When a loved one is discharged from the hospital, receiving a comprehensive discharge summary is essential for a smooth transition home. This document not only outlines the patient's medical history and treatment received but also provides clear instructions for ongoing care and follow-up appointments. It serves as a crucial communication tool between healthcare providers and caregivers, ensuring everyone stays informed about the patient's needs. Curious to learn how to create an effective discharge summary or what key elements to include? Read on!
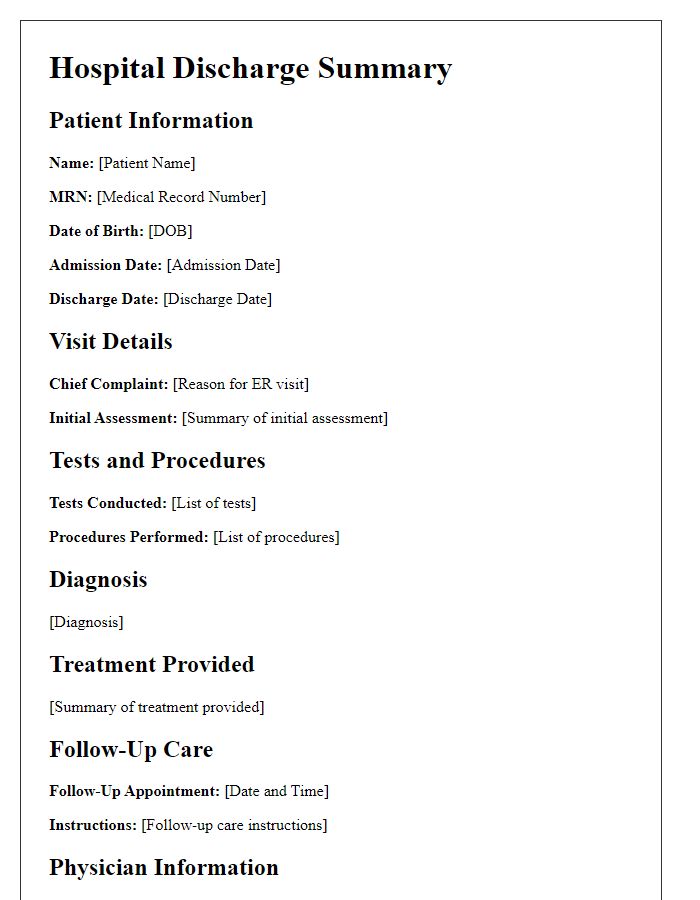
Patient Information
