When it comes to caring for our beloved seniors, having the right guidance is crucial for ensuring their comfort and well-being. Understanding specific geriatric care instructions not only eases the burden but also enhances the quality of life for older adults. This article will explore essential tips and best practices that anyone can implement with confidence, whether you're a family member or a professional caregiver. So, grab a cozy seat and get ready to dive into the world of senior care that truly makes a difference!
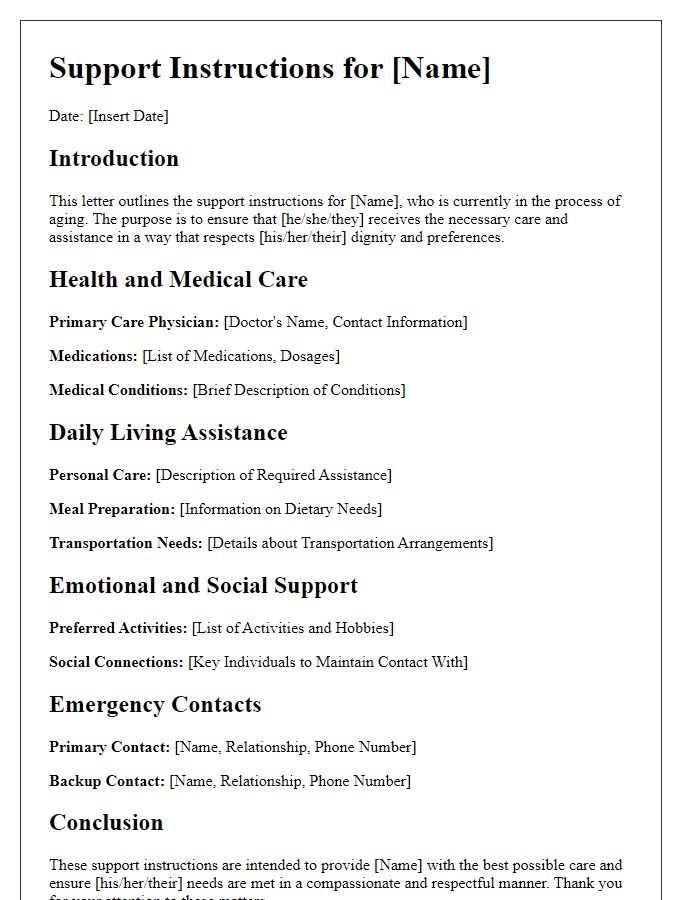
Personalized Patient Information
Personalized geriatric care instructions must focus on individual patient needs, health conditions, and lifestyle factors. For instance, managing chronic conditions such as diabetes or hypertension requires medication adherence, regular monitoring of blood sugar or blood pressure levels, and dietary adjustments tailored to the patient's preferences and nutritional requirements. Physical activity is essential; activities like walking or chair exercises can enhance mobility and reduce fall risks. Social engagement is crucial for mental well-being, suggesting participation in community activities or family gatherings. Cognitive exercises, including puzzles or reading, can promote mental agility. Medication management should include a comprehensive list of prescriptions, dosage, and timing to prevent confusion. Home safety measures, such as removing tripping hazards and ensuring proper lighting, can enhance patient safety. Regular follow-up appointments with healthcare providers should be scheduled to monitor health status and adjust care plans as necessary. Each instruction ensures a holistic approach to improving quality of life for elderly patients.
