Are you considering participating in a clinical trial but unsure where to begin? Navigating the world of clinical research can be daunting, but it's an essential step toward advancing medical science and improving patient care. By participating, you not only contribute to groundbreaking discoveries but also gain access to cutting-edge treatments and expert medical support. Ready to learn more about how you can get involved and make a difference?
Patient Information and Privacy
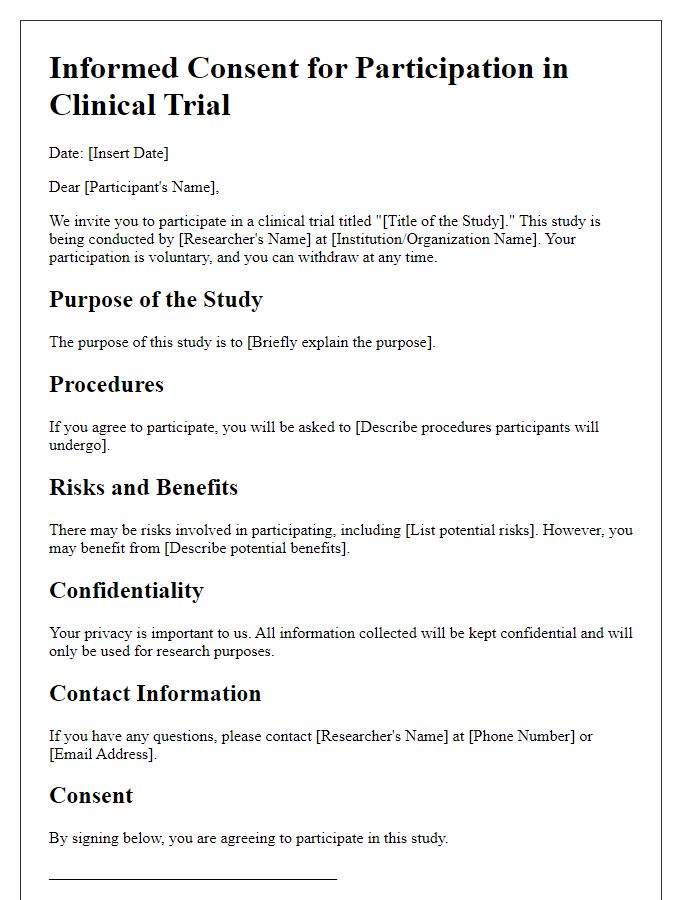
Patient participation in clinical trials, particularly for investigating innovative therapies, requires comprehensive understanding of patient information and privacy protocols. Informed consent documents outline essential details, including study purposes, methodologies, and potential risks or benefits associated with participation, as mandated by ethical standards established by regulatory bodies such as the FDA (Food and Drug Administration). Personal health information (PHI) is safeguarded under regulations such as HIPAA (Health Insurance Portability and Accountability Act), ensuring confidentiality throughout the trial process. Researchers and staff must adhere to strict data protection measures to prevent unauthorized access, and any reporting of study results must be done in aggregate form without revealing individual identities. Regular audits (e.g., quarterly or biannual) are typically conducted to ensure compliance with privacy standards, fostering a secure environment for participant data.
Study Purpose and Design
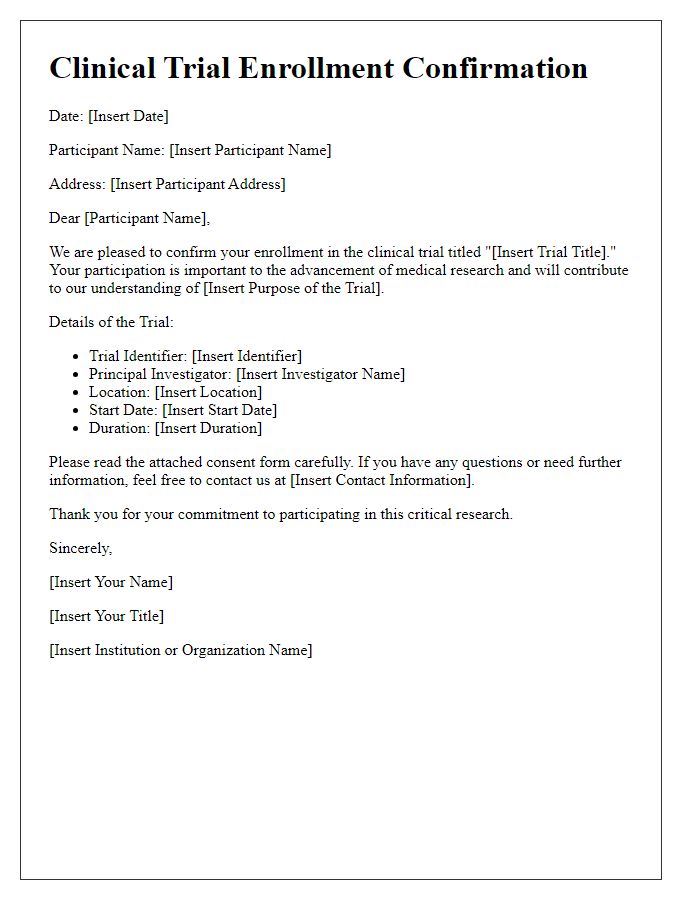
The clinical trial study aims to evaluate the efficacy of the experimental drug, Zymorax, in treating Stage II melanoma among adults aged 18 to 65. The trial will be conducted across five major oncology centers in the United States, including the Mayo Clinic in Rochester, Minnesota, and MD Anderson Cancer Center in Houston, Texas. Participants will be randomly assigned to receive either Zymorax or a placebo in a double-blind design, ensuring neither the participants nor the researchers are aware of the assignments. This approach helps eliminate bias in assessing the drug's effectiveness. The study will span 24 months, with participants undergoing regular health assessments, blood tests, and imaging scans to monitor tumor progression and drug response. Safety will be measured through the tracking of adverse events, aiming for a comprehensive understanding of the drug's impact on patient health.
