Are you ready to take charge of your healthcare decisions, even when you might not be able to voice them yourself? Creating an advanced healthcare directive can empower you and your loved ones to navigate medical situations with clarity and confidence. This important document ensures that your wishes regarding treatment and care are documented and respected, providing peace of mind in challenging times. Dive into this article to learn how to craft an effective advanced healthcare directive that reflects your values and needs!
Personal Information
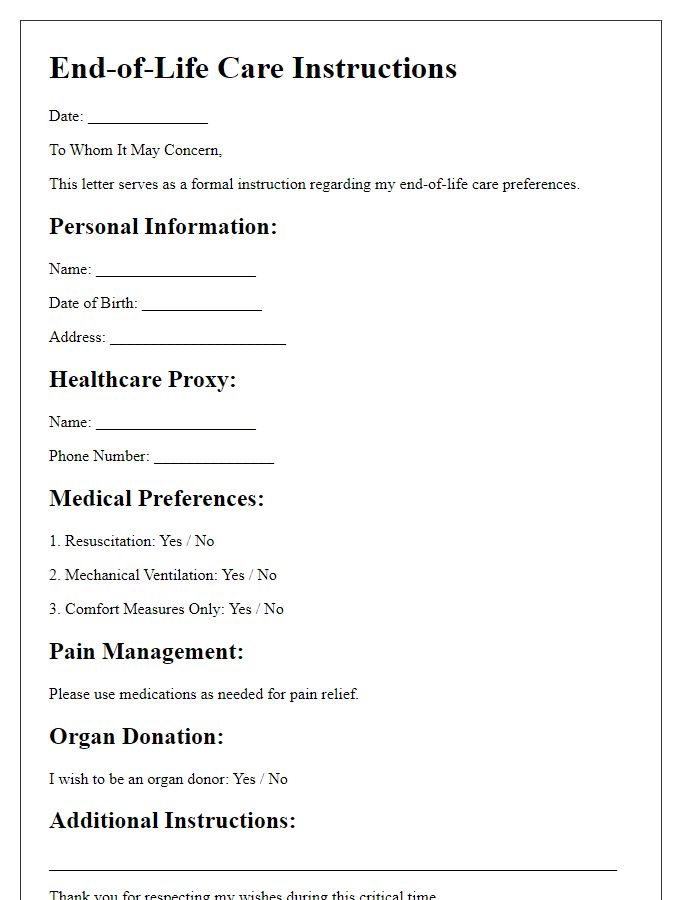
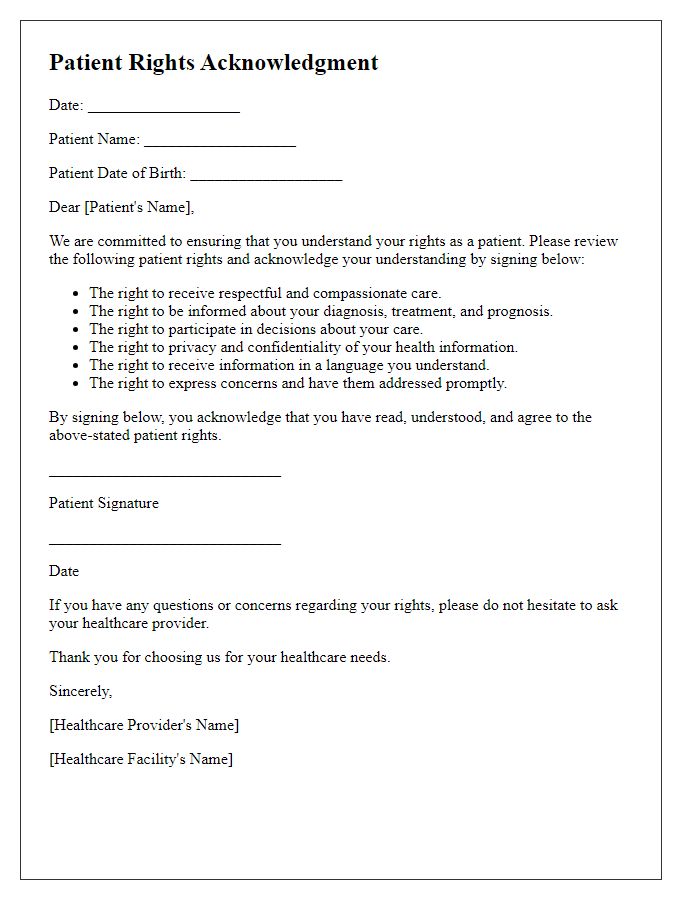
