Navigating the whirlwind of an emergency room visit can be overwhelming, but a well-crafted letter can help ease communication during such stressful times. In this article, we'll explore a simple letter template that can assist patients and their families in conveying important information to medical staff. Whether it's outlining medical history, allergies, or specific concerns, having a clear structure can make a significant difference in the care received. So, let's dive in and discover how you can create an effective emergency room letter that ensures your voice is heard!
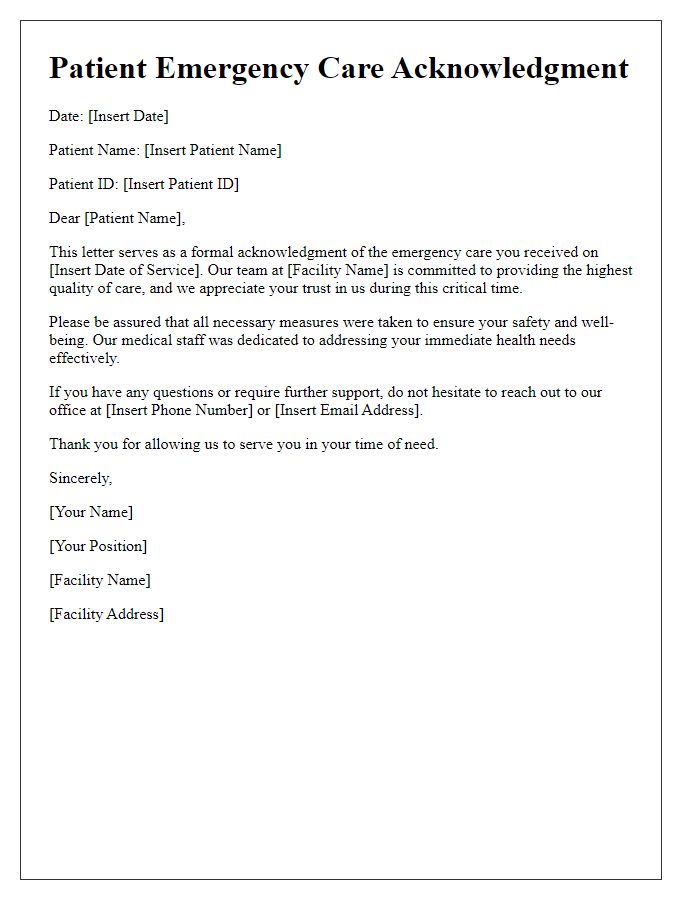
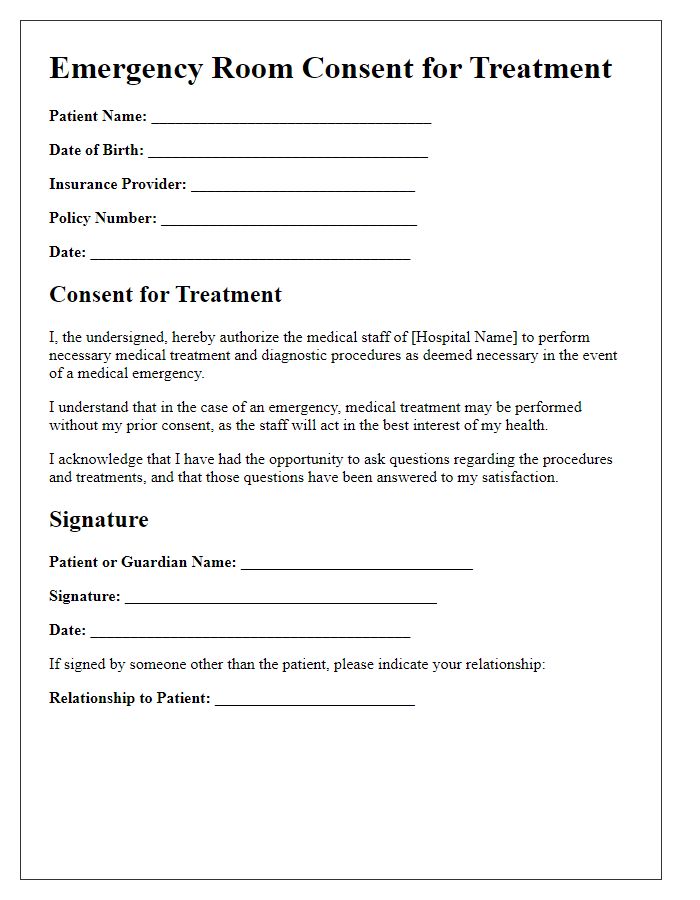
Patient Identification and Information
Emergency room visits often require timely and accurate patient identification to ensure proper care. Patient identification is critical, involving details such as name, date of birth (DOB), and unique medical record number (MRN), ensuring a match with personnel and electronic health records (EHR). Additional information may include contact details and insurance information, which facilitate the billing process and provide critical coverage details during urgent care events. It is essential for healthcare providers at facilities like Northside Hospital in Atlanta, Georgia, to collect this information swiftly; hastening treatment for conditions such as chest pain or severe trauma can significantly affect patient outcomes. Accurate identification prevents medication errors, saves time, and enhances the overall efficiency of emergency medical services (EMS).
