Are you seeking a streamlined way to refer patients to a rheumatology clinic? Crafting a well-structured referral letter can make all the difference in ensuring your patients receive the specialized care they need. In this article, we'll explore essential elements to include in your referral letter, such as patient history, clinical findings, and relevant tests. Read on to discover the best practices for writing an effective referral that enhances patient outcomes!
Patient's medical history and symptoms
A comprehensive referral for a rheumatology clinic involves detailing the patient's medical history and presenting symptoms. This may include a description of conditions such as osteoarthritis (a degenerative joint disease characterized by cartilage breakdown), rheumatoid arthritis (an autoimmune disorder causing joint inflammation), or lupus (a systemic autoimmune disease). Notable symptoms may involve joint pain (often persisting for over six weeks), stiffness (especially in the morning lasting more than 30 minutes), swelling in areas such as hands and knees, fatigue (fatigue levels rated on a scale of 1-10), and skin rashes (common in conditions like systemic lupus erythematosus). Past medical history should specify any previous diagnoses, treatments (like corticosteroids or DMARDs), relevant family history (such as genetic predispositions), and any laboratory results (like elevated ESR or CRP values indicating inflammation). Details such as the patient's age, sex, occupation, and lifestyle habits (including smoking or physical activity level) can provide additional context for the referral evaluation.
Relevant test results and diagnostics
A rheumatology clinic referral typically includes several relevant test results and diagnostics linked to autoimmune diseases and musculoskeletal disorders. Blood tests, such as Antinuclear Antibody (ANA) test, Rheumatoid Factor (RF), and Erythrocyte Sedimentation Rate (ESR), provide insight into inflammation levels and the autoimmune profile of the patient. Imaging studies, including X-rays, MRI scans, and ultrasounds, reveal joint damage or synovial thickening characteristic of conditions like rheumatoid arthritis or lupus. Comprehensive assessments of functional abilities and physical examinations highlight any swelling, pain points, or reduced range of motion in joints, aiding rheumatologists in diagnosing and formulating treatment plans effectively. Keeping a detailed record of symptoms, family medical history, and prior diagnoses enhances the accuracy of the referral process.
Current medications and treatments
