Are you struggling to keep track of your patient's surgical history? Updating and organizing this vital information can be a daunting task, but it's essential for providing the best care possible. In this article, we will explore a simple and effective letter template designed specifically to streamline the process of documenting surgical histories. So, let's dive in and discover how you can enhance your patient recordsâread on for the full details!
Patient's Full Name and Identification
Patient's surgical history is essential for comprehensive medical assessments and treatment planning. Full name, including middle name and surname, ensures accurate identification within medical records. Patient identification number, a unique code assigned by healthcare facilities, aids in distinguishing individuals with similar names. Dates of previous surgeries provide a timeline for medical history. Type of surgeries, such as appendectomy, cholecystectomy, or orthopedic procedures, outlines significant past interventions. Complications during surgeries and recovery outcomes indicate potential risks for future procedures. Notable allergies and adverse reactions to anesthesia form critical information for anesthesiologists. Upcoming surgeries or procedures scheduled ensure continuity of care and facilitate thorough preoperative assessments.
Date and Type of Surgical Procedure
A patient's surgical history update typically includes crucial information such as the precise date of each surgical procedure and the specific type of surgery performed. For instance, a patient might have undergone an appendectomy on March 15, 2021, at City Hospital, a well-known medical facility in Springfield. Each entry documents the surgical intervention, aiding in ensuring comprehensive care and understanding potential risks for future medical decisions. Accurate and timely updates contribute to improved patient safety and collaborative healthcare planning among medical professionals.
Surgical Team and Institution Details
The surgical history update encapsulates crucial information regarding the patient's medical background. The surgical team (comprising board-certified surgeons, anesthesiologists, and surgical nurses) at the renowned Medical Center (established in 1985) ensures high standards of care. The institution boasts advanced surgical technologies and a comprehensive surgical recovery unit. Significant previous surgeries include an appendectomy and knee arthroscopy, both performed within the last five years. Documentation of any complications during these procedures, such as infections or delayed healing, enhances understanding of the patient's surgical resilience. Regular follow-ups (typically within one month post-surgery) allow for continued assessment of the patient's recovery trajectory, contributing to improved future surgical outcomes.
Pre-Operative and Post-Operative Condition Overview
Pre-operative assessments crucially evaluate a patient's surgical risk, focusing on medical history and current health status. Factors such as age (typically over 65 increases risk), pre-existing conditions (like diabetes, heart disease), and medications (anticoagulants influence bleeding risk) are meticulously examined. The surgical procedure, categorized under elective or emergency scenarios, dictates the necessary preparations. Anesthesia type, commonly general or regional, also plays a vital role in pre-operative planning. Post-operative recovery expectations are equally essential, detailing complications such as infections (can occur in about 3-4% of cases) or allergic reactions to anesthetics. Monitoring vital signs (heart rate, blood pressure) during recovery ensures early detection of potential issues. Rehabilitation protocols, tailored according to the specific surgical procedure, guide the patient's gradual return to normal activities while minimizing the risk of re-injury or complications. Explicit documentation remains a critical part of this process, ensuring effective communication among healthcare professionals involved in the surgical care continuum.
Relevant Test Results and Follow-Up Plan
Accurate surgical history updates are vital for patient care management within healthcare facilities. Relevant test results, including blood work and imaging studies such as X-rays or MRIs, provide essential information regarding patient health status prior to any surgical interventions. For instance, a complete blood count (CBC) may reveal anemia, impacting surgical decisions in procedures performed at leading hospitals like Johns Hopkins or Cleveland Clinic. Follow-up plans must outline specific timelines, such as scheduling follow-up consultations within two weeks post-surgery, to monitor recovery progress and address potential complications. Additionally, patients undergoing orthopedic surgery may require physical therapy sessions scheduled weekly to optimize rehabilitation. Clear communication of these critical details ensures continuity of care and improved patient outcomes.
