Navigating the complexities of medical discharge can often feel overwhelming, especially when it comes to understanding your rights and responsibilities. Whether you're facing a transition from hospital to home care or moving to a rehabilitation facility, clear communication is key. This article aims to simplify the often confusing terms of medical discharge, ensuring that you feel informed and empowered throughout the process. So, grab a cup of tea and join us as we break down everything you need to know!
Patient Information and Identification
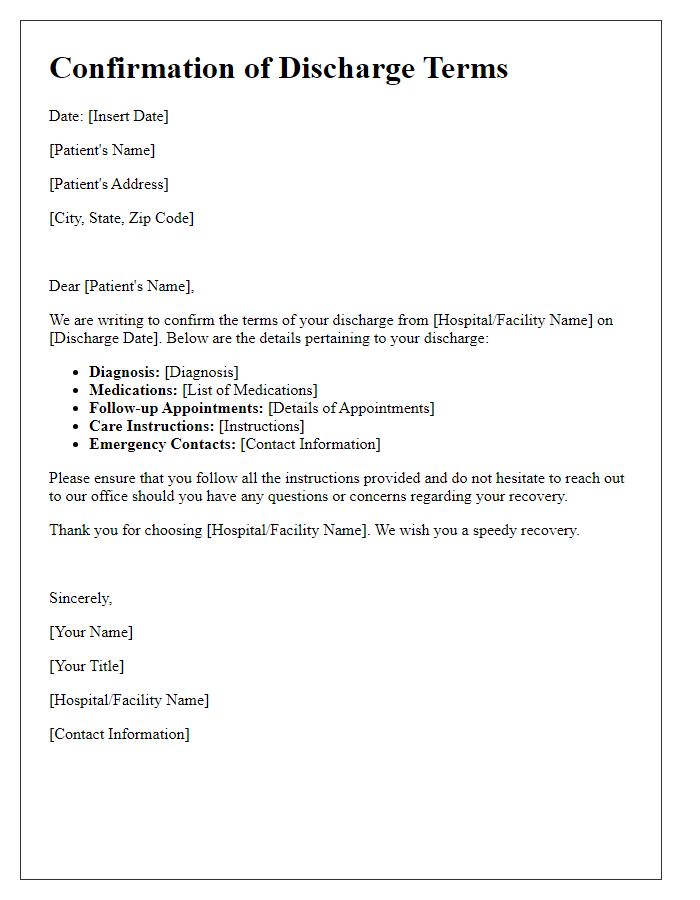
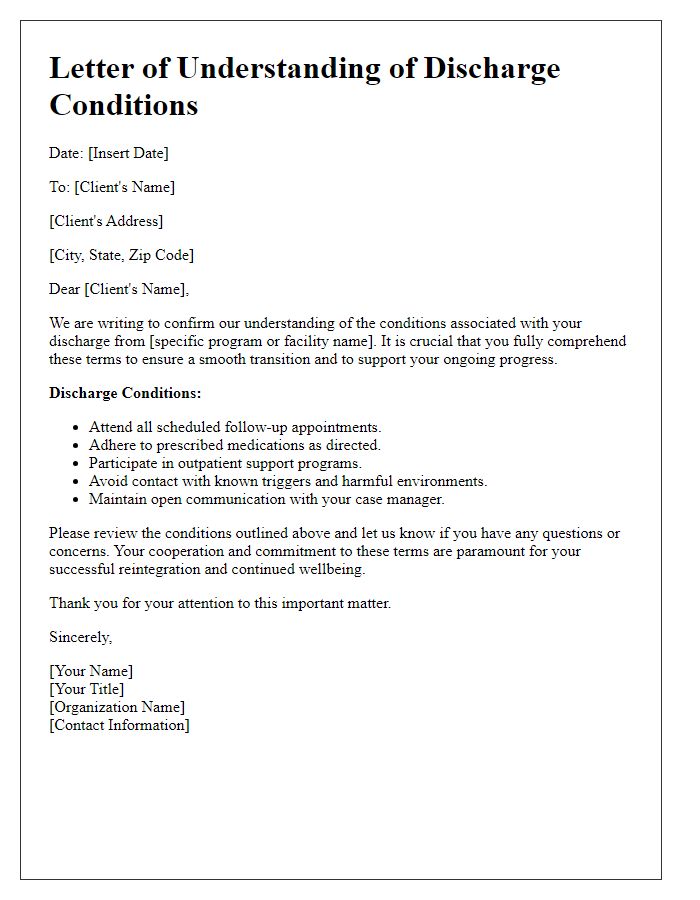
Patients undergoing medical treatment must have their discharge terms clearly defined to ensure a smooth transition to post-hospital care. Essential patient information, including full name (John Doe), date of birth (January 1, 1980), and medical record number (MRN: 123456789), identifies the individual accurately. Important details about the hospital stay, such as admission date (March 5, 2023) and discharge date (March 12, 2023), are crucial for tracking care progress. Additionally, understanding the diagnosis, treatment received, and any follow-up