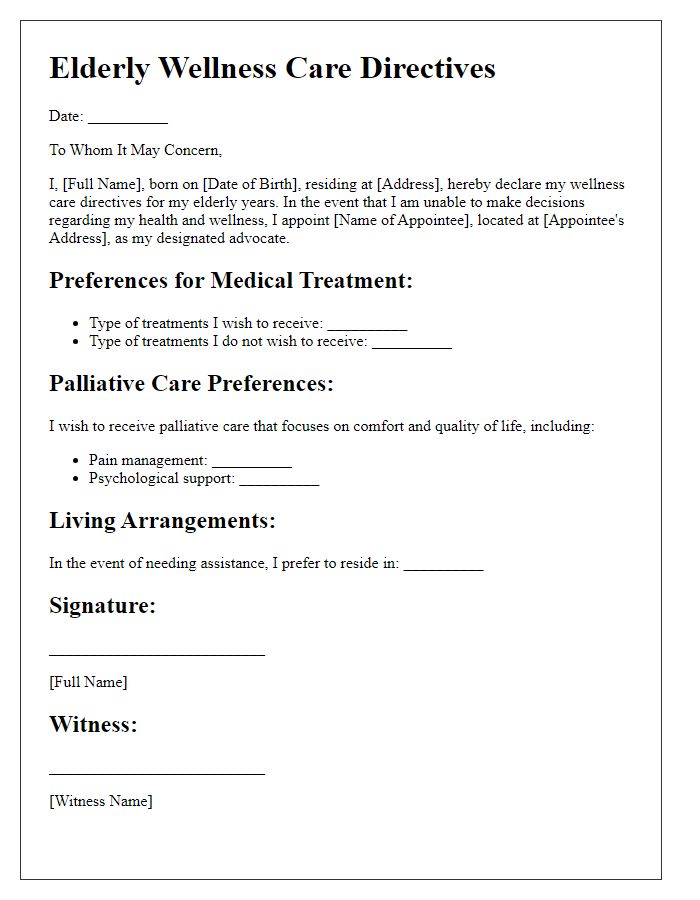
Medication and Dosage Details
Geriatric patients often require careful management of medications to ensure safety and effectiveness. Common medications prescribed for older adults include antihypertensives, such as Lisinopril (usually 10-40 mg daily), and statins, like Atorvastatin (typically 10-80 mg daily). It is crucial to monitor kidney function and electrolyte levels, especially in patients over 65 years old. Dosage adjustments may be necessary due to renal impairment, which can significantly impact drug clearance. Additionally, side effects of medications, such as dizziness or confusion, should be closely observed as they can exacerbate conditions like falls in elderly individuals. Regular medication reviews with healthcare providers at facilities such as clinics or nursing homes can help optimize therapeutic regimens and minimize adverse effects.
Daily Routine and Activities
In geriatric care, establishing a structured daily routine is essential for promoting the well-being and independence of elderly individuals. Morning activities should include gentle stretches to enhance flexibility and circulation. A nutritious breakfast, rich in fiber and protein, is crucial for maintaining energy levels throughout the day. Engaging in cognitive exercises, like puzzles or reading, stimulates mental acuity and memory retention. Social interactions, whether through family visits or community programs, provide emotional support and reduce feelings of isolation. Afternoon activities may involve light physical exercises, such as walking in a local park or participating in chair yoga, to promote mobility and balance. Dinner should prioritize balanced nutrition, focusing on heart-healthy options. Lastly, incorporating relaxation techniques, such as meditation or listening to calming music, during the evening promotes restful sleep, vital for overall health.
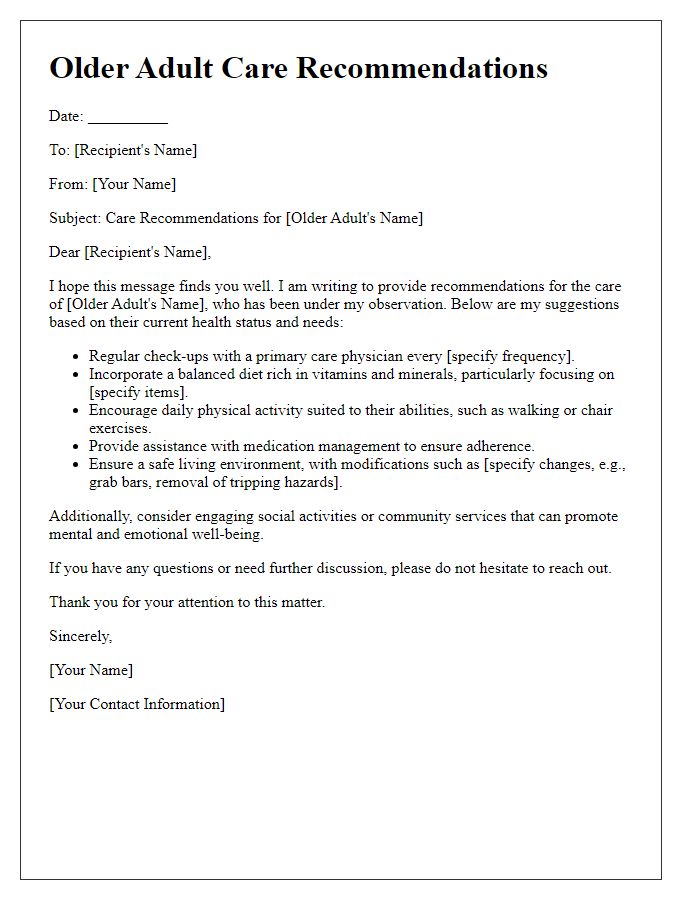
Emergency Contacts and Protocols
In a geriatric care setting, maintaining a clear and accessible list of emergency contacts and protocols is essential for ensuring the safety and well-being of elderly patients. Emergency contacts should include primary caregivers, family members, and medical professionals, such as the attending physician at the local hospital (for instance, St. Mary's Medical Center) as well as specialists involved in the patient's care (like a cardiologist or geriatrician). Protocols might cover actions to take in various emergency scenarios, ranging from falls leading to potential fractures to sudden deterioration in health (like chest pain signaling a heart attack). It's imperative to have the specific phone numbers readily available, with clear instructions on how to reach emergency services (such as 911 in the United States) and local urgent care facilities. Furthermore, detailed protocols regarding medication administration during crises (including the use of EpiPens for allergic reactions) should be readily accessible, ensuring that caregivers and family members are well-prepared to act decisively in critical situations.
