Are you frustrated with a hospital stay that felt longer than necessary? You're not alone; many patients find themselves questioning the length of their stay and the billing that follows. In this article, we'll explore some common reasons for extended hospital stays, as well as the steps you can take to dispute unexpected charges. Stick around to discover how you can advocate for yourself and ensure you're not paying for unnecessary days in the hospital!

Patient Information Details
A hospital stay exceeding the expected duration can lead to increased medical costs and potential insurance disputes. Specific patient information, such as the name, date of birth, and medical record number, is essential for identifying the case. Relevant details about the hospital facility, including the name and address of the institution, along with the specific dates of admission and discharge, are crucial for context. The reasons for the extended stay should highlight medical complications, treatment delays, or unforeseen circumstances impacting recovery. Documentation of communication with healthcare providers, including discharge instructions and follow-up care plans, can strengthen the dispute. Overall, a comprehensive understanding of both patient and institutional details plays a vital role in effectively addressing the issue.
Medical Record and Treatment Summary
Length of hospital stays, typically ranging from 24 hours to several weeks, can significantly impact patient recovery and healthcare costs. The review of medical records, including treatment summaries, often reveals inconsistencies or errors in documented stay durations. For instance, a stay at St. John's Hospital in Los Angeles, California, might show a discharge date that does not align with recorded treatment procedures, such as post-operative recovery or ongoing therapies. Accurate records, including admission and discharge dates, along with notes on the patient's condition, are crucial for understanding the necessity of the hospital length. Discrepancies can lead to disputes regarding billing and insurance claims, requiring careful examination of all documentation to ensure that the patient's rights are protected and justified treatment timelines are maintained.
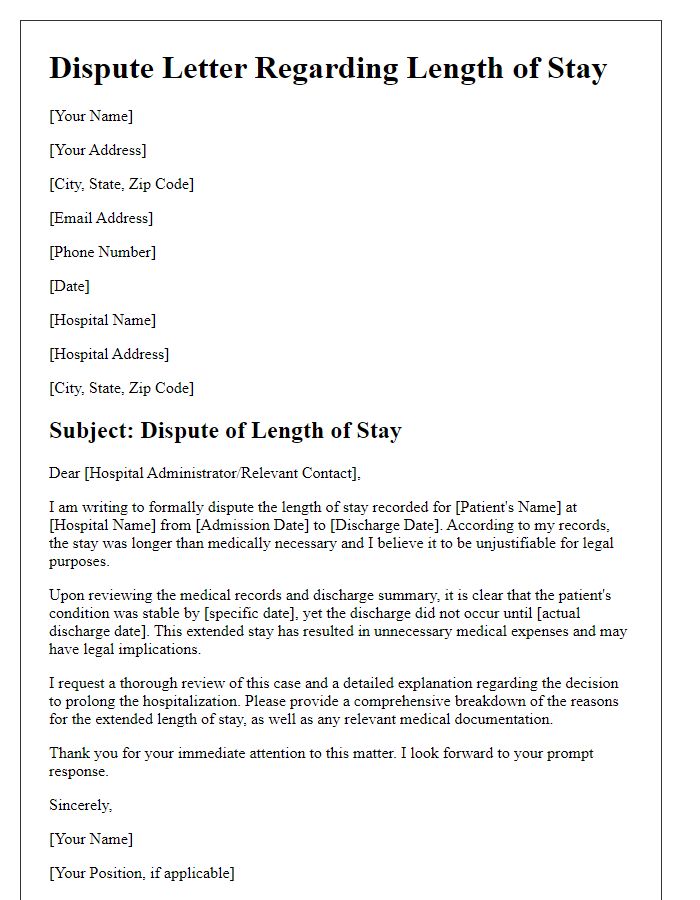
Specific Dispute Statement
Disputing the length of stay at hospitals can have significant implications for both financial responsibilities and patient care. A patient admitted to St. Mary's Medical Center in March 2023, for instance, had a documented stay of 10 days, which, according to diagnostic guidelines from the American Medical Association, exceeds the average duration for similar conditions, typically ranging from 3 to 5 days. In a review of medical necessity, it was found that diagnostic tests conducted, including MRI scans and X-rays, were performed within the first 48 hours. Furthermore, the post-discharge summary indicated no significant complications arose, suggesting a potential overextension of hospital resources. Clear documentation of treatment protocols and comparison of standard benchmarks can strengthen the dispute, potentially leading to adjustments in billing and healthcare assessments for the involved parties.