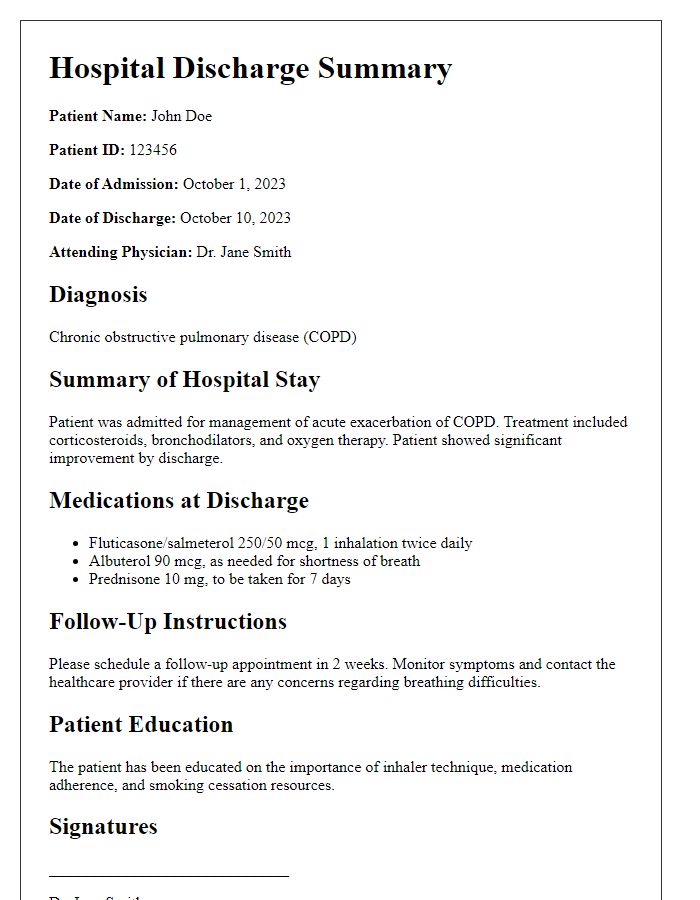
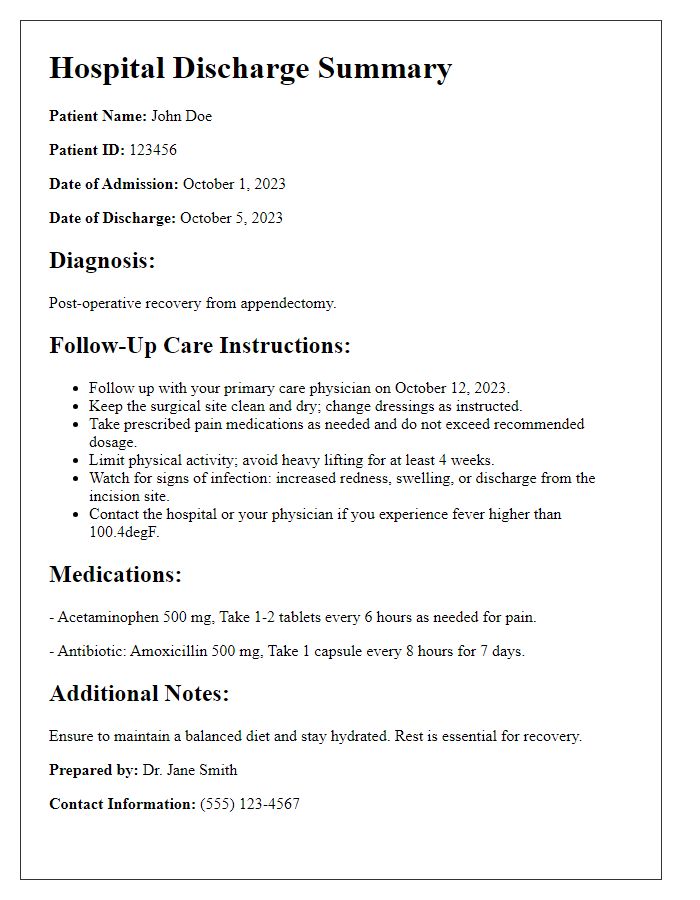
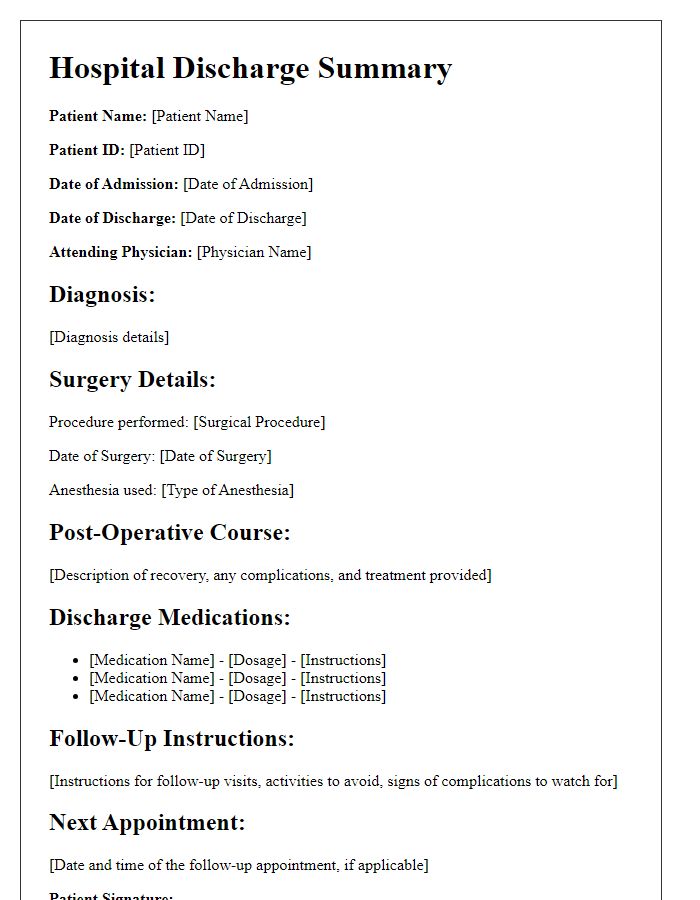
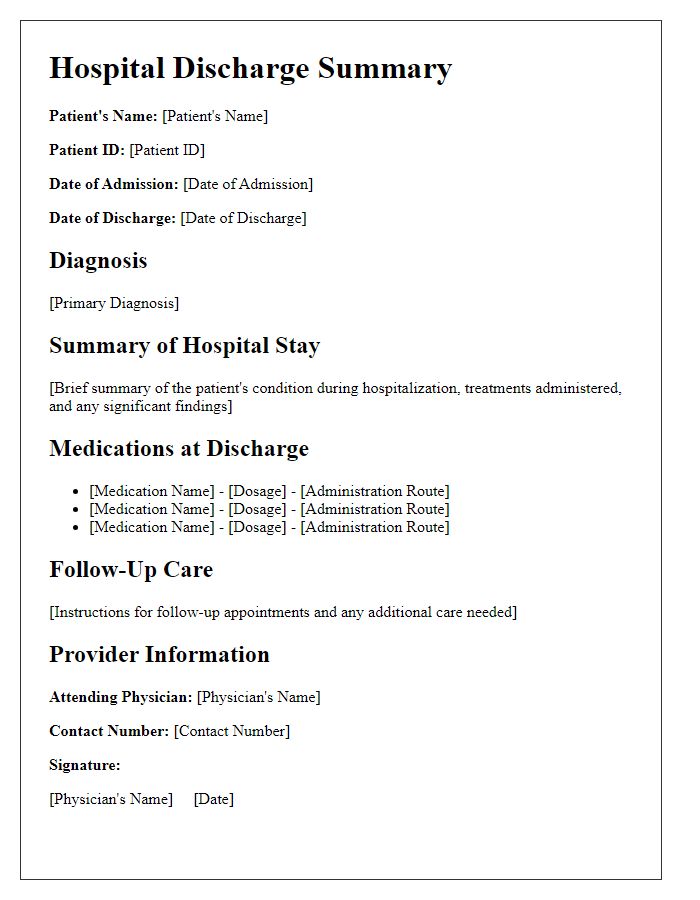
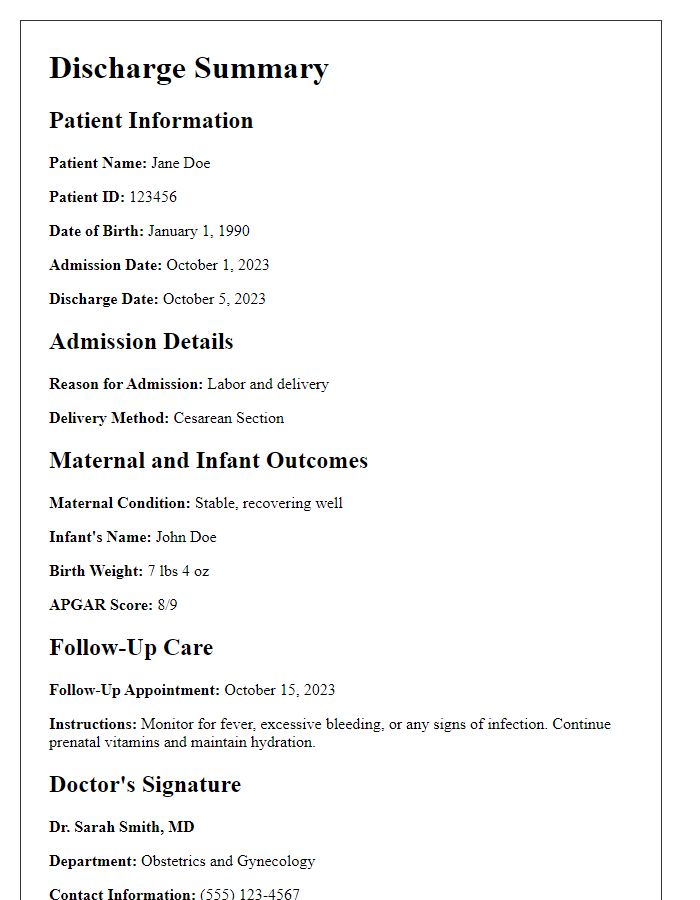
The hospital discharge summary is an essential document that provides detailed information regarding a patient's stay and treatment at a healthcare facility. This summary typically includes critical patient information such as full name (John Smith), date of birth (January 15, 1980), medical record number (123456), and admission date (October 1, 2023), highlighting the time spent in the facility. The attending physician (Dr. Emily Johnson) and the healthcare team members involved in the patient's care are also noted, along with any relevant contact information for follow-up appointments. Additionally, the discharge summary outlines the primary diagnosis (pneumonia), secondary conditions (asthma), and any procedures performed (bronchoscopy on October 3, 2023), ensuring a comprehensive overview for future healthcare providers. This structured information is vital for continuity of care, medication management, and ongoing health tracking, allowing seamless transitions from hospital to home.