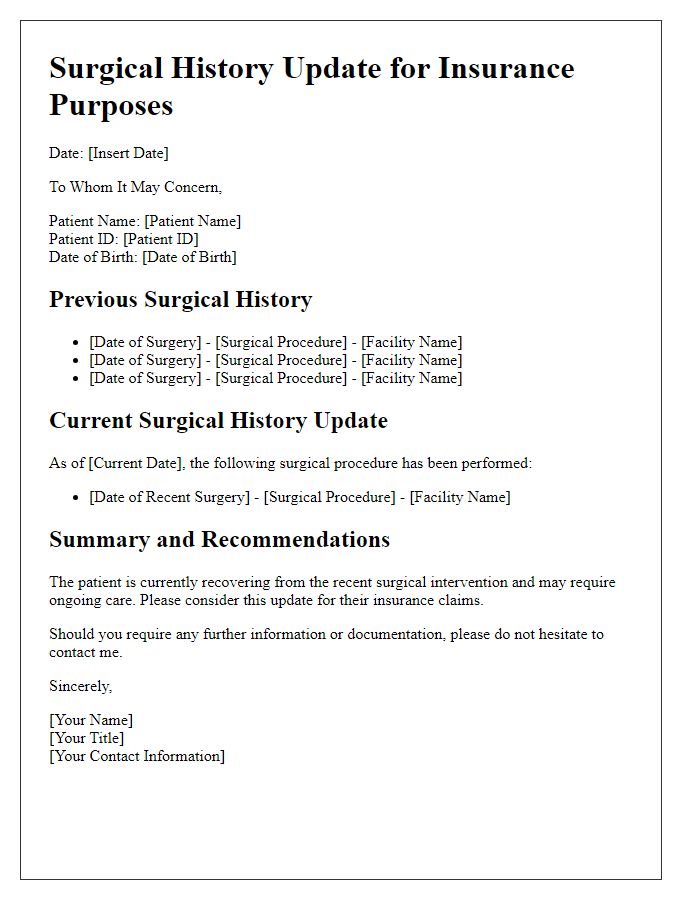
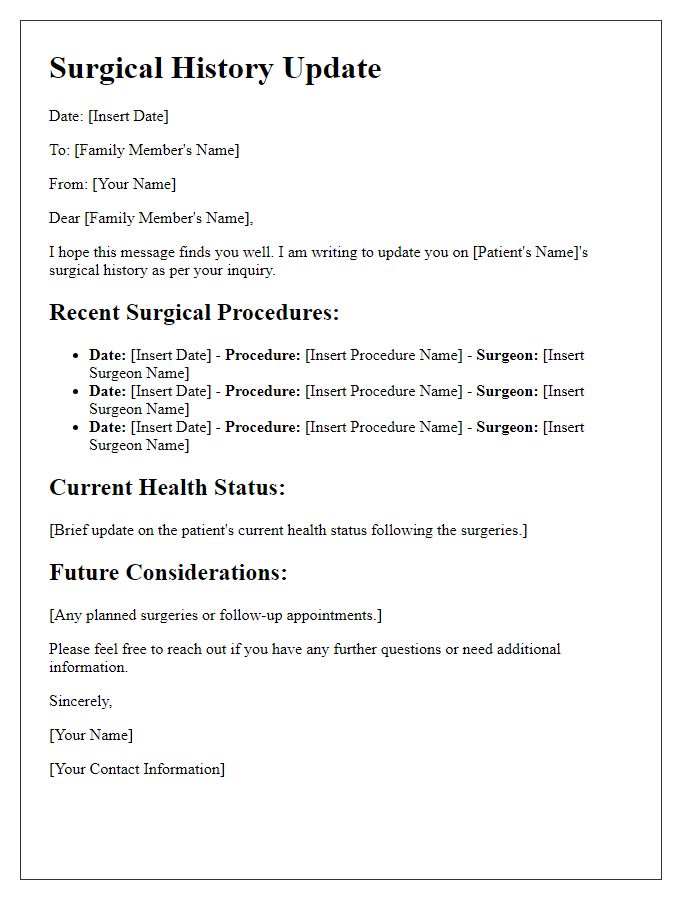
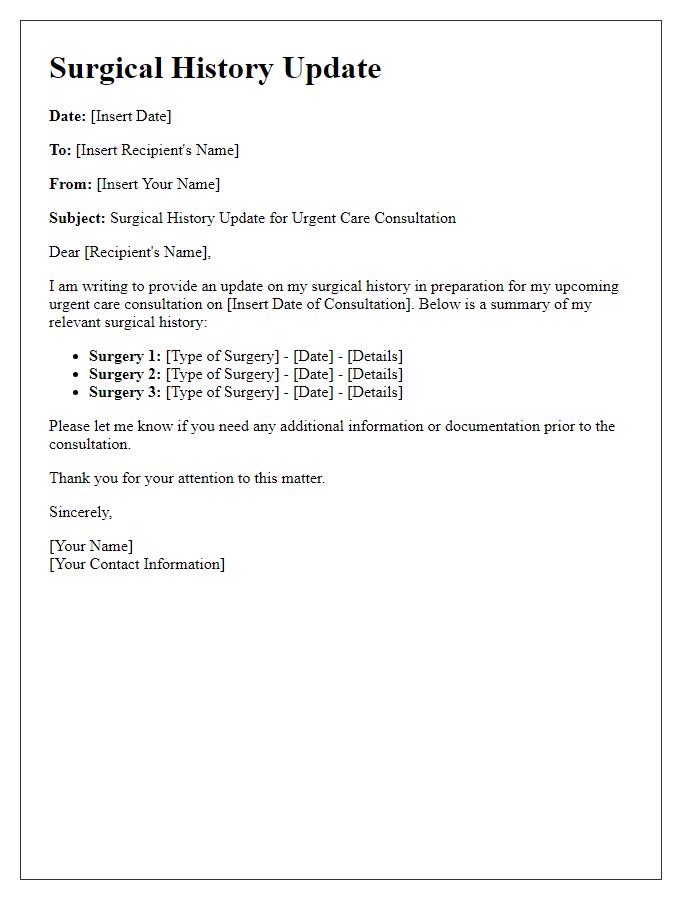
Letter Template For Patient'S