Welcome to our exploration of clinical trial protocol amendments! Navigating the intricacies of clinical trials can be a complex journey, and understanding the importance of protocol amendments is crucial for researchers and participants alike. These amendments can enhance trial integrity, ensure participant safety, and adapt to new findings. So, if you're curious about how these changes can impact clinical research, read on to discover more!
Regulatory compliance requirements
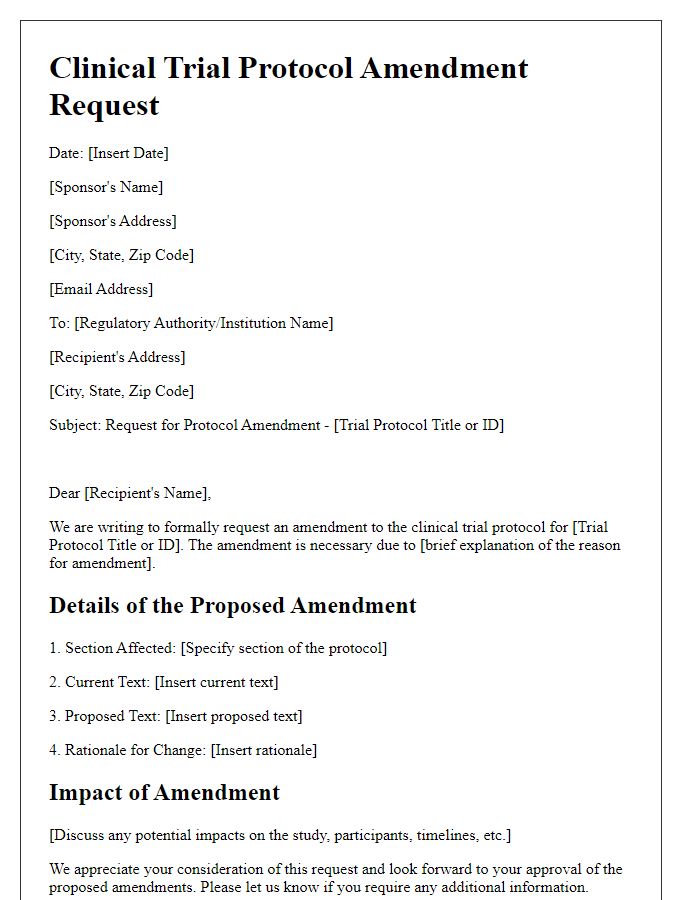
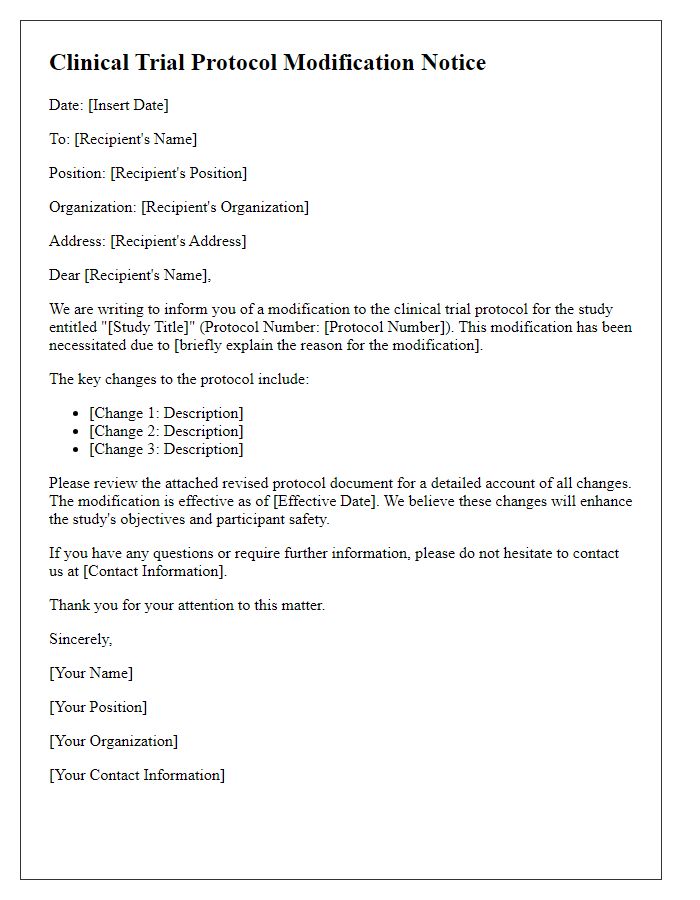
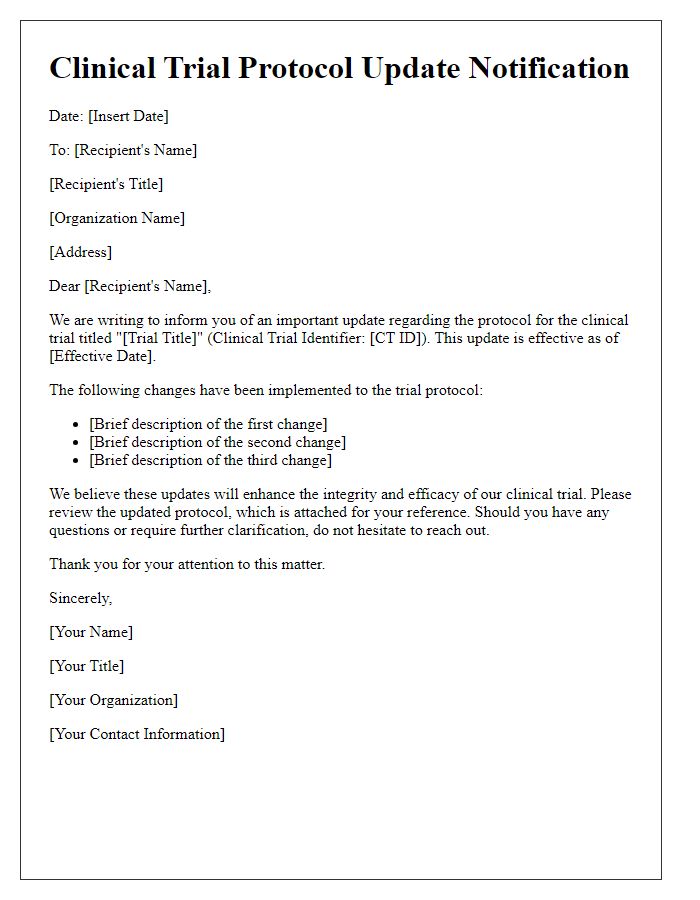
A clinical trial protocol amendment is crucial for aligning ongoing research with regulatory compliance requirements established by entities like the Food and Drug Administration (FDA) or the European Medicines Agency (EMA). This amendment process necessitates precise documentation of changes, ensuring adherence to Good Clinical Practice (GCP) guidelines and local health authority regulations. Key elements include updated study objectives, revised inclusion and exclusion criteria, modifications in treatment administration protocols, or alterations in data collection methods. Timely submission of these amendments, typically within 30 days of the decision to make changes, is critical to avoid potential delays in study progress. Furthermore, all stakeholders, including Institutional Review Boards (IRBs) and participating sites, must be notified promptly to maintain ethical standards and participant safety throughout the trial.
Amendment rationale and objectives
Clinical trial protocol amendments often arise from various factors impacting the study's execution and integrity. For instance, safety concerns identified in Phase III trials may necessitate adjustments to patient monitoring protocols. Modifications may also be driven by interim analysis results indicating a need to recalibrate treatment dosages. Additionally, regulatory agency feedback, such as from the FDA or EMA, may necessitate clearer eligibility criteria or expanded geographic locations for participant recruitment. Amendments aim to enhance data integrity, ensure participant safety, and maintain compliance with ethical standards while striving to achieve the primary and secondary objectives of the study, ultimately contributing to the advancement of medical knowledge.
Detailed protocol changes