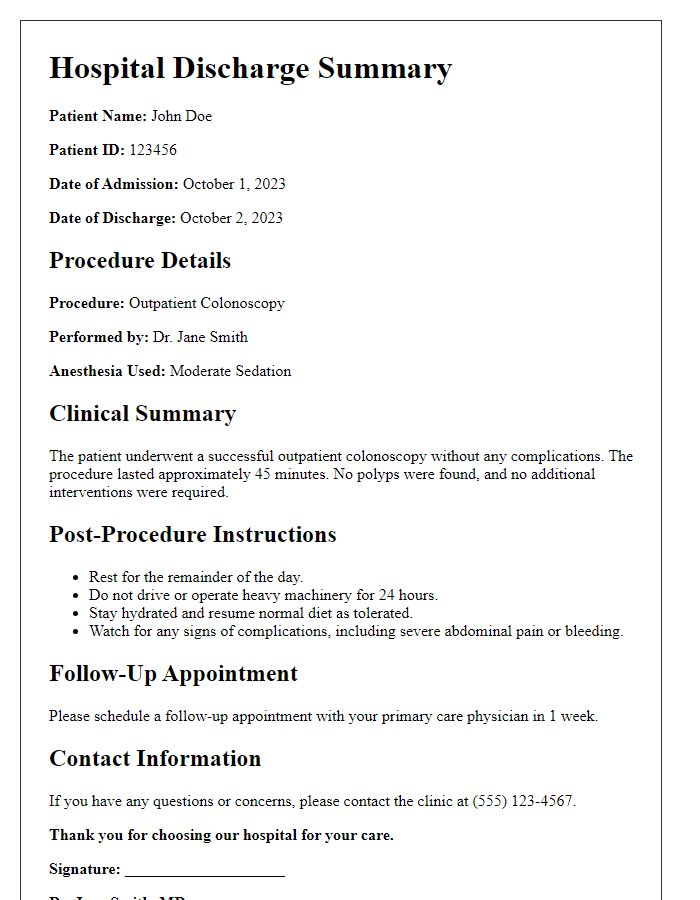
Admission and Discharge Dates
The patient's hospital admission occurred on March 1, 2023, where they were treated for pneumonia at City General Hospital, a facility known for its comprehensive respiratory care. The discharge was successfully completed on March 10, 2023, marking a nine-day hospitalization. The discharge summary provides a detailed account of the patient's progress during their stay, including vital signs, treatment administered, and follow-up care necessary to ensure optimal recovery post-discharge. The summary plays a crucial role in coordinating care with outpatient providers and facilitating a smooth transition home for the patient.