Surgical History Update Samples
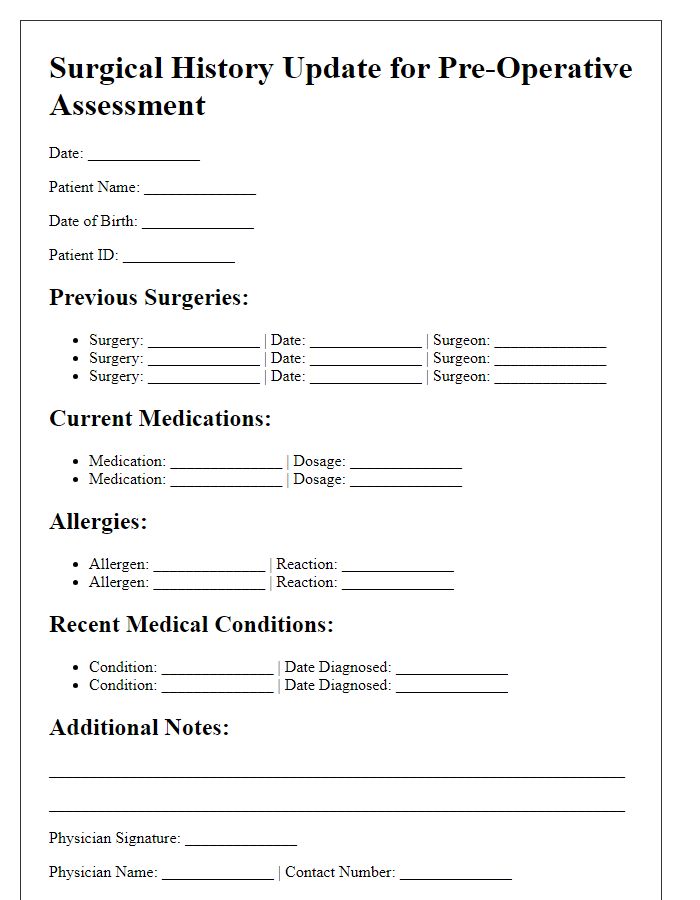
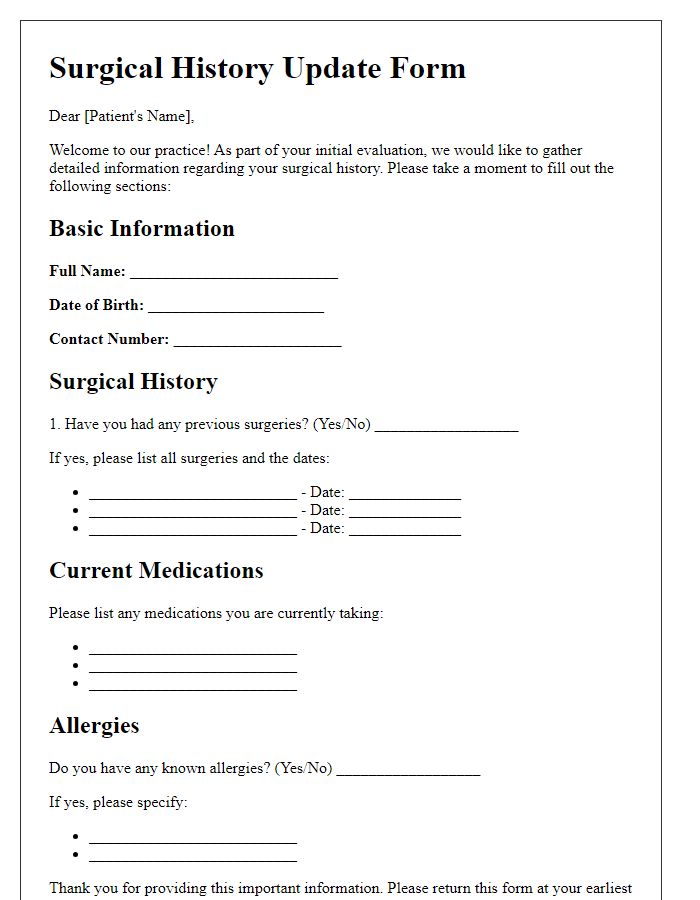
Letter template of surgical history