Risks and Benefits
Participating in a clinical trial involves potential risks and benefits that must be carefully considered. Risks may include common side effects associated with experimental treatments, which can vary depending on the specific drug or procedure involved, such as nausea, fatigue, or allergic reactions. Serious adverse events, though less common, can also occur, with occurrences ranging from 3% to 10% in some studies, necessitating close monitoring of participants. Benefits of participation often include access to new therapies not yet available to the general public, which may offer greater efficacy than standard treatments. Additionally, participants may contribute to important medical advancements, potentially benefiting future patients with similar conditions. Clinical trials, particularly those registered at reputable institutions like the National Institutes of Health (NIH), ensure ethical standards and participant safety through oversight and informed consent processes. Engagement in these studies can also provide participants with access to expert medical care and continuous health assessments during the trial duration.
Consent and Voluntary Participation
Informed consent in clinical trials ensures the ethical treatment of participants, requiring clear communication about the study's purpose, procedures, risks, and benefits. Potential participants, often recruited from hospitals or research centers, like Johns Hopkins or Mayo Clinic, must understand that participation is voluntary, with the right to withdraw at any time without penalty. Researchers must provide detailed information about the trial type, including Phase I (safety testing) or Phase III (efficacy evaluation) processes. This transparency allows individuals to make informed decisions, balancing personal health needs and contributing to medical advancements. Documentation of consent, a crucial legal and ethical requirement, often involves signing a consent form reiterating the participant's understanding and agreement to participate.
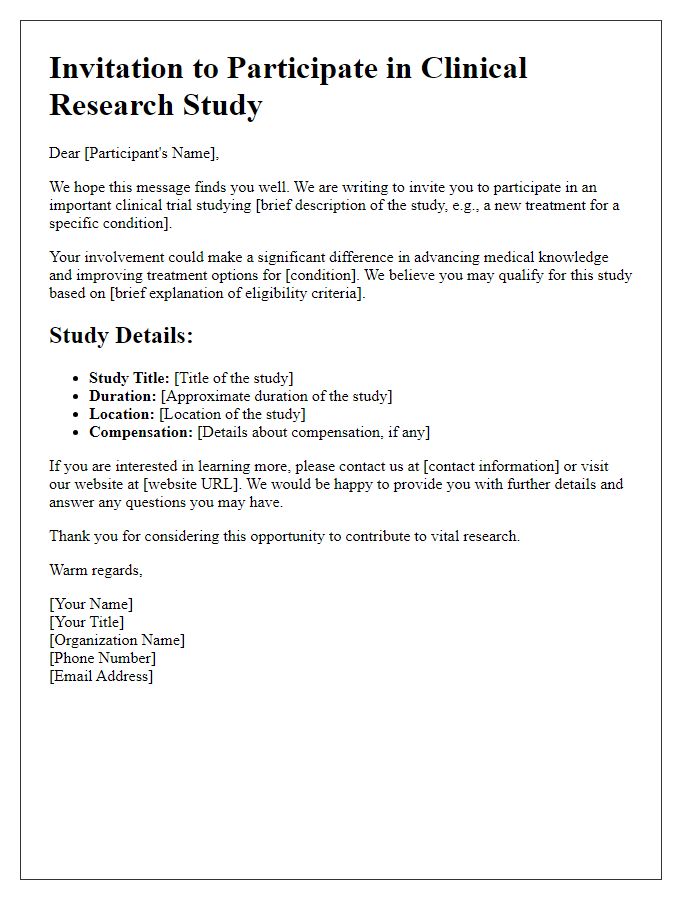
Contact Information and Support
Contacting participants in clinical trials requires careful organization and attention to detail. Essential components include the trials' protocol number (e.g., 2023CT001), the principal investigator's name (such as Dr. Jane Smith), and the research institution's address (e.g., New York University Medical Center). Provide a dedicated phone line, like (555) 123-4567, for questions and support, ensuring prompt communication between the team and participants. An email contact, such as info@clinicaltrials.org, can facilitate quick dissemination of information related to the trial schedule and updates. Participant support services should also highlight resources, including 24/7 hotlines or patient advocates who assist with any concerns or queries throughout the clinical trial process.


Comments