A clinical trial protocol amendment details specific changes to research protocols, enhancing the overall study design and execution. This document highlights modifications in participant eligibility criteria, refining inclusion/exclusion parameters (e.g., age restrictions changed from 18-65 to 21-70 years). Changes in intervention protocols may include dosage adjustments (e.g., increasing dosage from 50mg to 75mg for better efficacy) or alterations in treatment duration. Data collection methods could also be revised, such as implementing digital tracking tools for patient adherence. Additionally, ethical considerations might necessitate updates to informed consent procedures, ensuring robust adherence to regulatory guidelines mandated by entities like the FDA or EMA. Finally, the amendment incorporates timelines for these changes, ensuring they align with project milestones and budgetary constraints for effective resource allocation.
Impact assessment on patient safety and data integrity
Clinical trial protocol amendments can significantly impact patient safety and data integrity. For instance, modifications to inclusion criteria might expose vulnerable populations to risk, particularly in trials involving novel therapies for conditions like cancer or cardiovascular diseases. Changes in dosages or treatment regimens must undergo rigorous evaluation to ensure they do not compromise patient safety. Additionally, alterations in data collection methods can introduce variability, affecting the reliability of results. Compliance with regulatory guidelines set forth by organizations such as the FDA (Food and Drug Administration) is imperative to uphold ethical standards and maintain the integrity of trial data. Moreover, the involvement of independent review boards is essential to assess potential risks associated with protocol changes, guaranteeing that patient welfare remains a top priority during the clinical trial process.
Sponsor and investigator signatures
The clinical trial protocol amendment requires the signatures of both the sponsor and the investigator to ensure compliance with regulatory standards and to validate changes. The sponsor, typically a pharmaceutical company or research organization, represents the entity funding and overseeing the trial, ensuring that all modifications align with the study's objectives and ethical guidelines. The investigator, a qualified medical professional at the clinical site, is responsible for conducting the trial while adhering to Good Clinical Practice (GCP) standards. Proper documentation of these signatures is crucial for maintaining trial integrity, facilitating audits, and enabling transparent communication with regulatory authorities such as the FDA (Food and Drug Administration) in the United States or EMA (European Medicines Agency) in Europe. These signatures serve as formal approval for the amendment, indicating both parties' agreement to the updated terms and conditions of the trial protocol.



Comments