Supporting Evidence and Documentation
Hospital admissions can be subject to disputes regarding the length of stay, particularly in cases involving Medicare. Discrepancies may arise due to differing interpretations of medical necessity, which is defined as the necessity for treatment or services based on the patient's clinical condition. Hospital billing codes, including ICD-10 codes, detail the diagnosis that justifies the length of stay, and must align with the provided documentation. An example of this could be a patient diagnosed with pneumonia (ICD-10: J18.9), who requires a documented average of 3 to 5 days of observation. Essential supporting evidence includes physician notes that outline the clinical reasoning for care, nursing assessments to evaluate daily progress, and lab results confirming ongoing treatment necessity. The absence of cohesive and clear documentation can lead to prolonged disputes regarding proper billing and insurance reimbursements, ultimately impacting the financial responsibility of patients and healthcare facilities.
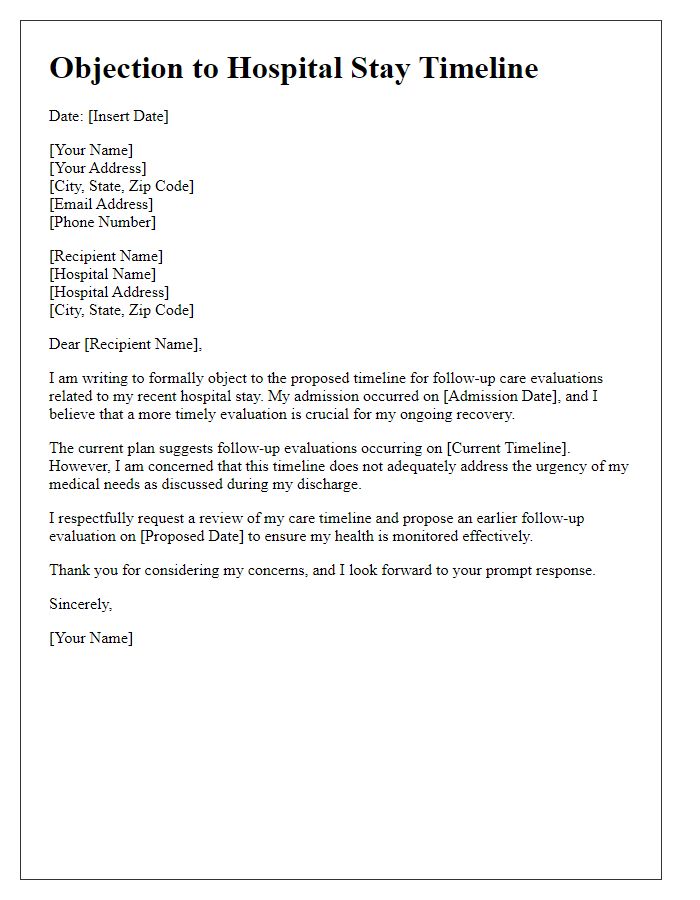
Request for Review and Resolution Timeline
A hospital stay length dispute often requires a thorough analysis of medical billing and treatment records. Patients may receive hospital bills after extensive stays, which can span days or even weeks at facilities like Johns Hopkins Hospital in Baltimore, Maryland. Insurance providers often set authorization limits, typically around 3 to 5 days for routine procedures. Disputes can arise when patients believe their medical needs warranted longer stays due to complications or additional treatments. Hospitals may utilize codes from the International Classification of Diseases (ICD) to justify charges. Patients should compile relevant documents, including discharge summaries and physician notes, to support their claims. Prompt requests for review within 30 days can expedite resolution, ensuring that all parties involved, including insurance representatives and hospital administrations, address the legitimate concerns regarding medical necessity and coverage.