Current medications for rheumatology patients often include Disease-Modifying Antirheumatic Drugs (DMARDs) such as Methotrexate, typically prescribed to manage rheumatoid arthritis (RA). Patients may also be on Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) like Ibuprofen, utilized for pain relief and inflammation reduction. Corticosteroids, such as Prednisone, are frequently administered in varying dosages to control severe flares. Biologic agents, including Tumor Necrosis Factor inhibitors like Etanercept, may be indicated for refractory cases. It's essential to monitor the patient's treatment adherence and response, adjusting therapy accordingly for optimal disease management and minimizing potential adverse effects. Regular lab work, including Complete Blood Count (CBC) and liver function tests, should be conducted to assess the safety and efficacy of ongoing treatments.
Specific concerns or suspected conditions
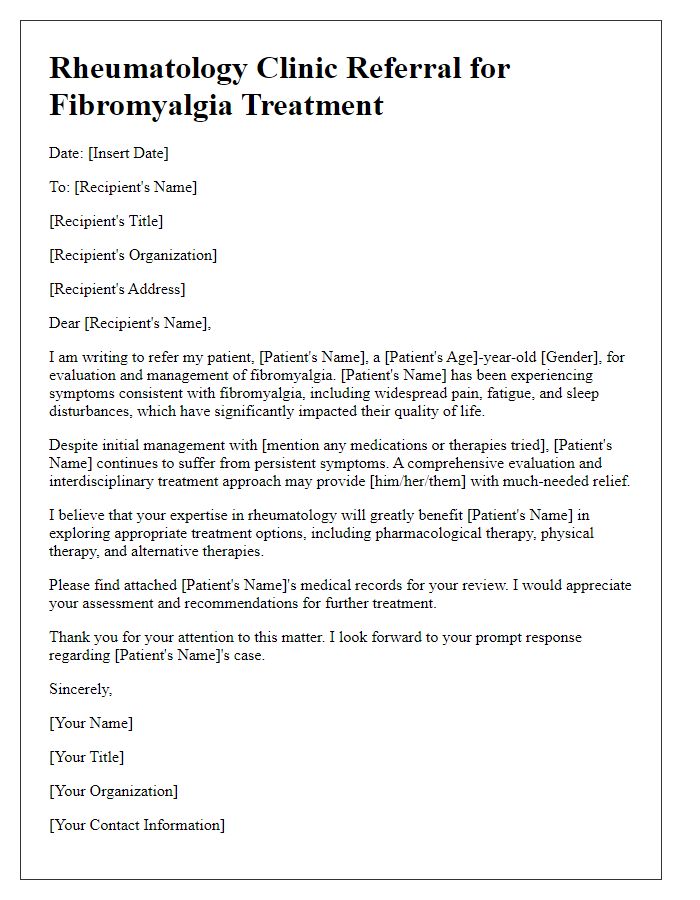
The rheumatology clinic referral process encompasses various specific concerns and suspected conditions, including autoimmune diseases like rheumatoid arthritis (characterized by joint inflammation affecting approximately 1% of the global population), systemic lupus erythematosus (an autoimmune disease impacting various body systems, with a prevalence rate of about 20 to 150 cases per 100,000 individuals), and psoriatic arthritis (associated with the skin condition psoriasis, affecting about 30% of patients with psoriasis). Physicians may also suspect conditions like fibromyalgia (a chronic disorder causing widespread musculoskeletal pain, with estimates suggesting it affects around 2% to 8% of the population), ankylosing spondylitis (a form of arthritis primarily affecting the spine, affecting approximately 0.1% to 0.5% of the population), or gout (a type of arthritis due to excess uric acid, affecting nearly 4% of U.S. adults). Comprehensive assessments including laboratory tests, imaging studies, and clinical evaluations are essential for accurate diagnosis and effective management of these rheumatologic concerns.
Provider's contact information and credentials
Contact information for the rheumatology clinic includes the clinic's name, address, phone number, and email. Credentials entail the medical education, board certifications, and relevant experience of the referring provider. The clinic typically has specialists with training in diagnosing and treating autoimmune disorders like rheumatoid arthritis and lupus, ensuring patients receive comprehensive care. Communication forms may include secure fax numbers or encrypted email for sending patients' medical records, including lab results, imaging studies, and medication history, which are crucial for effective evaluation by the rheumatology team.
Letter Template For Rheumatology Clinic Referral Samples
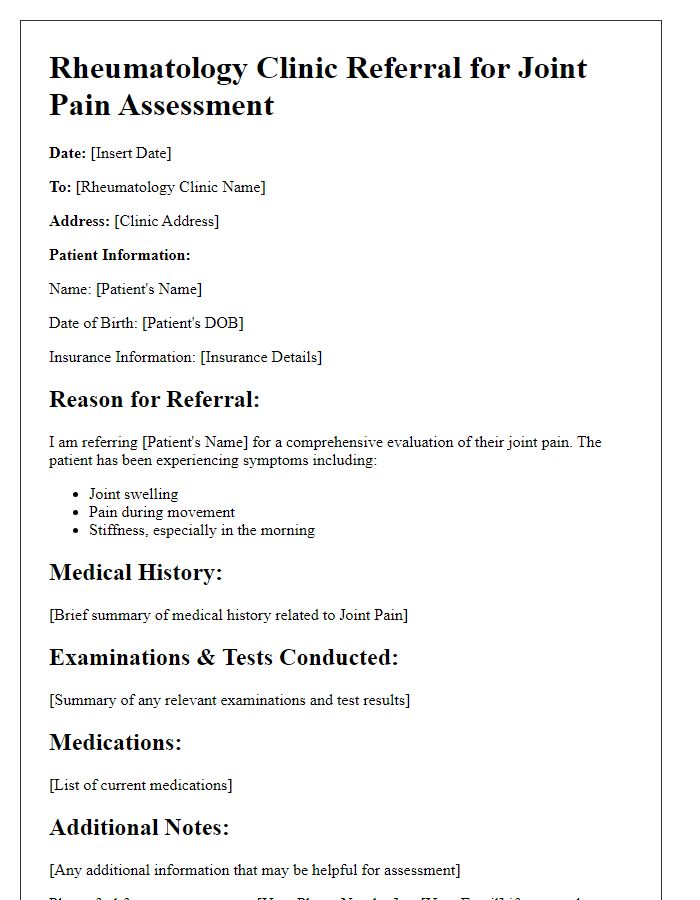
Letter template of rheumatology clinic referral for joint pain assessment.