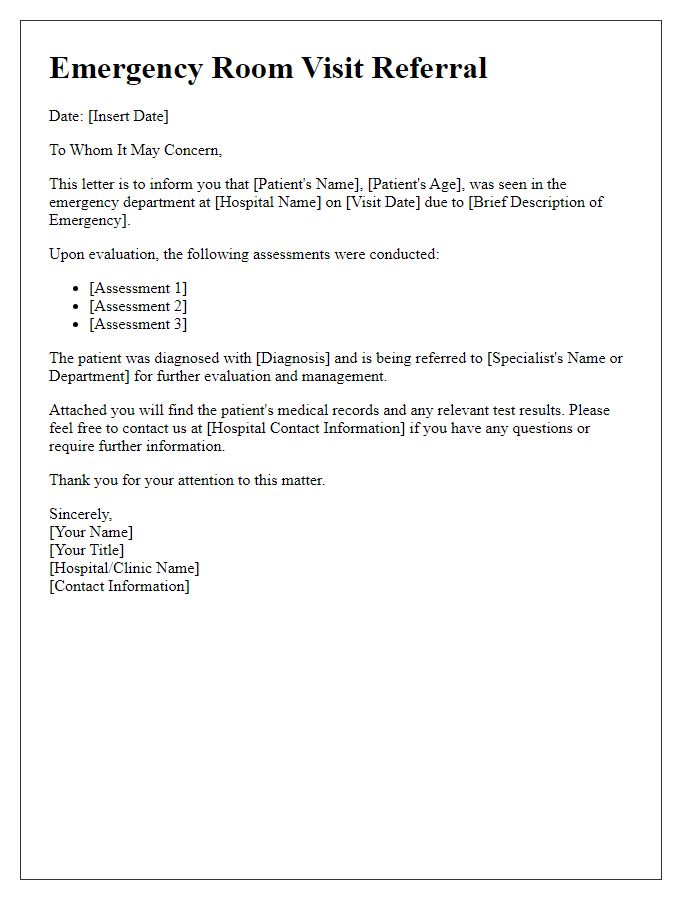
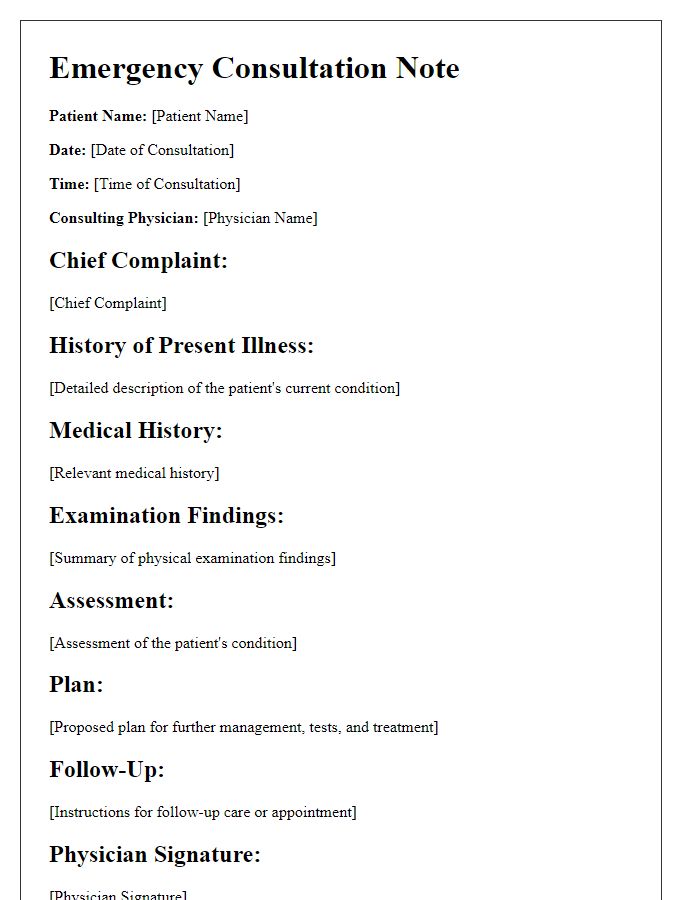
Visit Details and Reason for Visit
During the emergency room visit on October 15, 2023, at City General Hospital in New York, the patient, a 32-year-old female, presented with acute abdominal pain characterized by sharp cramps and nausea. Vital signs indicated a temperature of 101 degrees Fahrenheit and a heart rate of 110 beats per minute, suggesting a possible infection. Laboratory tests, including a complete blood count and metabolic panel, were performed to assess for underlying conditions such as appendicitis or bowel obstruction. The emergency medical team administered intravenous fluids and pain relief medication to stabilize the patient while awaiting the results of imaging studies, specifically an abdominal ultrasound, to determine the precise cause of the symptoms.
