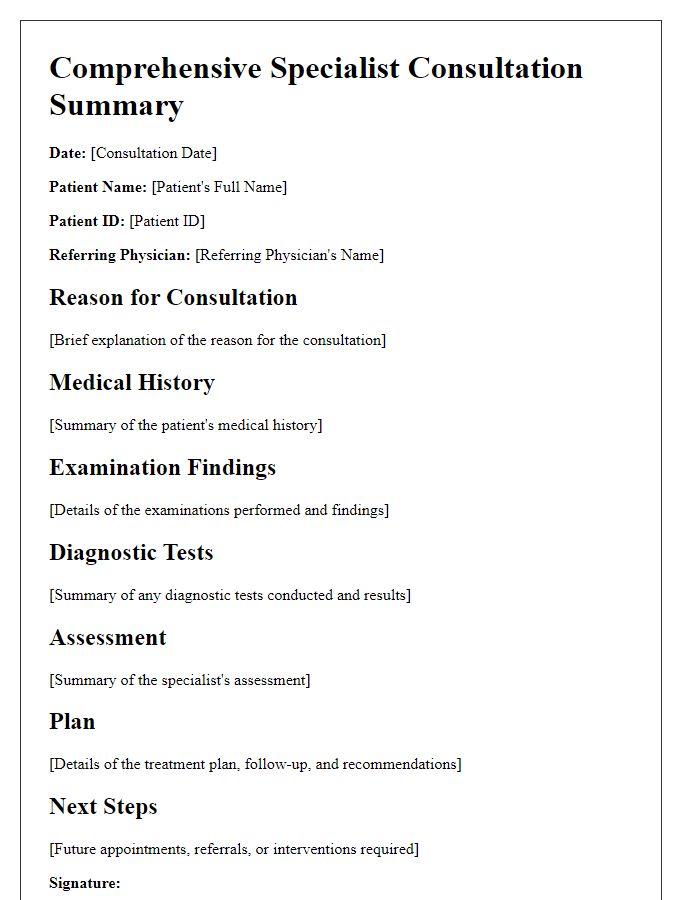
Are you looking for a streamlined way to document your specialist consultation reports? Creating a clear and concise letter template can make all the difference in effectively communicating essential findings and recommendations. This structured format not only helps in maintaining professionalism but also ensures that all critical information is easily accessible for future reference. Join me as we explore the essential components of an effective consultation report template that will enhance your communication skills and facilitate better patient care!

Patient Information: demographics and identifiers
Patient demographics encompass essential identifiers including full name, date of birth, and medical record number. For example, a patient named John Doe, born on January 15, 1985, may have a medical record number of 123456789. Other critical identifiers consist of gender, ethnicity, contact information, and insurance details. Gender plays a vital role in understanding specific health risks while ethnicity can influence genetic predispositions. Accurate contact information ensures effective communication regarding appointments and medical advice. Insurance details facilitate billing processes and access to specialized care. Collectively, these identifiers form a comprehensive profile that supports tailored healthcare solutions.
Referring Physician Details: contact and reference
The specialist consultation report serves as a critical document in the healthcare continuum, providing essential insights for patient care. Referring physician details must encompass key information, including the physician's full name, contact number, email address, and the practice or hospital affiliation. For example, the physician might be Dr. John Smith, reachable at (555) 123-4567, via email at john.smith@healthcare.com, associated with Sunshine Medical Center. Additional information such as the physician's specialty and the patient's referral reason aids in the context, ensuring effective communication between healthcare professionals. Accessing these details facilitates timely responses and improves patient management outcomes.