update for pre-operative assessment.
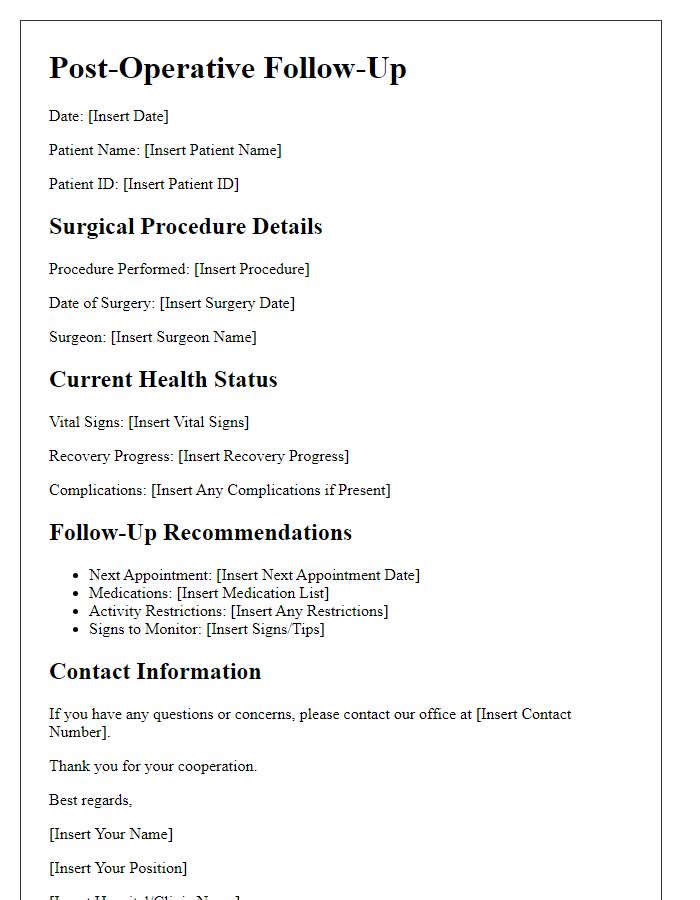
Letter template of surgical history update for post-operative follow-up.