Medical History and Current Medications
During an emergency room visit, detailed medical history is crucial for effective patient care. Patients should provide information about past illnesses, surgeries, and significant family health conditions such as diabetes or heart disease. Additionally, listing current medications, including over-the-counter drugs and supplements, is essential for preventing potential drug interactions. Patients should note allergy reactions to specific medications, as this can drastically alter treatment options. Furthermore, the emergency medical staff should be informed about chronic health conditions like hypertension or asthma, as these may influence the diagnosis and treatment plan. Accurate information ensures timely interventions and enhances patient safety in critical situations.
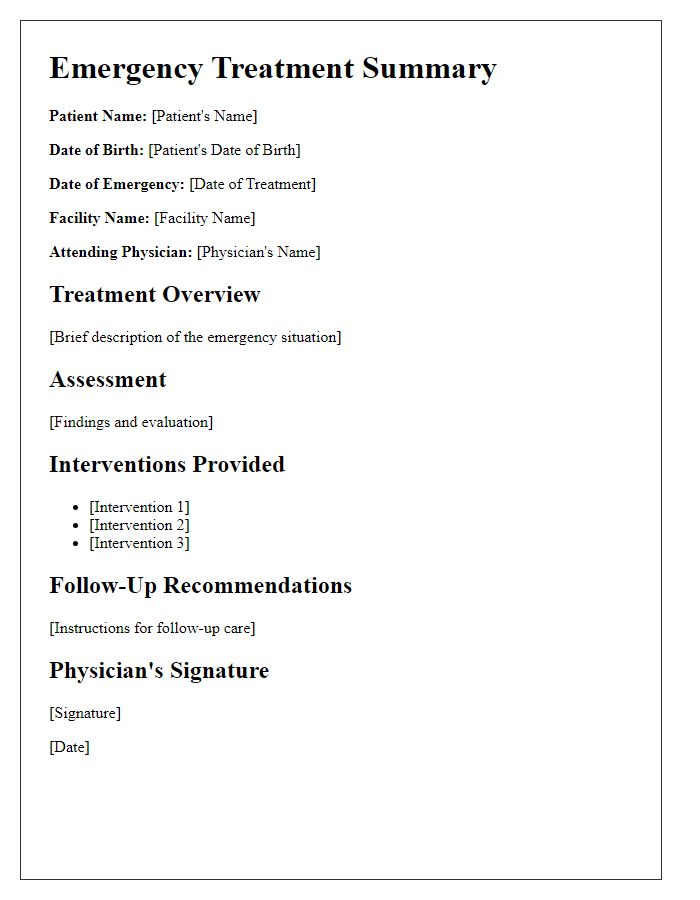
Diagnosis and Treatment Provided
Patients visiting the emergency room often receive a diagnosis and treatment related to acute medical conditions. Common diagnoses may include fractures, pneumonia, or cardiac events such as myocardial infarction, with incident rates varying by region. For example, pneumonia affects approximately 5 million people annually in the United States. Treatments can include intravenous antibiotics administered in cases of infection, casting for fractures, or immediate interventions such as defibrillation for cardiac arrest scenarios. Emergency departments, such as those at hospitals like Mount Sinai or Johns Hopkins, are equipped with advanced imaging technology, like CT scanners, to assist in diagnosing conditions swiftly. Furthermore, the multidisciplinary team involved in patient care may consist of emergency physicians, nurses, radiologists, and pharmacists, all pivotal in ensuring effective treatment and patient outcomes.