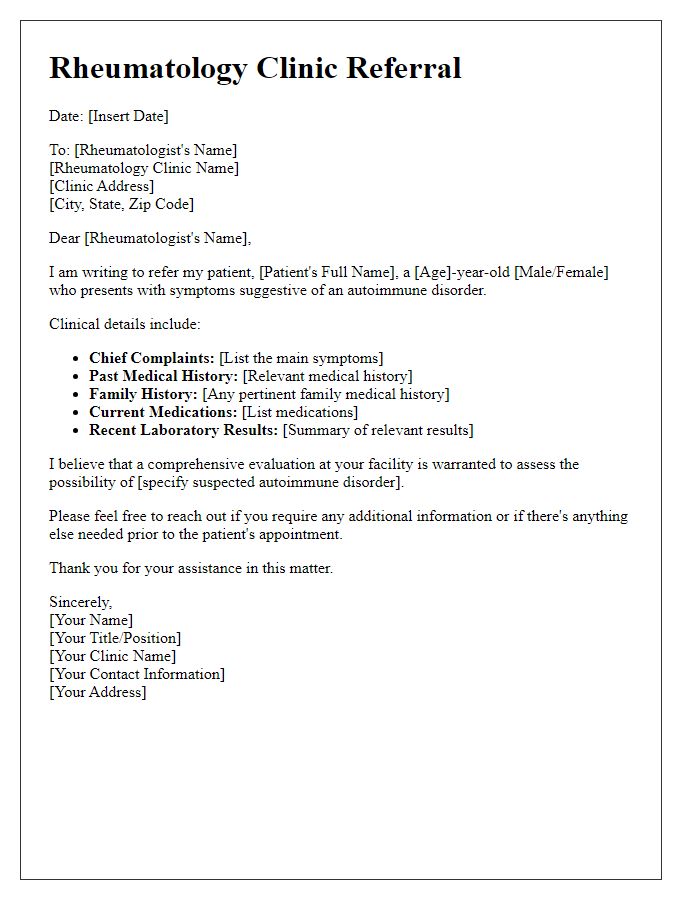
Letter template of rheumatology clinic referral for autoimmune disorder evaluation.
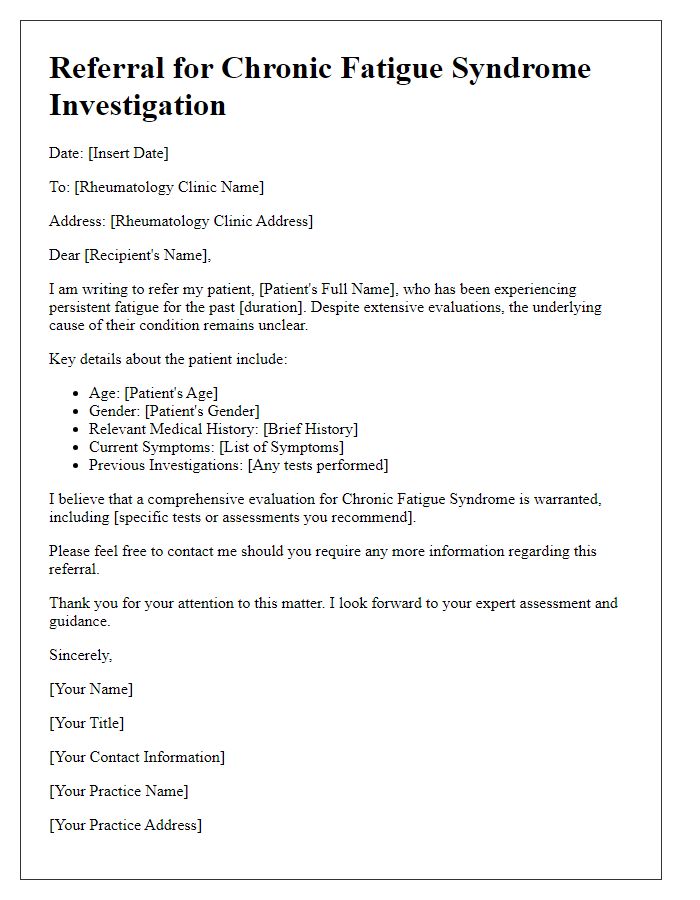
Letter template of rheumatology clinic referral for chronic fatigue syndrome investigation.
Letter template of rheumatology clinic referral for suspected lupus diagnosis.
Letter template of rheumatology clinic referral for arthritis management plan.
Letter template of rheumatology clinic referral for follow-up on inflammatory markers.