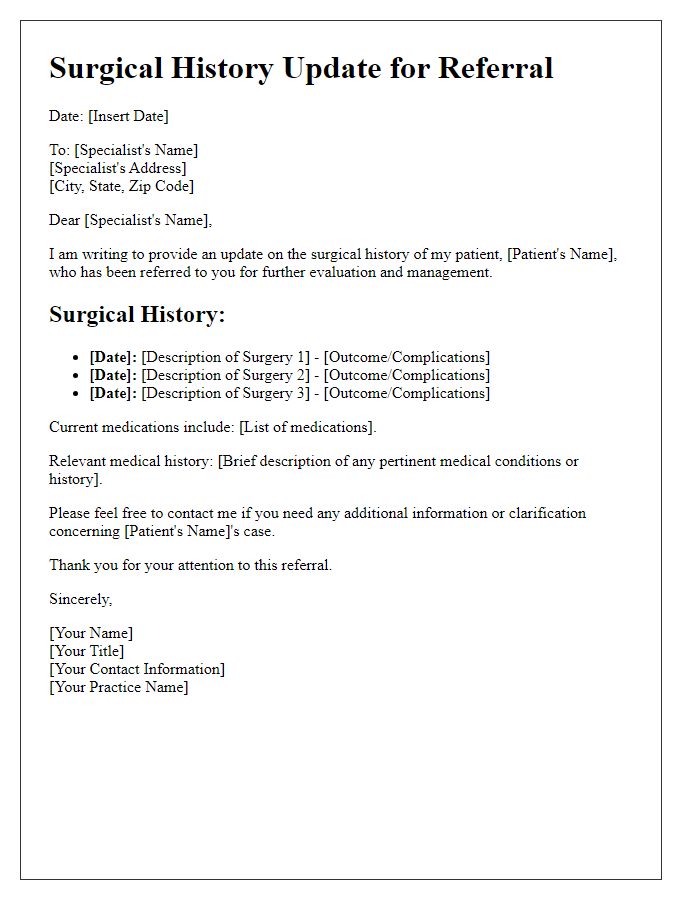
Letter template of surgical history update for referral to a specialist.
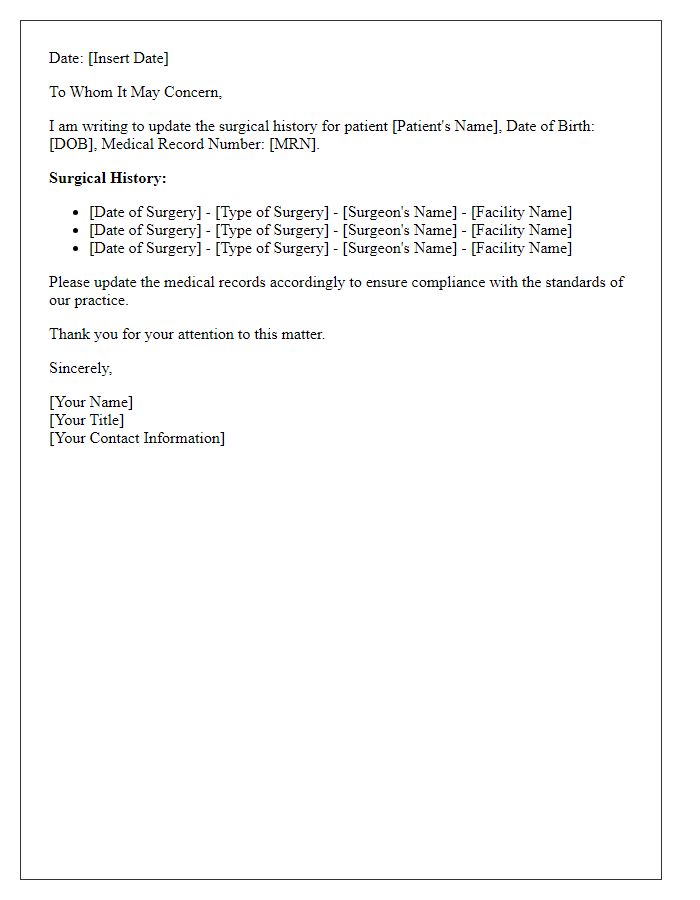
Letter template of surgical history update for medical records compliance.