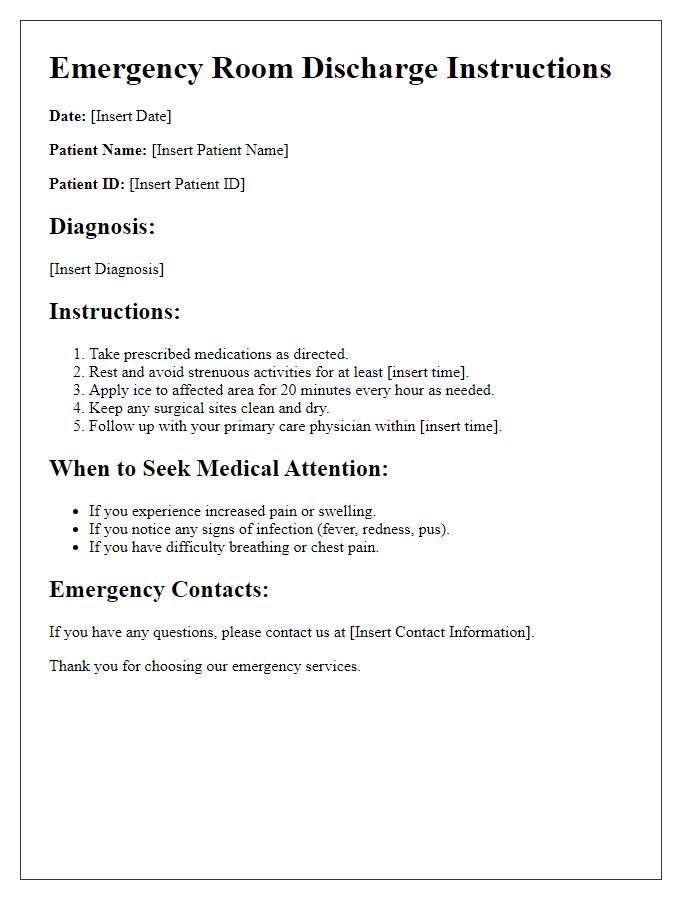
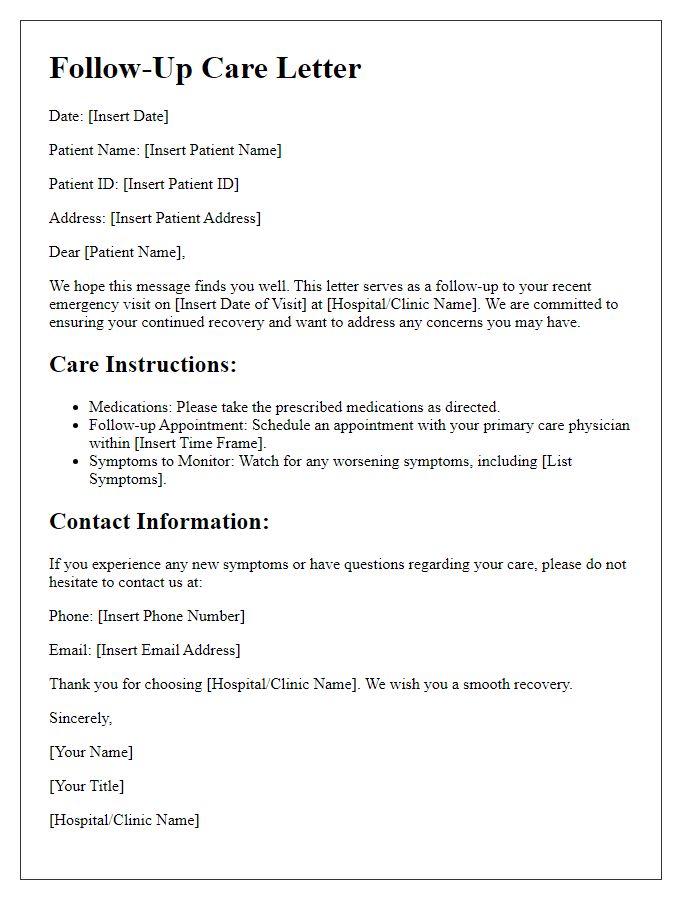
Follow-up Instructions and Emergency Contact Information
Follow-up instructions after an emergency room visit are crucial for ensuring ongoing health care management. Patients should schedule follow-up appointments within the next week with their primary care physician (PCP) to discuss test results and recovery plans, particularly if they received treatments such as stitches or medications. Instructions may include monitoring symptoms, taking prescribed medications (such as antibiotics), and following up on any referrals to specialists, like orthopedic surgeons for fractures. Emergency contact information should feature local urgent care clinics and the nearest hospital (e.g., City Hospital, contact number: 555-1234) in case of worsening symptoms or new concerns. It's essential to keep this information accessible, particularly for those managing chronic conditions or experiencing complications.


Comments