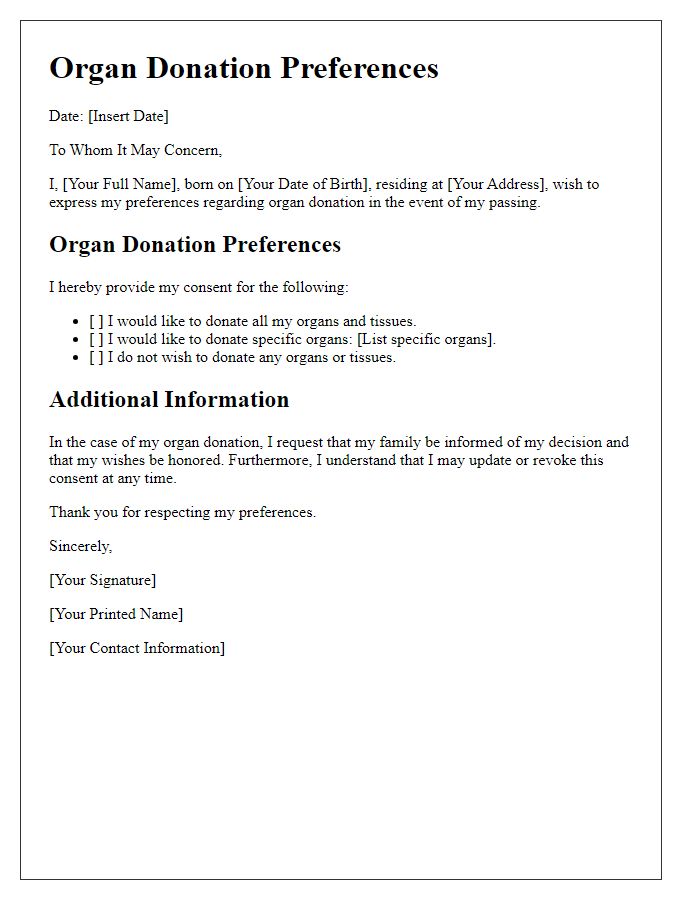
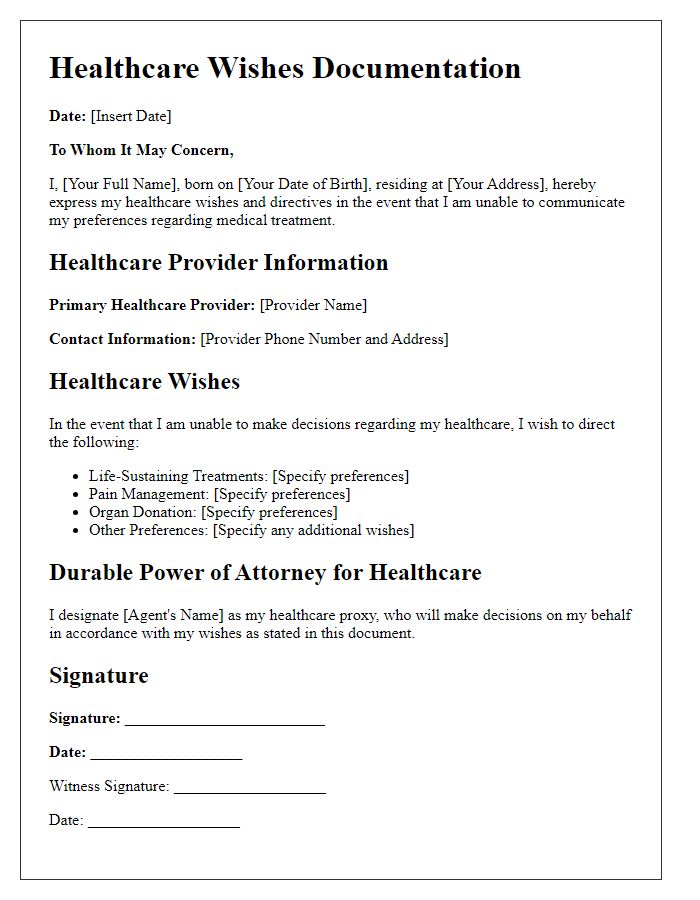
An advanced healthcare directive provides critical guidance for medical decisions when individuals cannot communicate their preferences. Key components include the designation of a healthcare proxy, typically a trusted family member or friend, to make choices on behalf of the individual. Important personal information includes the full name, date of birth, and contact information of the individual, ensuring medical professionals easily identify the directive's owner. Additionally, specifying any allergies and current medical conditions