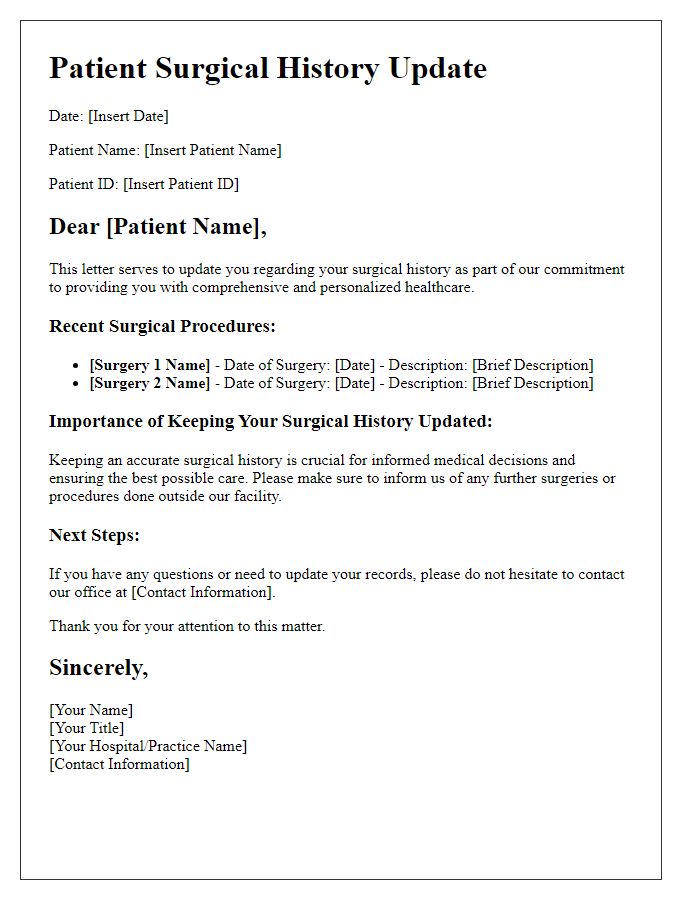
Letter template of surgical history update for patient education materials.
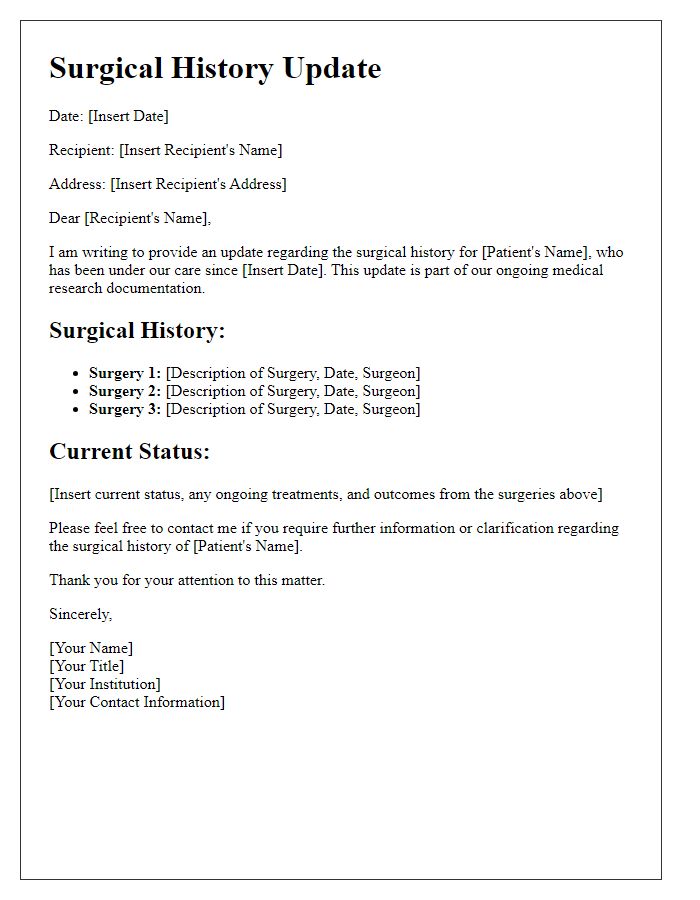
Letter template of surgical history update for medical research documentation.


Comments