Letter template of rheumatology clinic referral for systemic sclerosis assessment.
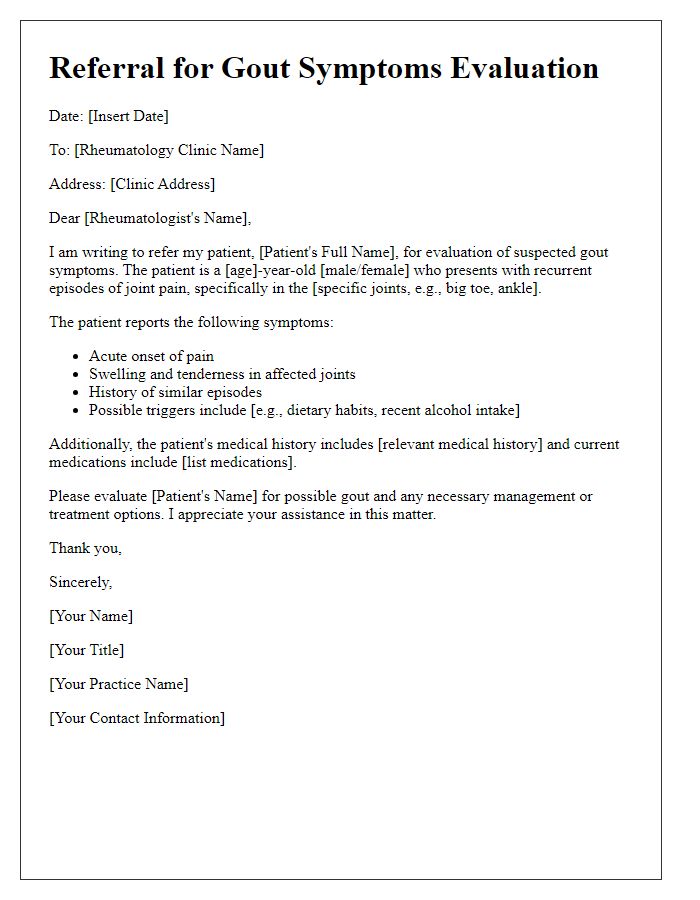
Letter template of rheumatology clinic referral for gout symptoms evaluation.
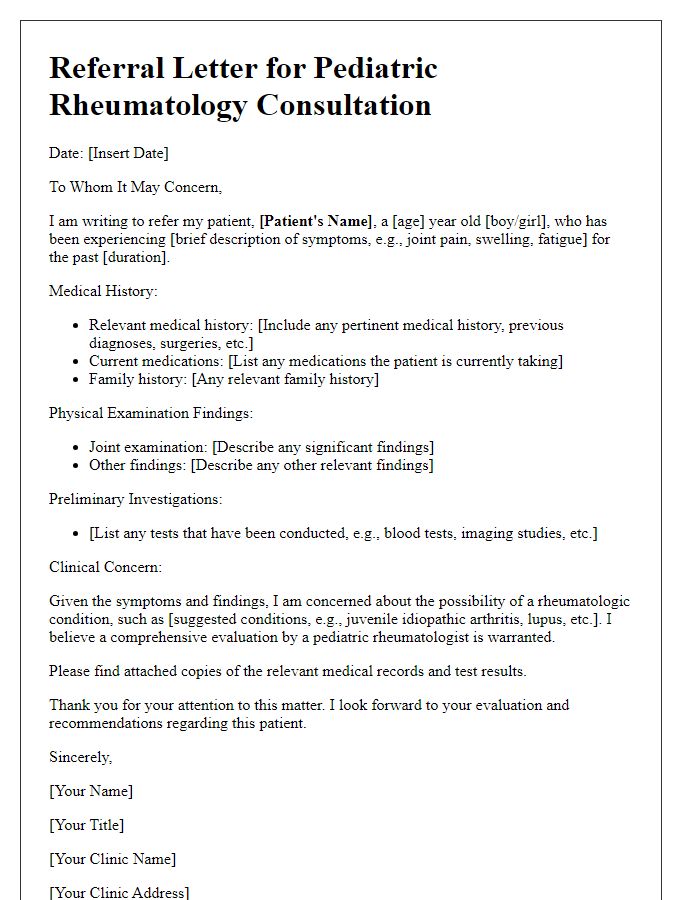
Letter template of rheumatology clinic referral for pediatric rheumatology consultation.


Comments