enhances the background context for healthcare providers, facilitating informed decision-making. Furthermore, including instructions regarding life-sustaining treatments, organ donation preferences, and pain management ensures clarity in accordance with the individual's values and wishes during critical healthcare situations.
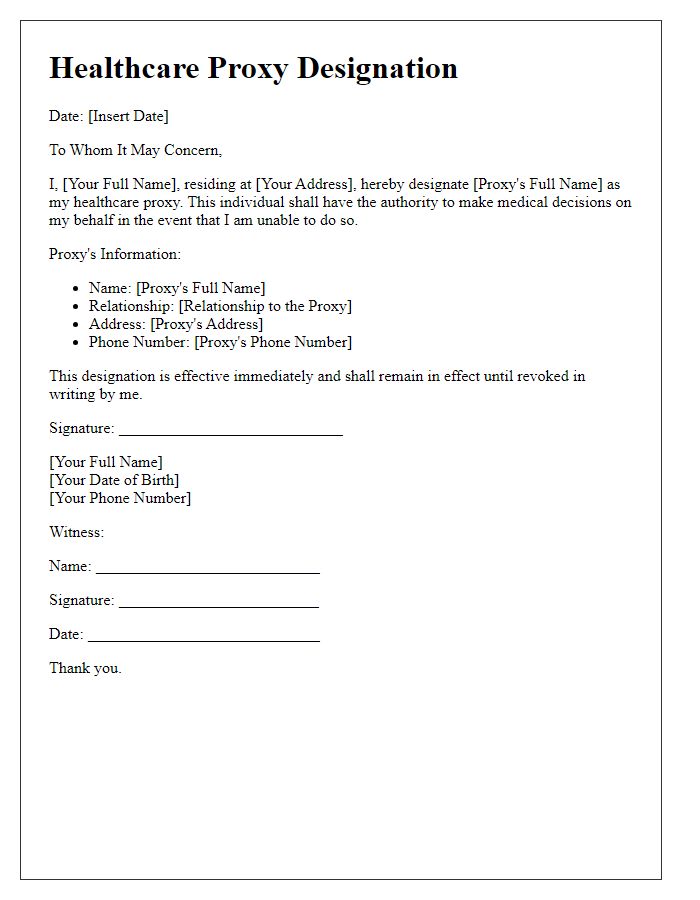
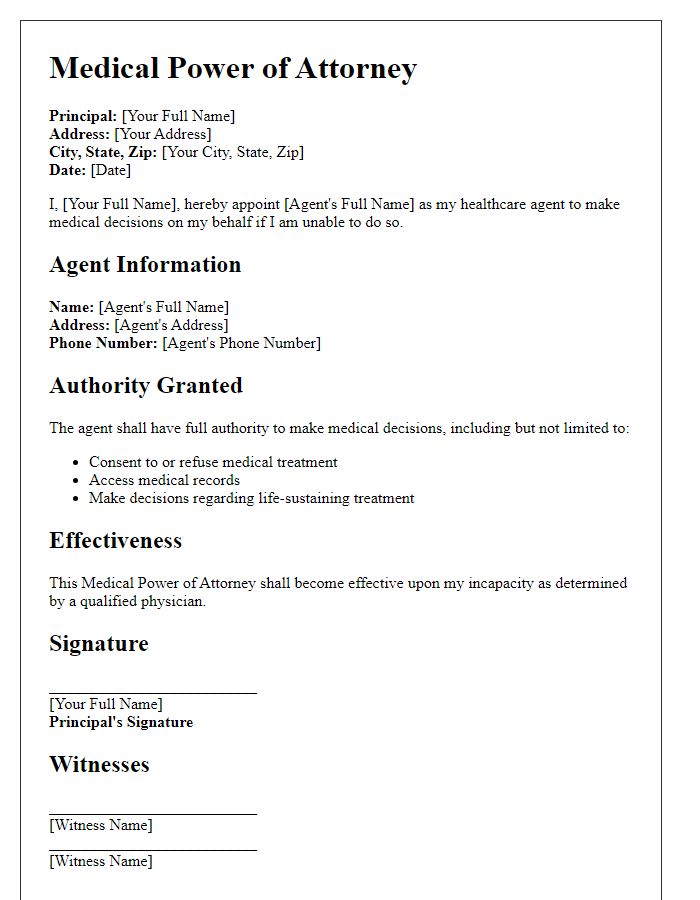
Healthcare Agent Identification
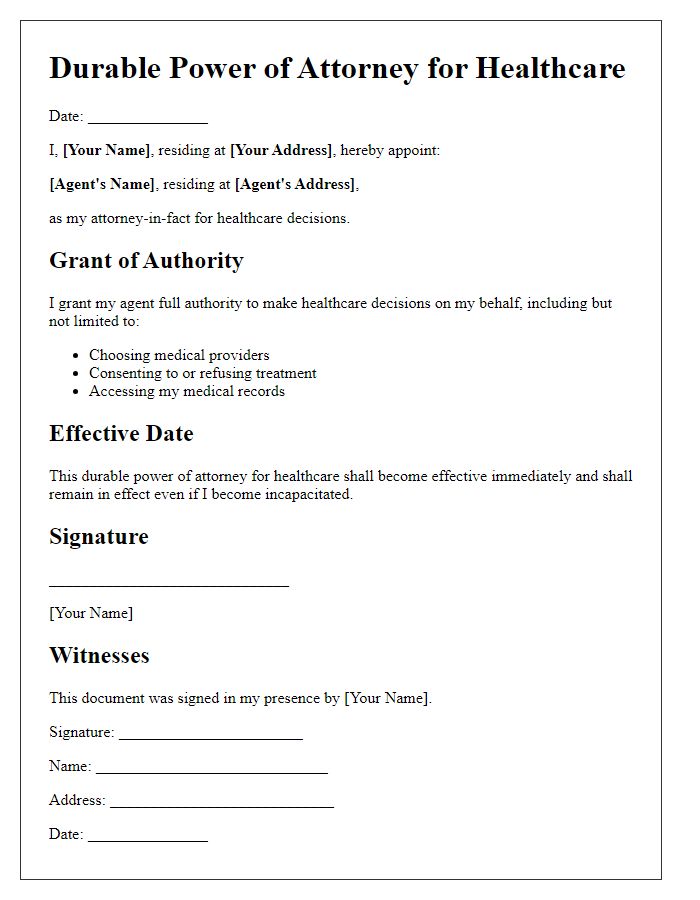
An advanced healthcare directive letter template serves as a crucial document in the planning of medical care preferences when the individual is unable to communicate decisions. This template includes a dedicated section for Healthcare Agent Identification, which designates a trusted person, often a family member or close friend, to make healthcare decisions on behalf of the individual. Properly identifying the healthcare agent ensures that this representative understands the individual's values and wishes regarding treatment options, end-of-life care, and medical procedures. Clarity in this designation can prevent conflicts or confusion during critical moments, allowing for choices that align with the individual's beliefs and desires for dignity in healthcare.