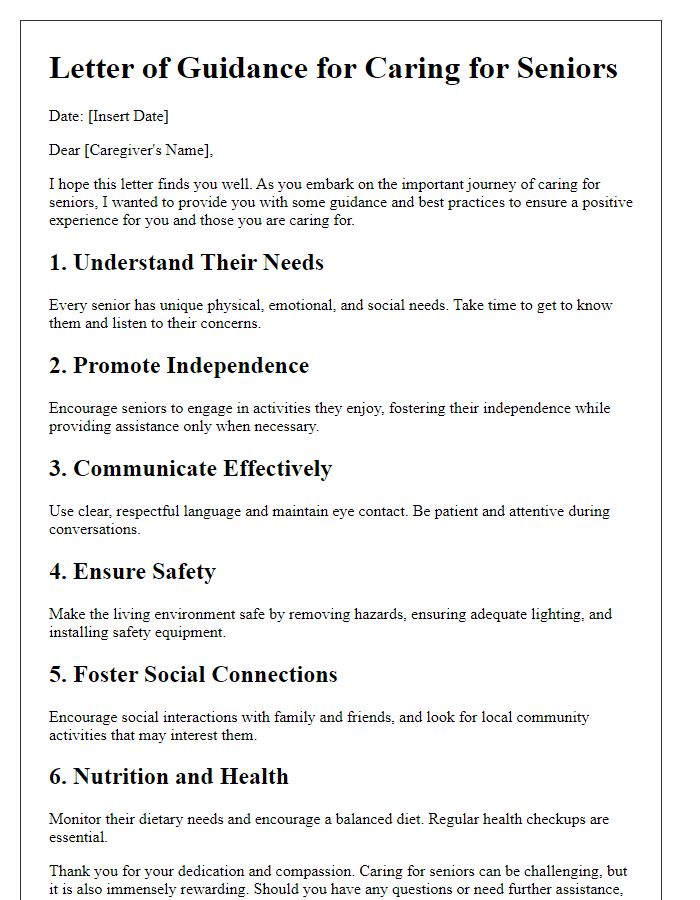
Caregiver Responsibilities and Guidelines
Geriatric care for elderly individuals requires attentive responsibilities and clear guidelines to ensure their comfort and health. Caregiver duties include administering medications (often multiple prescription types), assisting with daily activities (such as bathing and grooming), and monitoring vital signs (blood pressure, heart rate) to detect potential health issues. Proper nutrition (balanced diets with specific dietary restrictions) must be emphasized, along with meal preparation methods that accommodate individual health conditions (diabetes, hypertension). Additionally, caregivers should provide companionship to address mental well-being, recognizing signs of isolation or depression. Maintaining a safe environment (removing tripping hazards, installing grab bars) is essential to prevent falls, a common concern for seniors aged 65 and older. Regular communication with healthcare providers (physicians, specialists) is necessary to adjust care plans as needed, ensuring ongoing health assessments and interventions. Lastly, documentation of daily activities, changes in behavior, or health status is crucial for maintaining continuity of care and for any future evaluations.


Comments