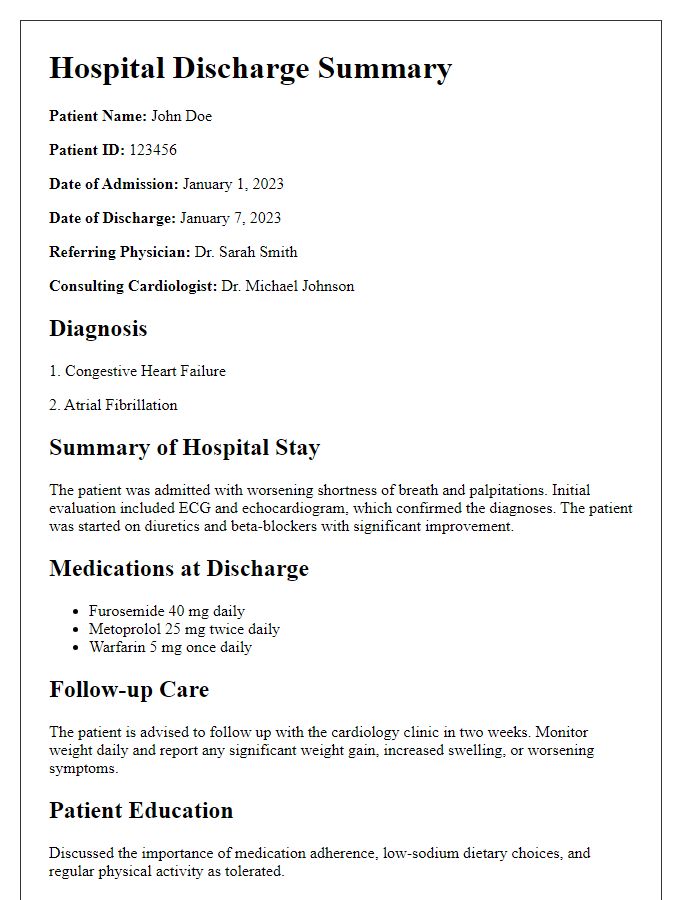
Diagnosis and Treatment Summary
The hospital discharge summary provides a concise overview of the patient's diagnosis and treatment received during their inpatient stay. The primary diagnosis, such as pneumonia (a lung infection characterized by inflammation), was confirmed through a combination of clinical evaluation and chest X-ray results. Treatment involved a course of intravenous antibiotics, specifically Ceftriaxone, delivered over seven days to combat the infection effectively. Additionally, supportive measures included oxygen therapy to maintain optimal blood oxygen levels above 92%. Follow-up appointments were scheduled with the pulmonology department (specializing in respiratory tract diseases) within two weeks post-discharge to monitor recovery progress and ensure no complications arise. Health education on medication adherence and symptoms to monitor was provided to the patient upon discharge.
Medications and Prescriptions
Patients, upon hospital discharge, often require a comprehensive summary of medications and prescriptions to manage their health post-treatment. Common medications such as anticoagulants (e.g., Warfarin, used for blood thinning) or antihypertensives (e.g., Lisinopril, for managing blood pressure) may be prescribed. Additionally, dosages (e.g., 5 mg of Lisinopril once daily) and administration routes (oral or injectable) should be clearly specified. Antibiotics like Amoxicillin might be indicated for infection prevention, typically prescribed for a duration of 7-14 days. Further, patients may receive instructions on potential side effects and interactions with existing medications, highlighting the importance of follow-up appointments at local clinics (such as Smithtown Medical Center). Proper documentation ensures continuity of care and aids in preventing medication errors, fostering a smoother recovery process for the patient.
Follow-Up Care Instructions
Following a hospital stay, clear follow-up care instructions are essential for a patient's continued recovery. Post-discharge appointments should be scheduled within one week at the outpatient clinic (specific location, e.g., City Medical Center, Suite 200). Medications prescribed, including dosage details and frequency, play a crucial role in recovery--ensure adherence to prevent complications. Dietary recommendations may include low-sodium or low-sugar guidelines tailored to specific health conditions, such as hypertension or diabetes. Activity limitations must be observed, with an emphasis on avoiding strenuous activities for at least two weeks. Monitoring for symptoms that warrant immediate medical attention, such as fever above 100.4 degrees Fahrenheit or unexplained pain, is critical. Easily accessible resources, including local support groups or rehabilitation services, can provide additional assistance.