appointments scheduled (e.g., cardiology on March 19, 2023) helps outline the path for recovery. Specific instructions regarding medication (e.g., dosage of Metoprolol 50 mg), activity restrictions (e.g., avoid heavy lifting for two weeks), and signs of complications requiring immediate attention are vital for ensuring patient safety and efficacy of post-discharge care.
Discharge Date and Summary
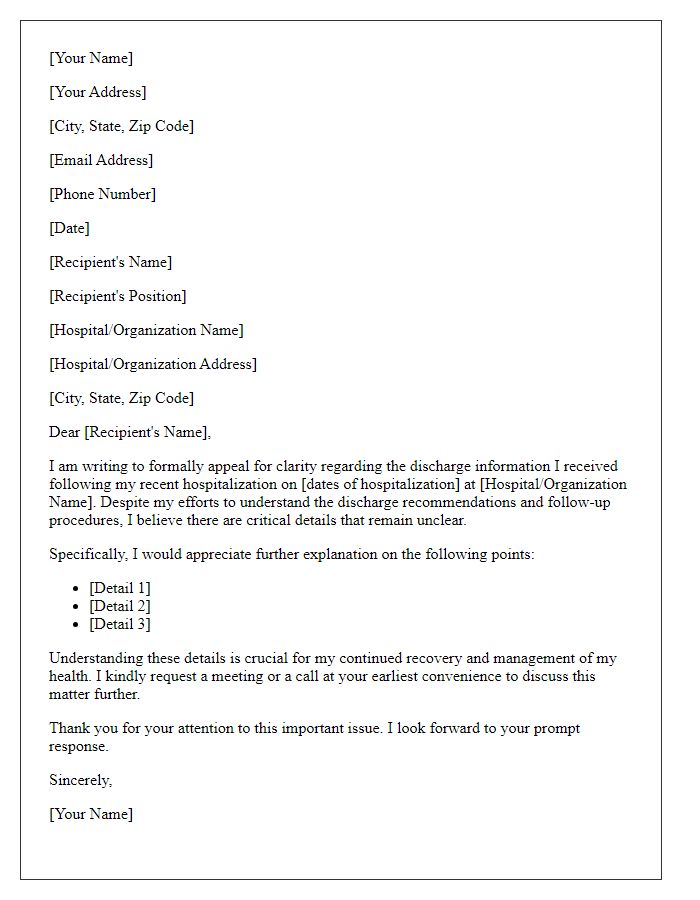
Medical discharge from a healthcare facility marks the end of a patient's inpatient care, often around day 3 to 7 of hospitalization, depending on the condition. A discharge summary, typically generated by the healthcare professional overseeing the patient's recovery, outlines key details regarding the patient's diagnosis, treatment received, medications prescribed, follow-up appointments, and instructions for home care. It serves as a crucial document for ongoing medical management, ensuring seamless transition into outpatient care. Accurate documentation is essential, with patients advised to keep track of their discharge date, any specific outcomes of treatment, and follow-up plans, to maintain continuity in their healthcare journey.