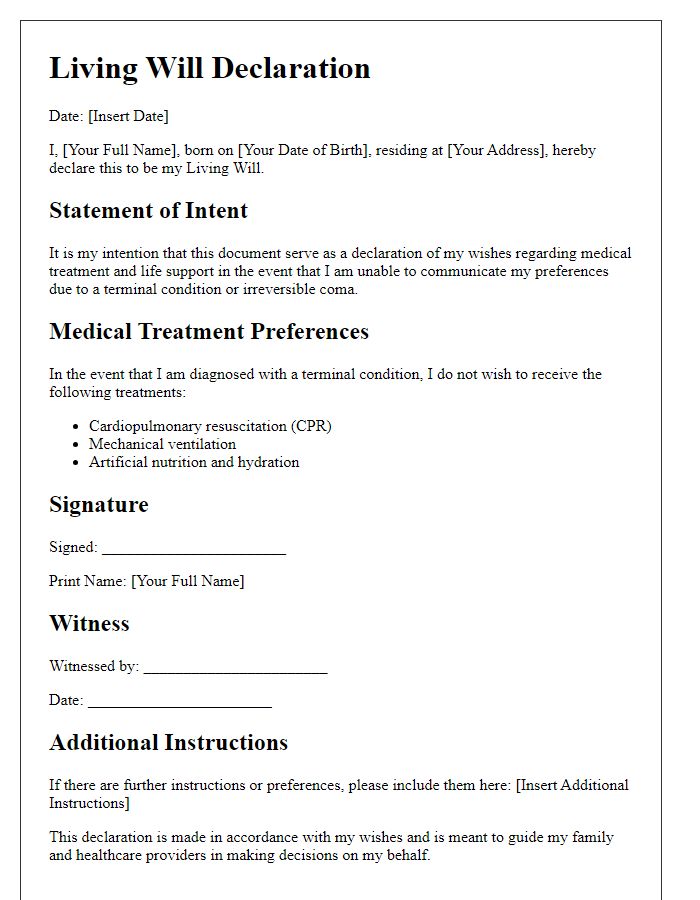
Treatment Preferences
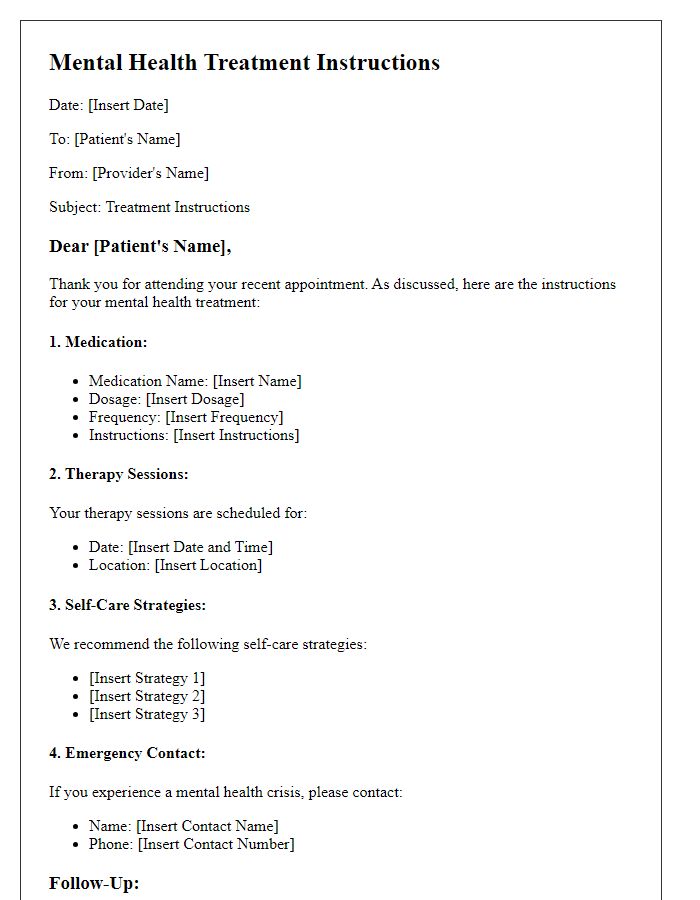
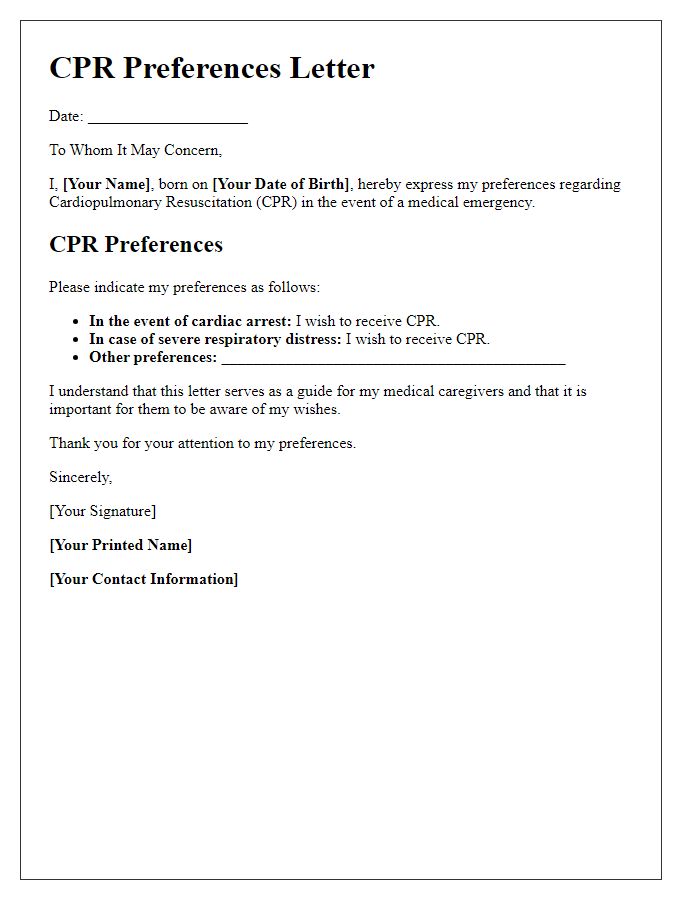
An advanced healthcare directive outlines treatment preferences for individuals, ensuring their healthcare wishes are respected in medical situations. Patients must specify desired interventions in cases of terminal illness or irreversible conditions. Common preferences include the use of life-sustaining measures, such as ventilators and feeding tubes, as well as resuscitation protocols like Do Not Resuscitate (DNR) orders. Patients may also indicate their preferences for pain management and palliative care options, emphasizing comfort and quality of life. Healthcare providers in hospitals or hospice settings must adhere to these directives, ensuring that the patient's values and choices guide their care.
Legal and Financial Considerations
An advanced healthcare directive template serves as a crucial legal document, outlining an individual's preferences regarding medical treatment and decision-making during incapacitation. Essential elements include appointing a healthcare proxy, ensuring an appointed person can make critical choices about life-sustaining measures. Legal considerations address state-specific regulations and necessary signatures for validity. Financial implications, such as the potential costs of prolonged care and the impact on estate planning, demand careful evaluation. Utilizing a reliable template can streamline the process, ensuring comprehensive coverage of health preferences while minimizing future disputes among family members.
Signatures and Witnesses
An advanced healthcare directive often requires careful consideration regarding the signatories and witnesses involved in the process. The directive document typically must include the signatures of the person making the directive, known as the principal, alongside their full name and date. Two witnesses, who are not related to the principal, should provide their signatures, names, and contact details. Each witness must confirm that the principal appears to be of sound mind and voluntarily signing the document. Additionally, some jurisdictions may require a notary public to validate the directive, adding an extra layer of legal assurance. Witnessing should occur in the presence of the principal to uphold the integrity of the document.



Comments