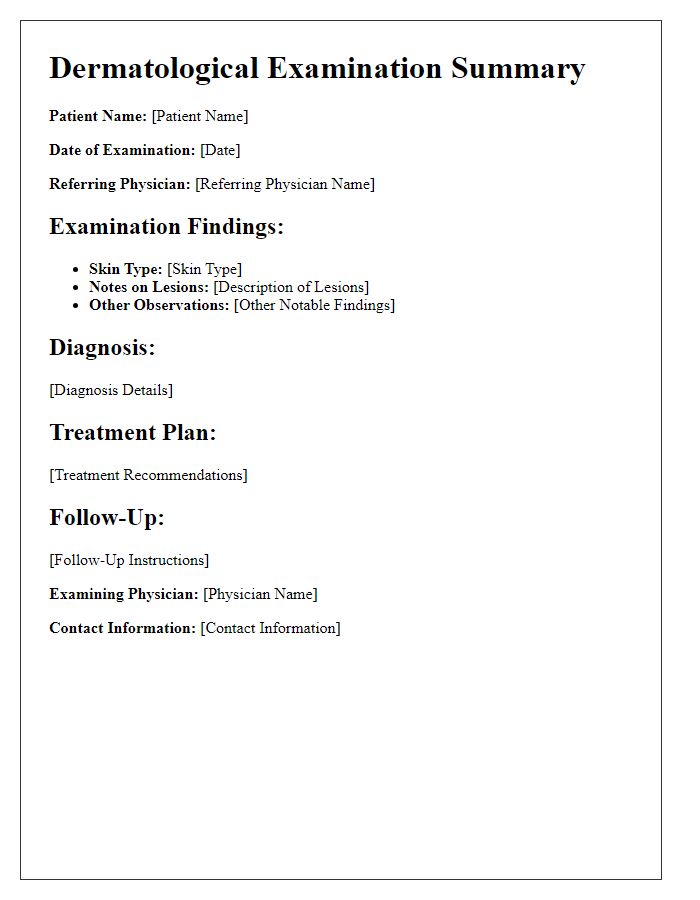
Clinical Findings and Diagnosis
During the dermatopathology visit, clinicians observed multiple lesions, some exhibiting irregular borders and color variations. Specific areas demonstrated signs of inflammation, suggesting an underlying skin condition. Histological analysis revealed a predominance of atypical keratinocytes and lymphocytic infiltrates, indicative of possible malignancy. Further diagnostic tests, including immunohistochemistry, confirmed the presence of malignant melanoma, staging it at Clark Level III and Breslow thickness of 2.5 mm. Recommendations for follow-up treatment include consultation with a surgical oncologist for potential excision and sentinel lymph node biopsy at an accredited institution, ensuring optimal management of the condition.
Histopathological Results
Histopathological results reveal critical insights into skin lesions, showcasing specific cellular morphology and tissue architecture analysis. In cases of melanoma, for instance, presence of atypical melanocytes may indicate aggressive behavior, necessitating follow-up assessments. Psoriasis, characterized by hyperkeratosis and acanthosis, displays distinct visible features under microscopic evaluation. Biopsy specimens from lesions exhibit varying degrees of dermal inflammation, with infiltrating lymphocytes or plasma cells suggesting possible autoimmune processes. Additional findings, such as the presence of fungal elements in dermatophyte infections, require distinct management protocols. Accurate interpretation of these histological findings is essential for developing effective treatment plans tailored to each patient's unique dermatological condition.
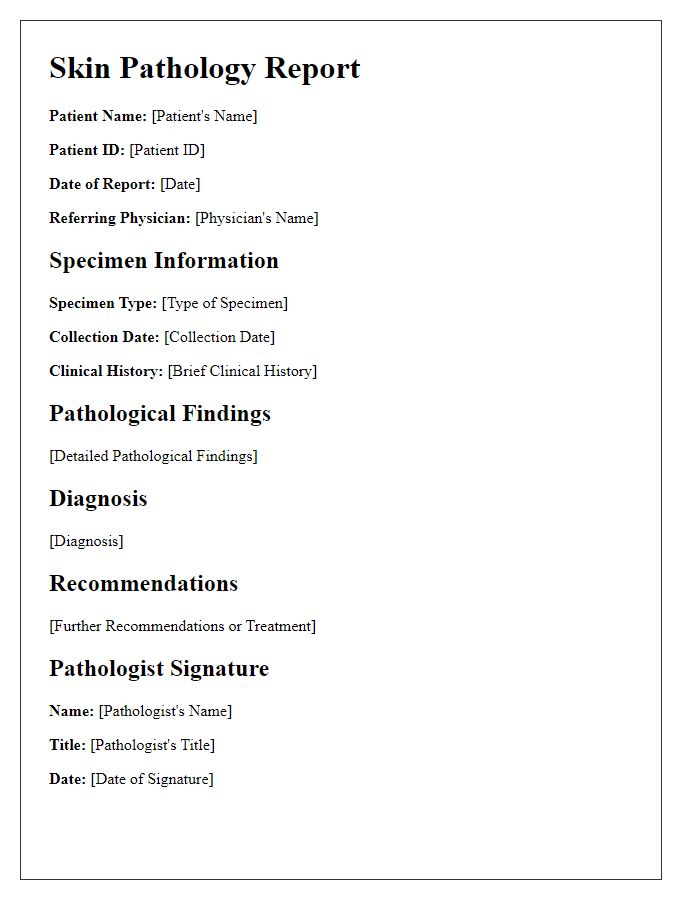
Treatment and Management Plan
During the dermatopathology visit, the physician evaluated skin conditions such as psoriasis and melanoma, noting the importance of pathology reports for accurate diagnosis. The management plan included a combination of topical treatments, including corticosteroids and retinoids, aimed at reducing inflammation and promoting skin regeneration. Additionally, the physician recommended follow-up appointments every three months at the dermatology clinic located in Boston, Massachusetts, to monitor progress and adjust treatment as necessary. The discussion emphasized patient education about potential side effects and preventative measures, such as sun protection and moisturizing routines, to enhance treatment efficacy and overall skin health.
Follow-up and Recommendations
A dermatopathology visit summary encompasses critical findings related to skin tissue examinations conducted by specialized pathologists. Patients often receive detailed reports regarding diagnoses such as melanoma, squamous cell carcinoma, or basal cell carcinoma, which require precise identification of cancer subtype and progression. For example, a patient may have a biopsy indicating early-stage melanoma with a Breslow depth of 0.7 millimeters, indicating a favorable prognosis. Recommendations for follow-up could include regular skin checks every three months for the first two years and potential referral to a medical oncologist for further assessment. Additional notes may stress the importance of self-examinations and monitoring any new or changing lesions, particularly in high-risk patients, such as those with a family history of skin cancer or previous skin malignancies. Adherence to treatment plans and lifestyle changes, such as sun protection and moisturizing routines, may be emphasized to optimize skin health post-diagnosis.


Comments