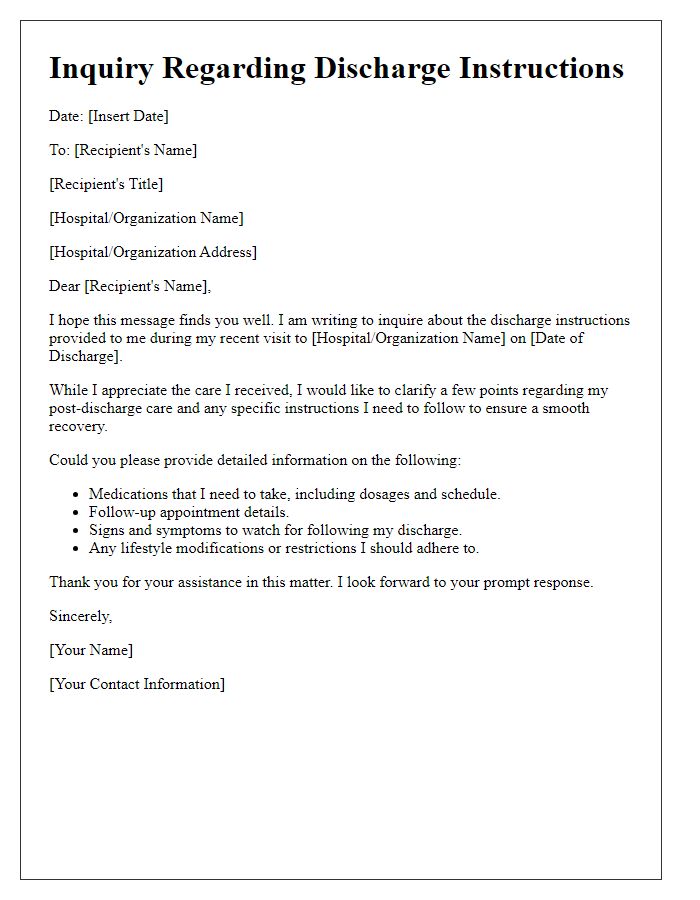
Medication Instructions and Dosage
Medical discharge presents critical information regarding medication instructions and dosage for patients. Clear guidelines regarding prescription medications, such as Dosage (specific milligrams) and Frequency (times per day), are essential to ensure patient compliance. Each medication, including Antibiotics (like Amoxicillin), may have specific administration requirements, such as taking with food or avoiding dairy products. Medication interactions must be highlighted, particularly if patients are prescribed multiple medications, such as Pain Relievers (like Ibuprofen) alongside Antidepressants (like Sertraline). Additionally, Refills might be necessary for chronic conditions, emphasizing the importance of following up with healthcare providers, such as Primary Care Physicians. Instructions should also address possible Side Effects, like dizziness or nausea, ensuring patients understand what to monitor post-discharge. Following these guidelines significantly contributes to successful recovery and minimizes complications.
Follow-up Appointments and Referrals
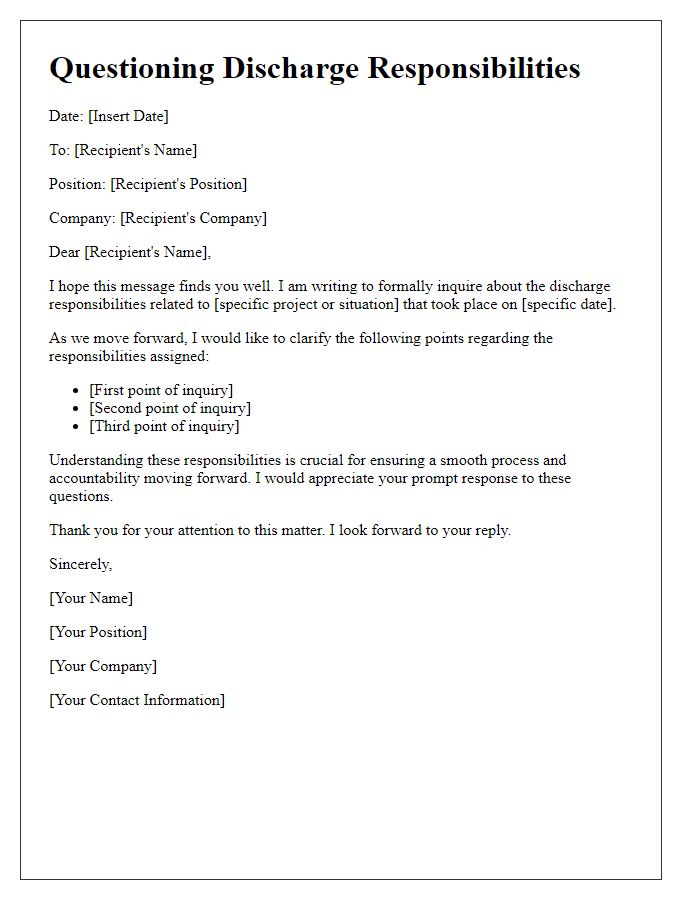
Medical discharge procedures often require clear communication regarding follow-up appointments and necessary referrals. Healthcare providers typically outline the recommended timetable for follow-ups, which may include specific dates (e.g., two weeks post-discharge) for assessments of recovery