Clinical Summary: chief complaint, history, and examination
A specialist consultation report provides an essential overview of a patient's clinical status. The chief complaint, which is the primary reason for seeking medical attention, often varies, such as persistent abdominal pain or unusual fatigue. The history section encompasses significant medical events and symptoms experienced by the patient, which may include prior surgeries, chronic illnesses like diabetes, or familial health patterns. The examination section highlights the healthcare professional's findings during the physical assessment, detailing observations like abdominal tenderness, heart rate, or abnormal lab results critical for diagnosis. Comprehensive documentation enhances clinical understanding and informs subsequent treatment plans, optimizing patient outcomes.
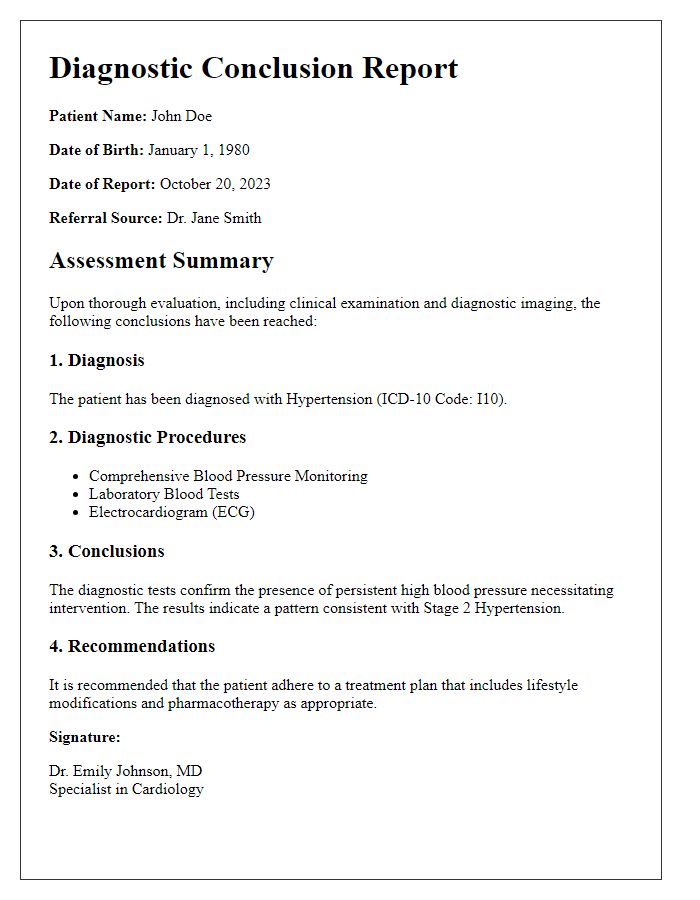
Diagnostic Findings: tests and results analysis
Diagnostic findings from the recent specialist consultation indicate significant insights into the patient's health condition. Comprehensive tests, including blood panels and imaging studies, reveal elevated levels of inflammatory markers, suggesting potential autoimmune disorders. Radiological examinations, such as MRI scans of the head, identify lesions consistent with demyelinating diseases like multiple sclerosis. Furthermore, the analysis of genetic tests highlights the presence of specific gene mutations associated with increased susceptibility to hereditary conditions. These diagnostic results will guide the treatment plan and require further monitoring and follow-up consultations to assess the progression of the identified conditions.
Recommendations: management plan and follow-up steps
The specialist consultation report outlines a comprehensive management plan tailored for the patient, emphasizing key recommendations for ongoing care. Initial recommendations include scheduling regular follow-up appointments every three months for monitoring progress and adjusting treatment as needed. Medication adherence is vital, suggesting a daily regimen of prescribed therapies to optimize health outcomes. Lifestyle modifications, such as a balanced diet rich in antioxidants and regular physical activity (at least 150 minutes per week), are encouraged to enhance overall well-being. Psychological support, including cognitive-behavioral therapy sessions, is advised to address any associated mental health concerns. Additionally, a referral to a nutritionist specializing in chronic conditions may provide further personalized dietary guidance. Lastly, utilizing patient management software for tracking health metrics and reminders for medication intake can significantly enhance patient engagement and adherence to the management plan.


Comments