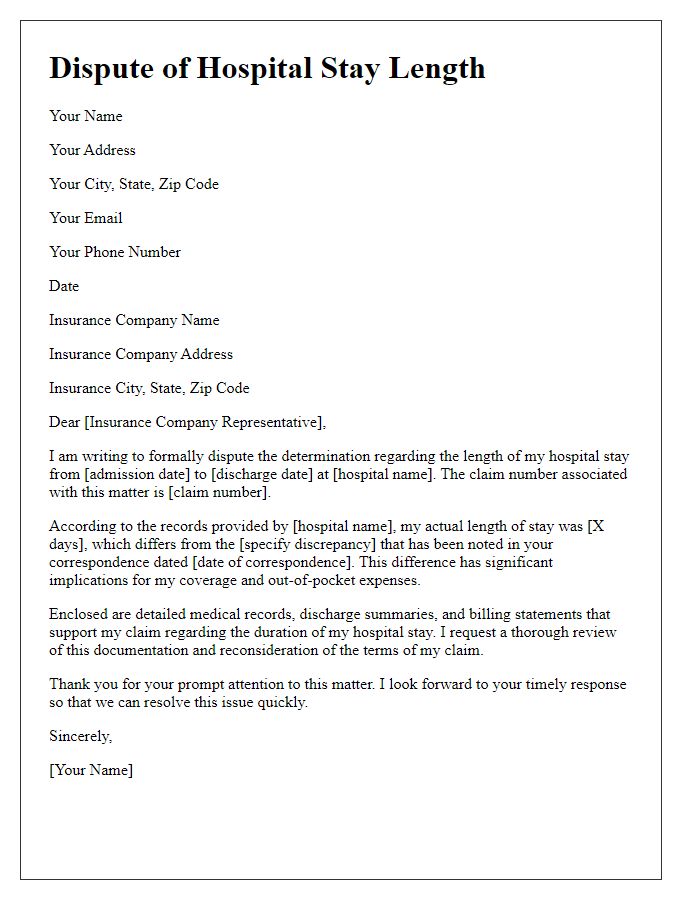
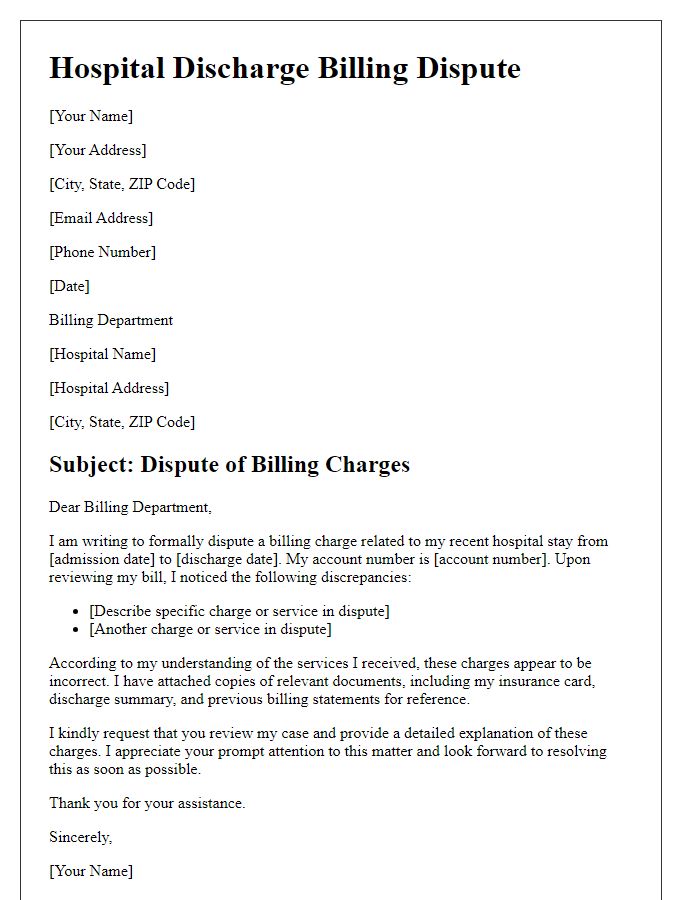
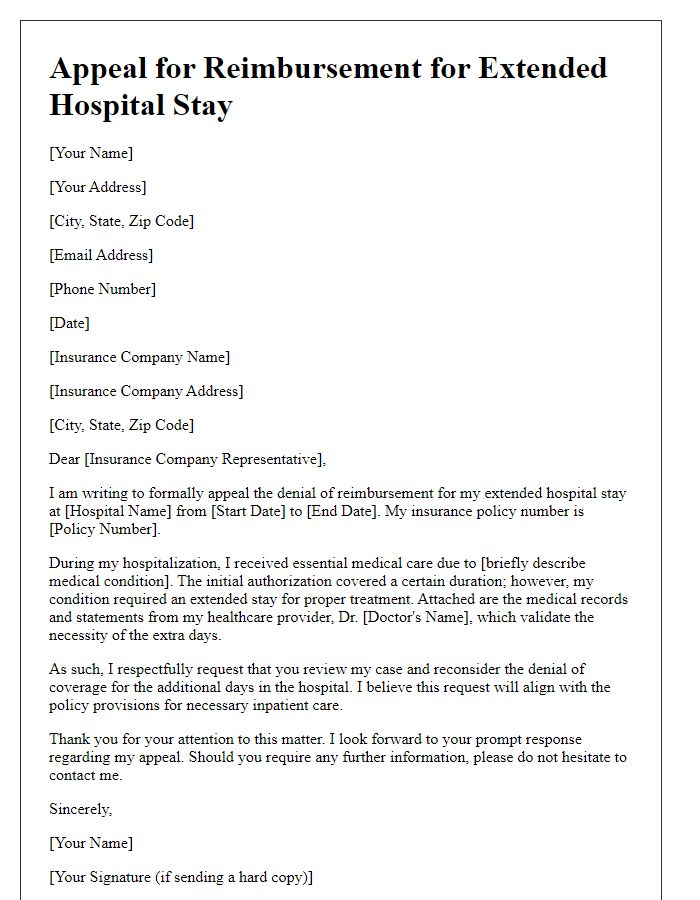
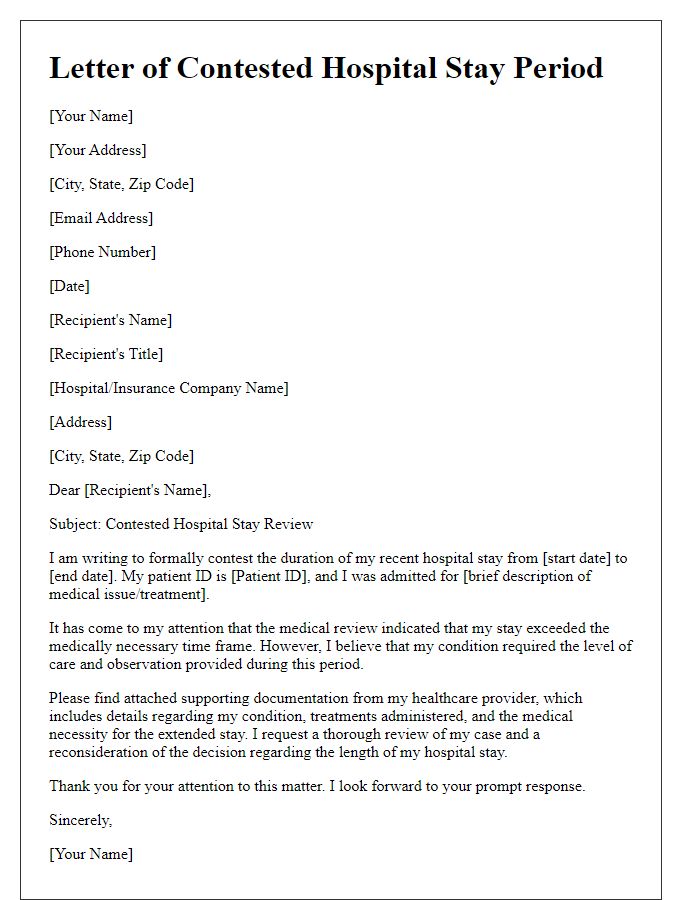
Letter Template For Disputing Hospital Stay Length Samples
Letter template of hospital visit duration disagreement for patient's records
Letter template of questioning hospital admission length for care comparison
Letter template of challenging hospital stay duration for policy clarification
Letter template of formal dispute regarding hospital stay duration for patient advocacy


Comments