progress. Referrals to specialized practitioners, such as a cardiologist or physical therapist, can also be essential in ensuring comprehensive post-treatment care. Documentation provided to patients should include vital information about appointments, including location details such as the facility name (e.g., Community Health Center), appointment numbers, and any preparatory instructions (e.g., fasting prior to blood work). This clarity helps patients understand their responsibilities while promoting better health outcomes.
Emergency Contact Information and Guidelines
Emergency contact information plays a crucial role in ensuring continuity of care after a medical discharge from healthcare facilities such as hospitals or rehabilitation centers. Patients receiving discharge instructions must list relevant contacts, including family members or caregivers, who can be reached in case of complications or emergencies. Guidelines for post-discharge care should include clear instructions on medication management, follow-up appointments, and signs of potential distress. Specific recommendations might emphasize the importance of keeping emergency numbers, such as local hospitals or urgent care centers, easily accessible. Educational materials should also emphasize the need for reaching out to healthcare providers for non-urgent questions or concerns during recovery, ensuring a smooth transition from hospital to home.

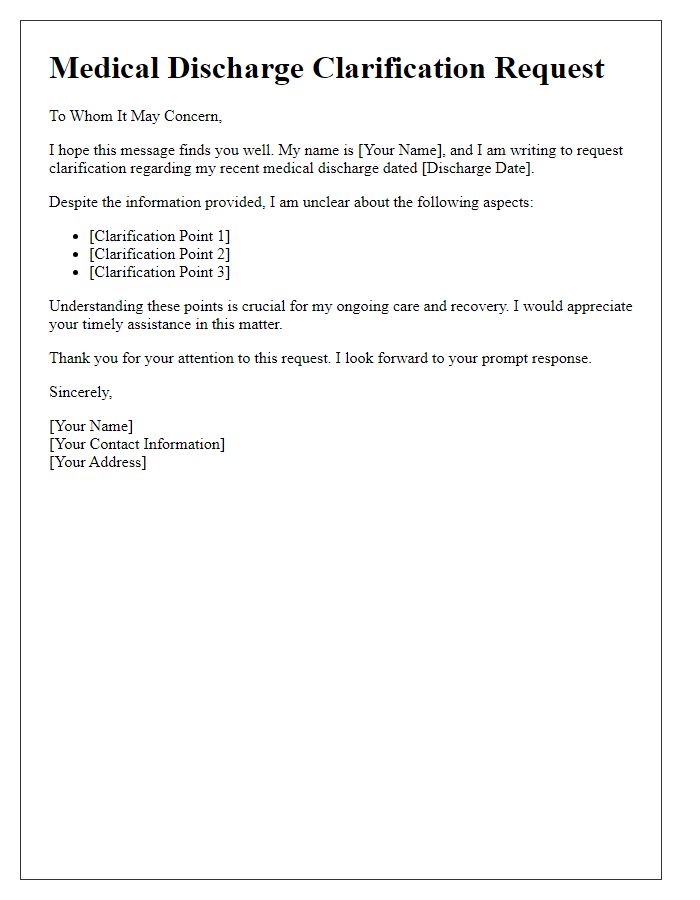

Comments