Letter Template For Hospital Discharge Summary Samples
Letter template of hospital discharge summary for chronic illness management
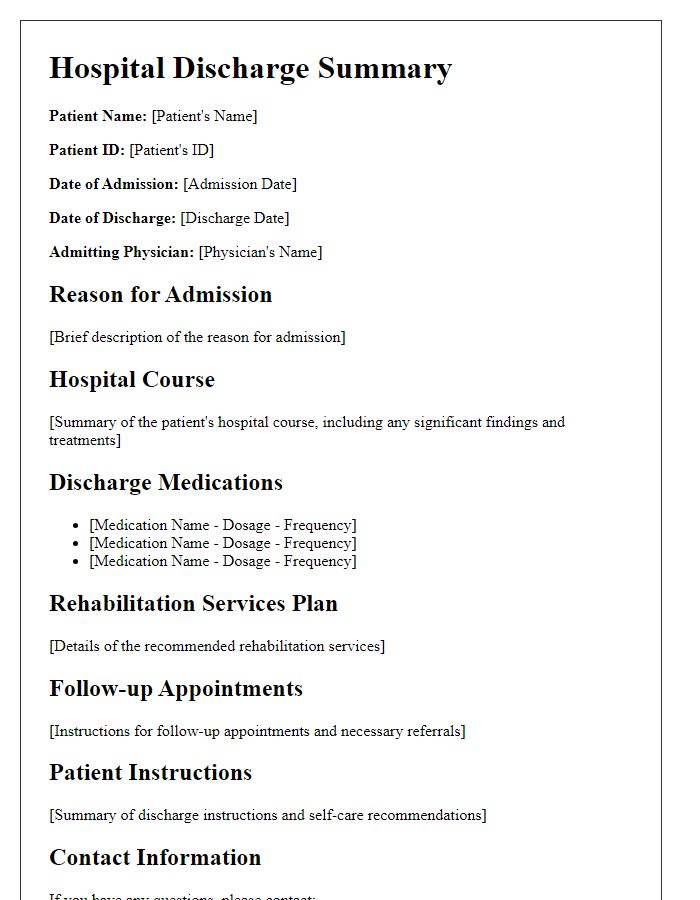
Letter template of hospital discharge summary for rehabilitation services
Letter template of hospital discharge summary for mental health treatment
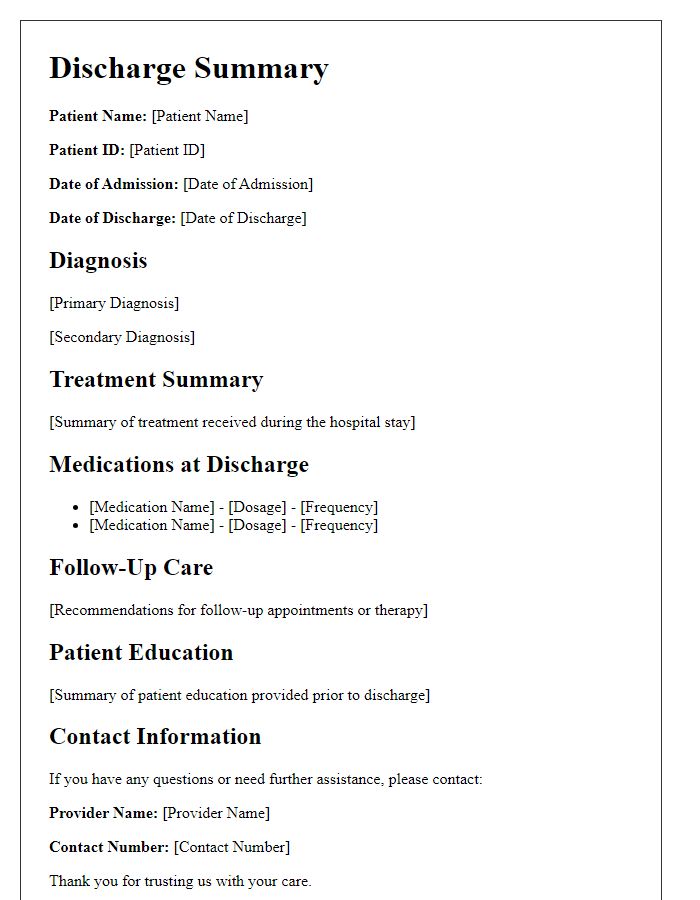
Letter template of hospital discharge summary for follow-up care instructions


Comments